What does SVT stand for in drug?
Specimen Validity Test SVT. A Specimen Validity Test (SVT) is one that determines that a specimen is directly from the donor. This is usually accomplished through the use of temperature activated drug test strips. Anything below or above a defined temperature is considered to be positive drug test. SVT tests may also determine whether specimens ...
What is the drug of choice for supraventricular tachycardia?
The safety profile of adenosine suggests that it should be the drug of first choice for the treatment of supraventricular tachycardia, but only limited comparative data to support this view are available at present. What antiarrhythmic is used for SVT? Intravenous adenosine, verapamil, and diltiazem are effective in acute termination of SVT.
How to stop an episode of supraventricular tachycardia?
You can make changes to your lifestyle to reduce your chances of having episodes, such as:
- cutting down on the amount of caffeine or alcohol you drink
- stopping or cutting back on smoking
- making sure you get enough rest
What can trigger supraventricular tachycardia?
Nicotine and illegal drugs, such as amphetamines and cocaine, may trigger an episode of supraventricular tachycardia. Over time, untreated and frequent episodes of supraventricular tachycardia (SVT) may weaken the heart and lead to heart failure, particularly if there are other medical conditions.
What medication is best for SVT?
What is the best medication for SVT?Best medications for SVTAdenocard (adenosine)AntiarrhythmicIntravenous injectionCardizem (diltiazem)Calcium-channel blockerOral or injectionCalan (verapamil)Calcium-channel blockerOral or injectionLopressor (metoprolol tartrate)Beta-blockerOral or injection3 more rows•Dec 28, 2020
What is the initial treatment for SVT?
The initial treatment for a sudden episode of SVT is vagal maneuvers, such as bearing down, coughing, or holding your breath. These actions can slow the electrical impulses in your heart and may stop the SVT.
What is the most common treatment for SVT?
Most people with supraventricular tachycardia (SVT) don't need treatment. However, if you have long or frequent episodes, your health care provider may recommend the following: Carotid sinus massage.
What is the best beta blocker for SVT?
Beta blockers such as IV metoprolol or esmolol infusion are often used in acute SVT, but data regarding this practice are limited.
Can SVT be treated with medication?
Medications to Treat Supraventricular Tachycardia (SVT) To best treat supraventriculat tachycardia, medications need to affect the conductivity of the A-V node, the staircase between the upper and lower heart chambers. These medications include: Beta-blocking agents. Calcium channel agents.
Which Medication is the first line to treat asymptomatic SVT?
Adenosine (Adenocard) Adenosine is the first-line medical treatment for the termination of paroxysmal SVT. It is a short-acting agent that alters potassium conductance into cells and results in hyperpolarization of nodal cells.
Are beta blockers used for SVT?
Medications typically used to treat SVT are: Beta Blockers: A beta blocker is a very safe medication that works by reducing the effect adrenalin has on the heart. Beta blockers are commonly used to treat high blood pressure and other common heart problems. Calcium Channel Blockers.
Is metoprolol good for SVT?
In patients with systolic blood pressure greater than 100 mm Hg but without an acute myocardial infarction the risk of hypotension necessitating treatment was small. Metoprolol appears to be an effective and safe drug in the treatment of supraventricular tachycardia.
How is SVT treated and managed?
Many people with SVT have a procedure called catheter ablation. This procedure can stop the rhythm problem in most people. During this procedure, the extra electrical pathway or cells in the heart that are causing the fast heart rate can often be identified and destroyed. Ablation is considered safe.
What triggers SVT episodes?
SVT is usually triggered by extra heartbeats (ectopic beats), which occur in all of us but may also be triggered by: some medications, including asthma medications, herbal supplements and cold remedies. drinking large amounts of caffeine or alcohol. stress or emotional upset.
