
What is HEDIS and what does it mean to you?
You’ve probably heard of the acronym HEDIS – but what does it stand for and what does it mean to you? The Healthcare Effectiveness Data and Information Set – HEDIS — was created by the National Committee for Quality Assurance (NCQA) to measure the clinical quality performance of health plans.
What is HEDIS and why should I Care?
What is HEDIS and why is it important? HEDIS refers to Healthcare Effectiveness Data and Information Set, standardized set of performance measures developed by the National Committee for Quality Assurance (NCQA www.ncqa.org) to evaluate consumer health care. HEDIS is a tool used by more than 90 percent
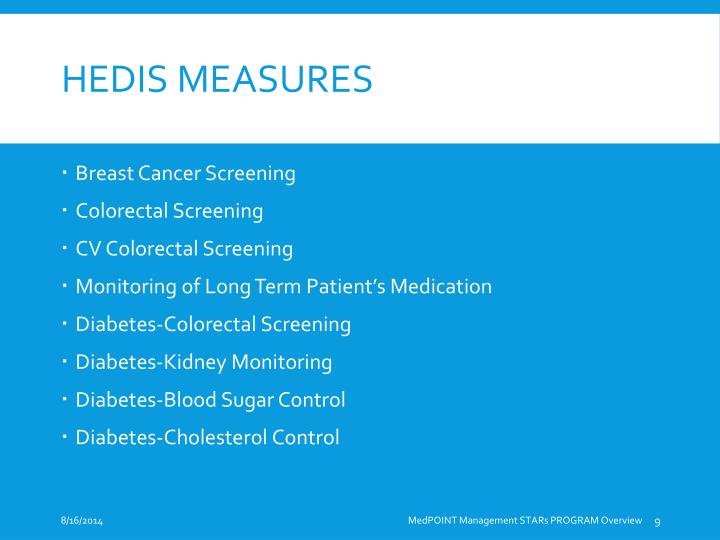
What are the HEDIS quality measures?
What is HEDIS ®?
- HEDIS stands for Healthcare Effectiveness Data and Information Set.
- NCQA Specifications standardize performance to evaluate and compare health plan performance and quality.
- Required for ongoing NCQA Health Plan accreditation.
What you can do to improve HEDIS HEDIS resources available?
You can also enter the keyword “Toolkits” in the search field of the provider portal to get to this HEDIS information. Once you’re there, choose “ Improving HEDIS Scores ,” which will give you a drop-down list of the HEDIS measures and corresponding resource tools.
What are the HEDIS measures for 2022?
For MY 2022, HEDIS added three new measures, retired three measures/indicators and changed seven existing measures....Additions to HEDIS in 2022Advance Care Planning. ... Antibiotic Utilization for Respiratory Conditions. ... Deprescribing of Benzodiazepines in Older Adults.
What are the 5 domains of HEDIS?
HEDIS measures clinical quality and customer service, requiring standardized reporting under 5 domains of care:Effectiveness of Care.Access/Availability of Care.Experience of Care.Utilization and Risk Adjusted Utilization.Health Plan Descriptive Information.Measures collected using Electronic clinical data Systems.
How is HEDIS data used by Medicare?
The HEDIS PLD data are submitted annually by Medicare Advantage (MA) Organizations, Cost Plans, and Demonstration Plans and contribute to the assignment of CMS Star Ratings for MA plans.
What are the 6 domains of care for HEDIS performance measures?
An outlined set of performance measures across 6 domains of care is required for reporting: Effectiveness of Care, Access/Availability of Care, Experience of Care, Utilization and Risk-Adjusted Utilization, Health Plan Descriptive Information, and Measures Collected Using Electronic Data Systems.
What are examples of HEDIS measures?
Examples of HEDIS® measures are Comprehensive Diabetes Care, Childhood Immunizations, yearly Well Child Exams for Children Ages 3-6 and yearly Adolescent Well Care Exams.
