Previously, it was believed that acetaminophen induces analgesia by inhibiting cyclooxygenase enzymes; however, it has been considered recently that the main analgesic mechanism of acetaminophen is its metabolization to N -acylphenolamine (AM404), which then acts on the transient receptor potential vanilloid 1 (TRPV1) and cannabinoid 1 receptors in the brain.
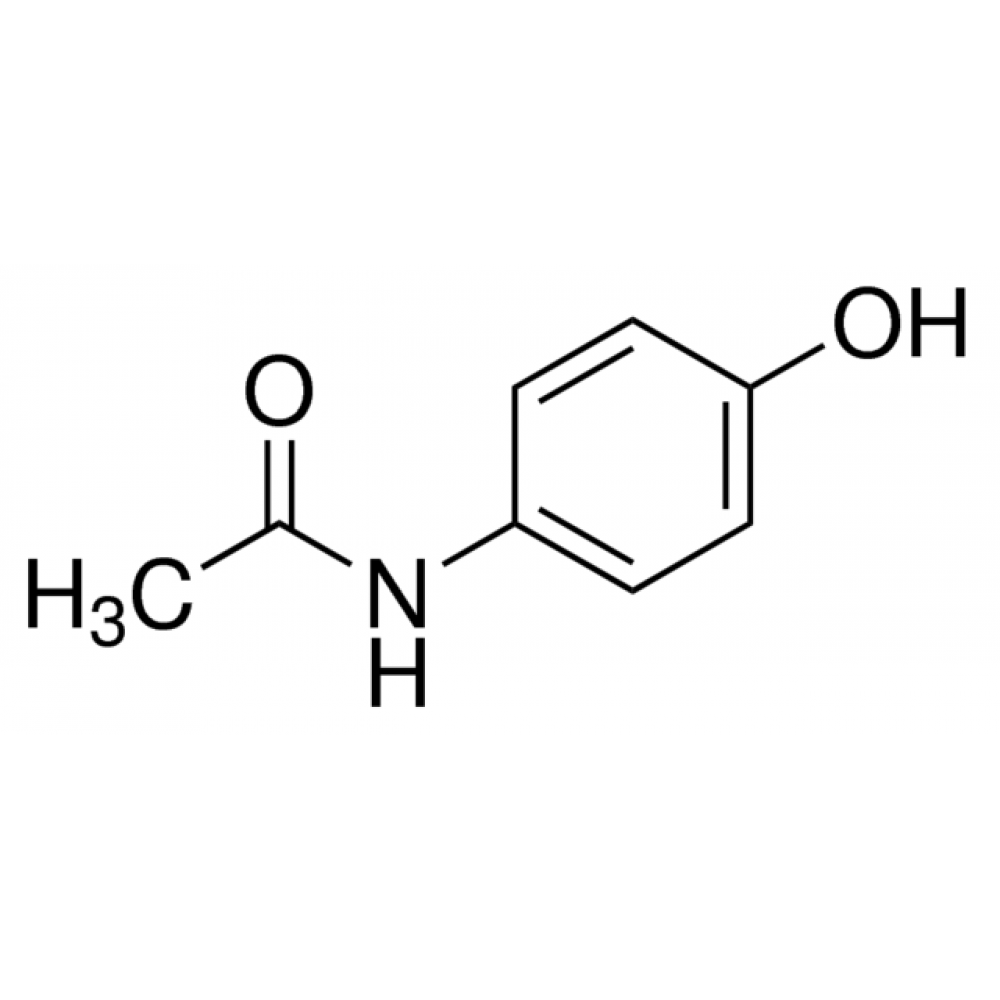
Is acetaminophen and paracetamol the same thing?
There is no difference between paracetamol and acetaminophen, according to Drugs.com. Acetaminophen is the generic form of paracetamol. Both drugs contain the same properties, treat the same ailments and produce the same effects. Paracetamol is a pain reliever and fever reducer that can be purchased over the counter or with a prescription.
What are the risks and benefits of acetaminophen?