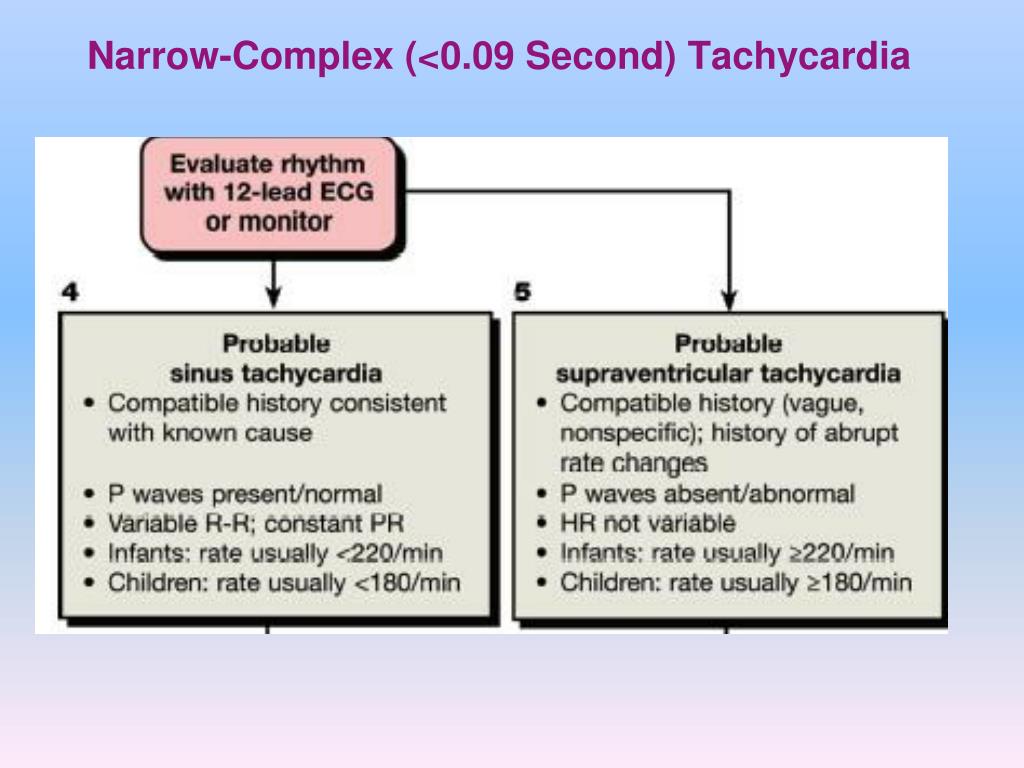
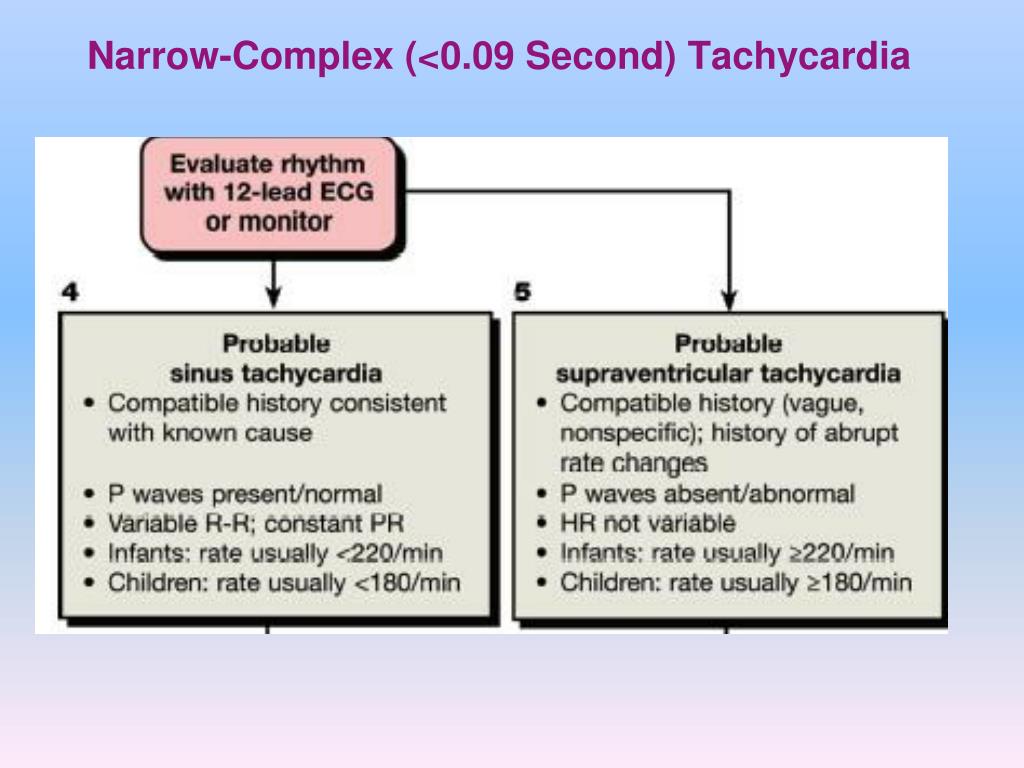
What heart rate is considered SVT?