What does HEDIS mean in healthcare?
Healthcare Effectiveness Data and Information SetNCQA established Healthcare Effectiveness Data and Information Set (HEDIS) measures specifically for SNPs. HEDIS is a comprehensive set of standardized performance measures designed to provide purchasers and consumers with the information they need for reliable comparison of health plan performance.
Who is required to report HEDIS measures?
All SNP and MMP PBPs must report the HEDIS measures in Table 3. If a contract has multiple qualifying PBPs, then each qualifying PBP in the contract must report the measures in Table 3 in a separate submission. MMPs and contracts with SNP PBPs do not have to report any additional PLD files.
Who uses HEDIS data?
HEDIS (pronounced he´-dus) stands for Healthcare Effectiveness Data and Information Set. Employers and individuals use HEDIS to measure the quality of health plans. HEDIS measures how well health plans give service and care to their members.
How does HEDIS impact patient care?
Benefits of HEDIS Works to improve patient outcomes and decrease the cost of care through preventative services. May provide beneficial data regarding public health issues affecting large patient populations such as cancer, heart disease, smoking, asthma, and diabetes.
Are HEDIS measures mandatory?
HEDIS measures all have certain documentation requirements and parameters that are taken into account when a health plan is given a score. Requirements vary by health plan provider, but typically participation in HEDIS data collection is mandatory.
Which payer type uses HEDIS measures?
HEDIS refers to a widely used set of performance measures in the managed care industry. More than 90 percent of health plans—HMOs, POS plans, and PPOs—use HEDIS to measure performance.
What is the difference between HEDIS and stars?
For CAHPS measures, Star Ratings combine relative percentile distribution with significance and reliability testing. For HEDIS measures, Star Ratings use a clustering algorithm that identifies “gaps” in the data and creates five categories (one for each Star Rating).
How many domains of care does HEDIS have?
six domains of careThe Healthcare Effectiveness Data and Information Set (HEDIS®) is a tool used by more than 90% of America's health plans to measure performance on important dimensions of care and service. Altogether, HEDIS consists of 92 measures across six domains of care.
What are the 2021 HEDIS measures?
HEDIS MY 2020 & MY 2021 Draft FHIR Digital Measures (5 Measures)Avoidance of Antibiotic Treatment for Acute Bronchitis/Bronchiolitis (AAB)Cervical Cancer Screening (CCS)Childhood Immunization Status (CIS)Immunizations for Adolescents (IMA)Non-Recommended PSA-Based Screening in Older Men (PSA)
What are the stars measures?
CMS Star ratings include quality of care measures such as Adult BMI, Controlling Blood Pressure, Breast Cancer Screening, Osteoporosis Management in Women Who Had a Fracture, Comprehensive Diabetes Care, Colorectal Screenings, and others.
What is the difference between HEDIS and stars?
For CAHPS measures, Star Ratings combine relative percentile distribution with significance and reliability testing. For HEDIS measures, Star Ratings use a clustering algorithm that identifies “gaps” in the data and creates five categories (one for each Star Rating).
What is HEDIS analysis?
Analysis of HEDIS data helps identify gaps in care, particularly preventive care, in such important and chronic populations as patients with diabetes mellitus, patients with cardiovascular disease, and patients with lung disease. We can also identify and address at-risk pediatric populations who fail to complete preventive care such as immunizations, dental and well-child care.
What is the value of HEDIS to Magellan?
So, what is the value of HEDIS to Magellan? Aside from being a collection and reporting contract requirement for many of our customers and our own health plan, HEDIS gives Magellan valuable information about the populations we serve.
What is HEDIS in healthcare?