- Bloody or black, tarry stools
- bloody or cloudy urine
- fever with or without chills (not present before treatment and not caused by the condition being treated)
- pain in the lower back and/or side (severe and/or sharp)
- pinpoint red spots on the skin
- skin rash, hives, or itching
What does acetaminophen do to your body?
Symptoms of liver damage include:
- yellowing of your skin or the whites of your eyes (jaundice)
- pain in the upper right area of your abdomen
- nausea or vomiting
- loss of appetite
- fatigue
- sweating more than usual
- pale skin
- unusual bruising or bleeding
- dark or tea-colored urine
- dark, tarry stools
Why is acetaminophen not a NSAID?
Why is APAP not an NSAID? Tylenol (acetaminophen) is not anti-inflammatory It’s not an NSAID. In other words, it’s not an anti-inflammatory drug. It does not help reduce swelling or inflammation. Instead, acetaminophen works by blocking your brain from releasing substances that cause the feeling of pain.

What is acetaminophen mechanism of action?
Mechanism of Action [2][3] Like NSAIDs, acetaminophen has analgesic and antipyretic properties. However, studies have shown that acetaminophen lacks peripheral anti-inflammatory properties. It may be that acetaminophen inhibits the COX pathway in the central nervous system but not peripheral tissues.
What is the pharmacodynamics of acetaminophen?
The pharmacodynamics of acetaminophen can be described using a sigmoidal Emax model with a low Hill coefficient. To achieve a mean posttonsillectomy pain score of 3.6 of 10, an effect compartment concentration of 10 mg/l is necessary.
What is the pharmacokinetics of acetaminophen?
Pharmacokinetics. Upon ingestion, acetaminophen is rapidly absorbed from the gastrointestinal (GI) tract and quickly distributed throughout the body. Peak plasma concentrations are achieved within 30 to 60 minutes4; food may delay time to peak concentration, but the extent of absorption is not affected.
What is the mechanism of action of analgesics?
Analgesics can inhibit the sensation of pain by inhibiting transmission of non-nociceptive impulses along primary afferents (eg, local anesthetics) or by altering the perception of pain (eg, opioids).
What does acetaminophen do to your body?
Acetaminophen is a pain reliever and fever reducer. It is thought to work to relieve minor aches and pains by elevating the body's overall pain threshold so you feel less pain, and lowers your fever by helping your body eliminate excess heat.
What is mechanism of action in pharmacology?
(MEH-kuh-nih-zum … AK-shun) In medicine, a term used to describe how a drug or other substance produces an effect in the body. For example, a drug's mechanism of action could be how it affects a specific target in a cell, such as an enzyme, or a cell function, such as cell growth.
What receptor does acetaminophen bind to?
Acetaminophen acts not only on the brain but also the spinal cord and induces analgesia. Moreover, the most possible analgesic mechanism is that the acetaminophen metabolite AM404 acts by activating TRPV1 and/or CB1 receptors.
What is the pharmacological class of acetaminophen?
Acetaminophen is in a class of medications called analgesics (pain relievers) and antipyretics (fever reducers).
How is acetaminophen absorbed?
The absorption of oral acetaminophen occurs primarily along the small intestine by passive diffusion. Therefore, the rate-limiting step is the rate of gastric emptying into the intestines.
What transport mechanism is involved in absorption of paracetamol from GIT into blood?
As paracetamol is absorbed from the small intestine by passive diffusion, the rate-limiting point is the gastric emptying into the intestines.
What is mechanism of action of NSAIDs?
The main mechanism of action of NSAIDs is the inhibition of the enzyme cyclooxygenase (COX). Cyclooxygenase is required to convert arachidonic acid into thromboxanes, prostaglandins, and prostacyclins. [9] The therapeutic effects of NSAIDs are attributed to the lack of these eicosanoids.
What is the mechanism of action for ibuprofen?
The main mechanism of action of ibuprofen is the non-selective, reversible inhibition of the cyclooxygenase enzymes COX-1 and COX-2 (coded for by PTGS1 and PTGS2, respectively; Fig.