Causes of supraventricular tachycardia (SVT) A normal resting heart rate is 60 to 100 beats per minute (bpm). But with SVT your heart rate suddenly goes above 100bpm. This can happen when you're resting or doing exercise.
What is the most common cause of SVT?
SVT is often caused by faulty electrical signaling in your heart. It's often brought on by premature beats. Some types of SVT run in families, so genes may play a role. Other types may be caused by lung problems.
Does a drug have multiple schedules?
The drug has multiple schedules. The schedule may depend on the exact dosage form or strength of the medication.
Is there a lack of accepted safety for use under medical supervision?
Has a high potential for abuse. Has a currently accepted medical use in treatment in the United States or a currently accepted medical use with severe restrictions. Abuse may lead to severe psychological or physical dependence.
What is a paroxysmal form of SVT?
Paroxysmal forms of SVT (PSVT) are regular recurrent tachycardias with a sudden onset and termination. If terminated by vagal manoeuvres, a reentrant tachycardia involving the AV node is most likely. The ventricular rate during SVT is commonly between 140–250 beats/min (bpm). If vagal or pharmacologic manoeuvres (adenosine) during an SVT result in AV block with persistence of atrial tachycardia, the diagnosis is most likely AT. The A:V ratio is always 1:1 in AP mediated tachycardias . Non-paroxysmal forms of SVT are ongoing repetitive or permanent/incessant tachycardias, which if left untreated can result in systolic left ventricular dysfunction and dilation (tachycardiomyopathy). These forms of tachycardias—for example, incessant AT or AFL—may be of unknown duration and without significant symptoms. Inappropriate sinus tachycardia (IST) is another form of non-paroxysmal SVT.
What is the best treatment for tachycardia?
The treatment of choice to prevent tachycardia recurrences in WPW patients is catheter ablation , which is successful in over 95% of cases and with a low risk for adverse events depending on AP location. Prophylactic antiarrhythmic drug treatment (propafenone, flecainide, sotalol, amiodarone) is justified when awaiting such an ablation procedure or in patients not accepting the procedure, if the patient is symptomatic with frequent and long lasting episodes. A combination of a class 1C agent (propafenone or flecainide) and a β-blocking agent is the most effective drug regimen. 12 Class I antiarrhythmic drugs and amiodarone prolong the anterograde refractory period of the AP but have minor effect in the retrogradely conducting AP. The data on efficacy of sotalol are limited 13 and no study has yet shown that amiodarone is superior to class Ic antiarrhythmic agents or sotalol. In a prospective study of azimilide, a novel class III agent, the time to recurrence of symptoms related to SVT did not differ significantly from the placebo group, indicating that azimilide did not confer a beneficial effect compared with placebo. 14 β-blocking agents have no effect on APs and their ability to prevent tachycardia recurrences in patients with the WPW syndrome is unknown. Digitalis and calcium channel blocking agents (verapamil, diltiazem) may facilitate the development of VF during AF in patients with WPW syndrome, and should therefore not be used. 15 Long term antiarrhythmic drug treatment is not recommended in WPW patients with high risk profiles (occupations or lifestyles), or in those with severely symptomatic episodes.