Magellan’s collection of HEDIS (Healthcare Effectiveness Data and Information Set ) quality measures for 2017 has entered the final phase of data collection. You’ve probably heard of the acronym HEDIS – but what does it stand for and what does it mean to you? The Healthcare Effectiveness Data and Information Set – HEDIS — was created by the National Committee for Quality Assurance (NCQA) to measure the clinical quality performance of health plans. This is accomplished through the collection and analysis of data documenting the clinical care received by individual plan members from providers, influenced through activities and programs delivered by the health plans. The data is aggregated and reported collectively to reflect the ‘collective’ or population-based care received by the plan’s membership. These reports have become a major component of quality rating systems that measure the clinical quality performance of health plans by Centers for Medicare & Medicaid Services, states offering Medicaid and other entities. Right now, Magellan has entered the final phase of data collection for HEDIS quality measures for 2017.
How many measures are there in Hedis 2017?
There are 91 HEDIS 2017 measures, but it’s important to note that the number may vary from year to year as new measures are added to the set and some are retired. The measures cover many aspects of healthcare including preventive care such as screening tests (e.g., mammograms) and immunizations, management of physical and mental health conditions, access and availability of care, patient experience, utilization and relative resource use. Data is reported individually for each product and line of business
What are the measures of behavioral health?
Behavioral health has multiple measures that include ensuring continuity of care, appropriate psychotropic medication management/adherence, and initiation and engagement of drug and alcohol abuse treatment.
Why is HEDIS score important?
Higher scores can help compete more effectively in various markets. HEDIS score reporting are often required in public markets as well, where the results are often reported to the states, or occasionally counties, in which the plans reside. Behavioral health and pharmacy are well represented in the HEDIS measure set.
What is HEDIS survey?
HEDIS survey measures and standardized surveys from the Consumer Assessment of Healthcare Providers and Systems (CAHPS ®) program.
What is a VSD in HEDIS?
The Rules for Allowable Adjustments are included in the HEDIS Volume 2 publication after the applicable HEDIS measure specifications. NCQA’s HEDIS Value Set Directory (VSD) includes the necessary third-party codes for use with adjusted measure specifications.
What is a quality rating system?
Quality Rating System Measure Technical Specifications are unique to the issuers offering plans on the Exchange and participating in the CMS Quality Rating System (QRS).
What is CAHPS trademark?
CAHPS ® is a registered trademark of the Agency for Healthcare Research and Quality (AHRQ).
What is the T1015 code?
NOTE: **T1015 HCPCS code which identifies an all-inclusive clinic visit for services rendered at a Federally Qualified Health Center (FQHC).
What are the exclusions for hospice care?
Exclusions for hospice, palliative care , advanced illness, frailty and long-term nursing home residence exclusions are specified in HEDIS measures where the services being captured may not be of benefit for this population or may not be in line with patients’ goals of care.
What is supplemental data?
Supplemental Data: Standardized file process to collect data from sites to close gaps. • Synchronous telehealth requires real-time interactive audio and video telecommunications.
What is the numerator in healthcare?
Numerator: The number of members who meet compliance criteria based on NCQA technical specifications for appropriate care, treatment or service.
What is NCQA value set directory?
The National Committee for Quality Assurance (NCQA) uses a “Value Set Directory” to organize associated codes for each measure.
What is the medication for dementia?
Dispensed a dementia medication: Donepezil, galantamine, rivastigmine or memantine.
What is required exclusion for hospice?
Required Exclusions: HOSPICE/PALLIATIVE CARE: Members who use services or elect to use a benefit, regardless of when the services began in the measurement year. Supplemental data can be used for the hospice exclusion.
How Is HEDIS Used?
Fundamentally, HEDIS is used as a measure of effectiveness of care, access to care, and the experience of care. Its most “official” use is through the CMS five-star metrics measures. Higher star ratings for organizations enrolled in Medicare Advantage will receive quality bonus payments (QBPs) and rebates. Specifically, four- or higher-star ratings will trigger direct bonus payments to plan operators and rebates that can be returned to their beneficiaries.
What is stability health?