How does acetaminophen differ from NSAIDs in terms of its mechanism of action?
These two drugs have different mechanisms of action in the body. Tylenol is the brand name for the drug acetaminophen, and it works by disrupting pain signals in the body. NSAIDs alleviate pain while reducing inflammation. They work by preventing the production of a hormone that controls inflammation.
How does acetaminophen work vs ibuprofen?
by Drugs.com Acetaminophen is only effective at relieving pain and fever, while ibuprofen relieves inflammation in addition to pain and fever. Other key differences: Some research suggests NSAIDs such as ibuprofen are more effective than acetaminophen at relieving pain.
What does acetaminophen do to the liver?
Harmless at low doses, acetaminophen has direct hepatotoxic potential when taken as an overdose and can cause acute liver injury and death from acute liver failure. Even in therapeutic doses, acetaminophen can cause transient serum aminotransferase elevations.
How does acetaminophen damage the liver?
How does an overdose of acetaminophen cause liver injury? The answer is that liver damage from acetaminophen occurs when the glutathione pathway is overwhelmed by too much of acetaminophen's metabolite, NAPQI. Then, this toxic compound accumulates in the liver and causes damage.
Does acetaminophen inhibit COX?
Because acetaminophen is a weak inhibitor in vitro of both cyclooxygenase (COX)-1 and COX-2, the possibility exists that it inhibits a so far unidentified form of COX, perhaps COX-3. In animal studies, COX enzymes in homogenates of different tissues vary in sensitivity to the inhibitory action of acetaminophen.
Is acetaminophen cyclooxygenase 3?
Mechanism of action of acetaminophen: is there a cyclooxygenase 3? Acetaminophen, also known as paracetamol, is a nonsteroidal anti-inflammatory drug with potent antipyretic and analgesic actions but with very weak anti-inflammatory activity. When administered to humans, it reduces levels of prostaglandin metabolites in urine ...
Does paracetamol reduce prosta?
When administered to humans, it reduces levels of prostaglandin metabolites in urine but does not reduce synthesis of prosta …. Acetaminophen, also known as paracetamol, is a nonsteroidal anti-inflammatory drug with potent antipyretic and analgesic actions but with very weak anti-inflammatory activity. When administered to humans, it reduces levels ...
What is the mechanism of action of paracetamol?
Paracetamol (Acetaminophen): mechanisms of action. Paracetamol has a central analgesic effect that is mediated through activation of descending serotonergic pathways. Debate exists about its primary site of action, which may be inhibition of prostaglandin (PG) synthesis or through an active metabolite influencing cannabinoid receptors.
Does paracetamol reduce ferryl?
Paracetamol acts as a reducing cosubstrate on the POX site and lessens availability of the ferryl protoporphyrin IX radical cation. This effect can be reduced in the presence of hydroperoxide-generating lipoxygenase enzymes within the cell (peroxide tone) or by swamping the POX site with substrate such as PGG(2).
Is paracetamol an analgesic?
Paracetamol has a central analgesic effect that is mediated through activation of descending serotonergic pathways. Debate exists about its primary site of action, which may be inhibition of prostaglandin (PG) synthesis or through an active metabolite influencing cannabinoid receptors. Prostaglandin ….
Does paracetamol have an active metabolite?
Alternatively, paracetamol effects may be mediated by an active metabolite (p-ami nophenol). p-Aminophenol is conjugated with arachidonic acid by fatty acid amide hydrolase to form AM404. AM404 exerts effect through cannabinoid receptors. It may also work through PGHS, particularly in areas of the brain with high concentrations ...
How does acetaminophen affect the liver?