What is SNRT in medical terms?
Sinus node reentry tachycardia (SNRT), which originates from re-entrant circuits within or close to the sinus node, is paroxysmal in nature and may be terminated by vagal manoeuvres or adenosine. Inappropriate sinus tachycardia (IST), which usually appears in women <50 years of age, is an uncommon form of sinus tachycardia characterised by a persistent and excessive rate increase in response to activity during daytime and rate normalisation at night. The P wave morphology during both SNRT and IST is identical to sinus rhythm.
Where does supraventricular tachycardia originate?
Supraventricular tachycardia (SVT) is characterised by a rapid impulse formation, that emanates from the sinus node, from atrial tissue (focal or macro-reentrant atrial tachycardia (AT)), from the atrioventricular (AV) no de, or from anomalous muscle fibres that connect the atrium with the ventricle (accessory pathways (APs)).
What is the most common form of AVNRT?
The most common form of AVNRT (slow-fast) utilises the slow pathway anterogradely and the fast pathway retrogradely. Less common are the fast-slow AVNRT (reversed tachycardia circuit), resulting in a long R-P tachycardia with negative P waves in lead III and aVF before the QRS, and intermediate forms (slow-slow AVNRT). Associated structural heart disease is uncommon.
Can AV nodal acting drugs be used for preexcitated tachycardia?
1 AV nodal acting drugs should not be used in patients with preexcitated tachycardias. Immediate DC cardioversion is the treatment of choice for all haemodynamically unstable tachycardias.
Can a catherter ablation be performed in the case of systolic left ventricular dysfunction?
Catheter ablation should always be performed in the case of systolic left ventricular dysfunction, which usually normalises within a few months after abolishing the tachycardia. Macro-reentrant ATs are rarely prevented by drugs such as flecainide, propafenone, and amiodarone. By slowing atrial conduction velocity, these drugs may even facilitate the recurrences of macro-reentrant AT, whose atrial rate is then slower than in the basal situation. Amiodarone with or without verapamil or diltiazem may be used for rate control to improve symptoms, and can be used in symptomatic patients not amenable to ablation or other drug treatment.
What is the test for SVT?
Tests to diagnosis SVT include: Electrocardiogram (ECG). During an ECG, sensors (electrodes) that can detect the electrical activity of your heart are attached to your chest and sometimes to your limbs. An ECG measures the timing and duration of each electrical phase in your heartbeat. Holter monitor.
How to stop SVT?
You may be able to stop an episode of SVT by using particular movements such as holding your breath and straining as you would during a bowel movement, dunking your face in ice water, or coughing.
What is a supraventricular tachycardia test?
This device detects abnormal heart rhythms and is implanted under the skin in the chest area. If your doctor doesn't find a heart rhythm problem during those tests, you may need other tests, such as: Stress test. For some people, supraventricular tachycardia is triggered or worsened by stress or exercise.
How to diagnose supraventricular tachycardia?
To diagnose supraventricular tachycardia, your doctor will ask questions about your symptoms and your medical history and perform a physical exam. Blood tests are usually done to check for other health conditions that could cause your symptoms, such as thyroid disease.
How does cardioversion work?
Cardioversion may be done using medications or during a heart procedure. In the procedure, a shock is delivered to your heart through paddles or patches on your chest. The current affects the electrical signals in your heart and can restore a normal rhythm. Medications.
What is a tilt table test?
Your heart rate and blood pressure are monitored as you lie flat on a table. The table is then tilted as if you were standing up. Your doctor observes how your heart and the nervous system that controls it respond to the change in angle.
What is the best medication for SVT?
The mechanism and symptoms of supraventricular tachycardia can vary widely between patients, so there is no “best” medication for SVT. The management of supraventricular tachycardia will depend on the type of SVT, the symptoms, and the patient’s overall medical situation and tolerance for side effects.