Stability Health is committed to improving patient outcomes, and many of the support services we offer help to address the areas of diabetes care management that HEDIS covers. Through providing education and resources, we aid patients in managing their care, while also assisting clinicians in performing more comprehensive evaluations to identify those most at risk to improve patient care.
What age does hedis assessment apply?
The HEDIS assessment measurements for comprehensive diabetes care apply to health plan members between the ages of 18 and 75 with type 1 or 2 diabetes . The four measurements all must have been taken within the measurement year and are as follows:
Why is HEDIS important?
Proper diabetes management is essential for controlling blood glucose, reducing risks for complications, and prolonging a higher quality of life. While patients are mainly responsible for their self-care, the HEDIS measures help to ensure that clinicians are following through with their responsibility in monitoring status of diabetes, screening for potential complications, and helping patients achieve control of their diabetes.
What is HEDIS in healthcare?
Originally created in 1991 by the National Committee for Quality Assurance (NCQA), HEDIS was designed as a means for consumers to compare a health plan’s performance against a set of benchmarks in order to effectively evaluate and compare against other health plans. Over the past several decades, HEDIS has increasingly become a means by which healthcare plans are able to track their own year-to-year performance in order to maximize care and better meet patient needs.
What is the HEDIS system?
As a chronic condition, diabetes requires constant management by patients and consistent support from clinical care teams. This support system is offered through thousands of different individual providers and hundreds of clinics and hospitals in the U.S. With such a large variance of where care originates, it’s important to have some standards of measurement to ensure that provided care is effective, responsive, and comprehensive. One important set of standards that both patients and clinicians should be familiar with is the Healthcare Effectiveness Data and Information Set – also known as HEDIS.
What is the purpose of HEDIS?
Despite its increasing use by payers and providers, it is important to remember that the original intent of HEDIS was to inform consumers about the difference in the quality of care in available health plans. The NCQA publishes its annual Health Insurance Plan Ratings online for consumers.
What data sources are used for HEDIS?
Data systems that may be eligible for HEDIS ® ECDS reporting include, but are not limited to, member eligibility files, EHRs, clinical registries, HIEs, administrative claims systems, electronic laboratory reports (ELR), electronic pharmacy systems, immunization information systems (IIS) and disease/case management registries.
What is ECDS reporting?
The ECDS reporting standard represents a step forward in adapting HEDIS to accommodate the expansive information available in electronic clinical datasets used for patient care and quality improvement.
What is ECDS architecture?
The ECDS architecture was designed to help HEDIS implementers understand how health IT can increase the efficiency of quality reporting, while also providing an incentive to connect to data in these other sources.
What is ECDS in health care?
Electronic Clinical Data Systems (ECDS) are a network of data containing a plan member’s personal health information and records of their experiences within the health-care system. The HEDIS ® ECDS Reporting Standard provides health plans a method to collect and report structured electronic clinical data for HEDIS quality measurement and quality improvement.
Why is ECDS reporting important?
Ultimately, ECDS reporting creates insight for managing the health of individuals and groups. Public reporting helps make the promise of ECDS a reality.
What is a HIE registry?
HIEs and clinical registries eligible for this reporting category include state HIEs, immunization information systems (IIS), public health agency systems, regional HI Es (RHIO), Patient-Centered Data Homes™ or other registries developed for research or to support quality improvement and patient safety initiatives. Doctors, nurses, pharmacists, other health care providers and patients can use HIEs to access and share vital medical information, with the goal of creating a complete patient record. 3 Clinical registries can be sponsored by a government agency, nonprofit organization, health care facility or private company, and decisions regarding use of the data in the registry are the responsibility of the registry’s governing committee. 4
What is case management system?
Case management system. A shared database of member information collected through a collaborative process of member assessment, care planning, care coordination or monitoring of a member’s functional status and care experience. Case management systems eligible for this category of ECDS reporting include any system developed to support the organization’s case/disease management activities, including activities performed by delegates.