Acetaminophen is responsible for an estimated 500 deaths and 50000 emergency department visits in the United States each year.[9] It is the most common drug-related cause of acute liver failure. The mechanism of hepatic injury is due to the drug metabolism properties of acetaminophen.[10] Following therapeutic concentrations of oral acetaminophen, 60% to 90% of the drug gets metabolized in the liver to glucuronic acid- and sulfate-conjugate metabolites. A smaller fraction (approximately 5% to 15%) undergoes metabolism by the cytochrome P450 system (CYP450). Metabolism primarily via CYP2E1 results in the formation of the toxic intermediate N-acetyl-p-benzoquinone imine (NAPQI). Normally, NAPQI is neutralized by glutathione to nontoxic metabolites. However, with excessive doses of acetaminophen, the normal phase II drug metabolism pathways become depleted, and the CYP450 pathway metabolizes a higher portion of the acetaminophen taken, resulting in high concentrations of NAPQI formation, and the limited glutathione stores can become depleted. Without glutathione, NAPQI concentrations build-up, and NAPQI, as a reactive intermediate, can react with cellular macromolecules, proteins, lipids, and nucleic acids. This phenomenon can lead to centrilobular (Zone 3) hepatic injury and hepatocellular death. There can also be nephrotoxicity.
What is the most important aspect of acetaminophen toxicity?
The most crucial aspect of acetaminophen toxicity is prevention. Physicians, nurses, and pharmacists all share in this responsibility. Pharmacists and nurses need to emphasize the maximum dose permitted daily. Patients also need to understand how to look for acetaminophen in various medications they take and how to calculate the dose they receive when they combine products. Pharmacists need to perform medication reconciliation to look for drug interactions, as well as verify that there are not too many acetaminophen-containing drugs in the regimen. If there are concerns, the pharmacist should report them to the nurse and physician.
What is the best antidote for acetaminophen overdose?
The only approved antidote for acetaminophen overdose and toxicity is N-acetylcysteine (NAC).[11] NAC is a precursor to glutathione synthesis and helps to restore the intracellular stores of glutathione to neutralize the NAPQI compound, and it can inactivate NAPQI directly. N-acetyl cysteine can be administered orally or by IV. IV N-acetyl cysteine is typically preferred because vomiting is common with acetaminophen overdose. It is effective when administered within the first few hours (up to 8 to 10 hours) of a toxic ingestion of acetaminophen. N-acetyl cysteine administration has a 20-hour IV protocol or 72-hour oral protocol, and the clinician must monitor the AST/ALT during treatment.[12] One important thing to keep in mind is that most patients do not have symptoms in the first few hours of ingestion of toxic doses of acetaminophen and may only have abdominal pain and nausea as symptoms for the first 12 to 24 hours. Between 24 and 72 hours, these symptoms may dissipate, although AST/ALT concentrations may be abnormal. Patients who present more than 24 hours following ingestion of toxic doses of acetaminophen may have symptoms such as nausea, vomiting, jaundice, abdominal pain, and hypotension. These patients may require airway management, intravenous fluids, vasopressors, hemodialysis, or management of cerebral edema or other symptoms as they arise.
Is acetaminophen a contraindication?
Contraindications to the use of acetaminophen include hypersensitivity to acetaminophen, severe hepatic impairment, or severe active hepatic disease. However, there is a general debate among experts whether hepatic impairment is truly a limiting factor, as it would likely be associated with decreased production of the toxic metabolite, N-acetyl-p-benzoquinoneimine (NAPQI).
Does acetaminophen cross the placental barrier?
Acetamino phen can cross the placental barrier, but there is no evidence of increased teratogenic effects due to the use of normal doses of acetaminophen during pregnancy.[8] Acetaminophen also is excreted into breast milk, but there have not been many observations of adverse reactions in nursing infants.
Does acetaminophen cause liver failure?
Acetaminophen use has been linked to liver failure and sometimes has led to liver transplant or death. The hepatotoxicity occurring with acetaminophen use typically correlates with high doses of acetaminophen that exceed the recommended maximum dose.[6] This effect may involve the intake of more than one drug product that contains acetaminophen as an ingredient. Liver damage also has been seen in patients with chronic dosing of acetaminophen.
Can acetaminophen be administered intravenously?
Acetaminophen can be administered orally, rectally, or intravenously (IV). [5]
Where is acetaminophen metabolized?