What is the best home remedy for SVT?
In most people, lifestyle changes and home remedies are enough to manage and prevent supraventricular tachycardia. However, if symptoms persist or breathing becomes difficult, immediate medical help is needed.
What is SVT?
Supraventricular tachycardia occurs when the heart occasionally beats too fast for no identifiable reason. A glitch in nerve signals rather than a problem with heart muscles causes the heart to beat too fast (tachycardia).
How is SVT diagnosed?
Supraventricular tachycardia is diagnosed from the patient’s symptoms and an electrocardiogram (ECG), a device that measures the heart’s electrical activity. The most common symptoms of supraventricular tachycardia include:
What is AVRT in heart?
Atrioventricular reciprocating tachycardia (AVRT) happens when the nerve signal passes to the ventricles through the AV node but also an extra electrical connection exists that bridges the atrium and ventricle which can conduct electricity - known as an accessory pathway. The heart can get caught up in a looping circuit where electricity either goes down the AV node and returns back to the atrium through the accessory pathway, or the reverse happens with the signal traveling down the accessory pathway and returns through the AV node. Again, one heartbeat can produce two or more additional heartbeats as the electrical signal cycles back on itself. This is the most common form of SVT found in infants and children.
What is the name of the tachycardia that happens when you have two channels through the AV no?
Atrioventricular nodal reentrant tachycardia (AVNRT), also called paroxysmal supraventricular tachycardia (PSVT), happens when you have two channels through the AV node so that the nerve signal not only passes through the AV node to the lower chambers but simultaneously circles around the AV node back to the atria, causing the upper chambers to contract a second time. Round and round the signal can go, making the upper chambers beat very quickly with a rapid and regular ventricular responseAVNRT is the most common form of SVT among adults, particularly in women and older adults.
What is the best diet for supraventricular tachycardia?
There is no magic diet for supraventricular tachycardia. It’s enough to say that many minerals and vitamins are necessary for nerves and muscles to function properly. In particular, potassium, magnesium, calcium, and even sodium play an outsized role in nerve conduction and muscle contraction. Too little or too much of these minerals will cause problems. Eat a healthy diet sufficient in nutrients and minerals without overdoing it.
What is the treatment for recurring SVT?
Ongoing treatment of recurring SVT. If you have recurring episodes of SVT, you may need to take medicines, either on an as-needed basis or daily. Medicine treatment may include beta-blockers, calcium channel blockers, or other antiarrhythmic medicines.
How to treat sudden onset SVT?
Your doctor will teach you how to do these safely. These are things such as bearing down or putting an ice-cold wet towel on your face.
How is supraventricular tachycardia treated?
How is supraventricular tachycardia (SVT) treated? Your treatment for SVT depends on a few things. They include what type of SVT, how often you have episodes, and how severe your symptoms are. The goals of treatment are to prevent episodes, relieve symptoms, and prevent problems.
What are the symptoms of SVT?
SVT is usually treated if: You have symptoms such as dizziness, chest pain, or fainting that are caused by your fast heart rate. Your episodes of fast heart rate are occurring more often or do not return to normal on their own.
How to tell if you have SVT?
SVT is usually treated if: 1 You have symptoms such as dizziness, chest pain, or fainting that are caused by your fast heart rate. 2 Your episodes of fast heart rate are occurring more often or do not return to normal on their own.
What medicine can be given to prevent SVT?
For emergent cases, calcium channel or beta blockers can be given through IV (intravenously) for more rapid correction of the heart rhythm. Adenosine is another medicince that can be given through IV as well that can work in a matter of seconds.
How to prevent SVT?
Your healthcare provider might suggest other ways to help prevent SVT, such as the following: 1 Have less alcohol and caffeine 2 Don't smoke 3 Lower your stress 4 Eat foods that are healthy for your heart 5 Don't take recreational drugs, especially stimulants that can over-excite the heart muscle. Some herbs and supplements can have this same effect. Always check with your healthcare team before you take any non-prescribed medicines. 6 Stay well hydrated and get enough sleep