Acetaminophen is the major metabolite of _ phenacetin _ and _ acetanilid _. [F4124] Acetaminophen is mainly metabolized in the liver by first-order kinetics and its metabolism of comprised of 3 pathways: conjugation with glucuronide, conjugation with sulfate, and oxidation through the cytochrome P450 enzyme pathway, mainly CYP2E1, to produce a reactive metabolite ( N-acetyl-p-benzoquinone imine or NAPQI ). At normal therapeutic doses, NAPQI undergoes fast conjugation with glutathione and is subsequently metabolized to produce both cysteine and mercapturic acid conjugates. [Label] High doses of acetaminophen (overdoses) can lead to hepatic necrosis due to the depletion of glutathione and of binding of high levels of reactive metabolite ( NAPQI) to important parts of liver cells. The abovementioned damage to the liver can be prevented by the early administration of sulfhydryl compounds, for example, methionine and N-acetylcysteine . [A35814]
How long does it take for acetaminophen to reach its peak?
[A35815] Peak blood levels of free acetaminophen are not reached until 3 hours after rectal administration of the suppository form of acetaminophen and the peak blood concentration is approximately 50% of the observed concentration after the ingestion of an equivalent oral dose (10-20 mcg/mL). [F4124] The percentage of a systemically absorbed rectal dose of acetaminophen is inconsistent, demonstrated by major differences in the bioavailability of acetaminophen after a dose administered rectally. Higher rectal doses or an increased frequency of administration may be used to attain blood concentrations of acetaminophen similar to those attained after oral acetaminophen administration. [Label]
How low does acetaminophen binding to plasma proteins?
The binding of acetaminophen to plasma proteins is low (ranging from 10% to 25%), when given at therapeutic doses.
What is acetaminophen test?
An acetaminophen test system is a device intended to measure acetaminophen, an analgestic and fever reducing drug, in serum. Measurements obtained by this device are used in the diagnosis and treatment of acetaminophen overdose.
How much of acetaminophen is bound to red blood cells?
Volume of distribution is about 0.9L/kg. 10 to 20% of the drug is bound to red blood cells. [A176357] Acetaminophen appears to be widely distributed throughout most body tissues except in fat. [Label]
How long does acetaminophen last?
The half-life for adults is 2.5 h after an intravenous dose of 15 mg/kg. [Label] After an overdose, the half-life can range from 4 to 8 hours depending on the severity of injury to the liver, as it heavily metabolizes acetaminophen. [A35815]
When was acetaminophen detected in Illinois?
Acetaminophen was detected, not quantified in four of eight secondary effluents from publicly-owned treatment works in Illinois, sampled from February to June, 1980 (1). It was not detected in effluent from an industrial plant sampled as part of this same study (1).
Where are the analgesic effects of APAP?
What does seem clearer is that the predominant mechanisms of APAP's analgesic effects are in the central nervous system (CNS). Although, which central effects are largely responsible for APAP's effects on pain continue to be uncertain.
Is APAP a pain reliever?
Acetaminophen (APAP) (paracetamol [PARA]) has been used clinically for over a half of a century and although clinicians seem to be comfortable with its benefits, risks, and limitations, they still remain in the dark as to precise ly what is providing its pain relief.
Does APAP affect serotonergic pathways?
Perhaps, the most accepted theory is that of APAP's positive effects on the serotonergic descending inhibitory pathways. However, interactions with opioidergic systems, eicosanoid systems, and/or nitric oxide containing pathways may be involved as well.
Is acetaminophen an analgesic?
Potential analgesic mechanisms of acetaminophen. Despite nearing the end of the decade of pain research, the analgesic mechanisms of one of the most widely used and popular analgesics remains uncertain.
Is APAP a paracetamol?
Acetaminophen (APAP) (paracetamol [PARA]) has been used clinically for over a half of a century and although clinicians seem to be comfortable wit …. Despite nearing the end of the decade of pain research, the analgesic mechanisms of one of the most widely used and popular analgesics remains uncertain. Acetaminophen (APAP) (paracetamol [PARA]) ...
Does paracetamol reduce inflammation?
Paracetamol also decreases PG concentrations in vivo, but, unlike the selective COX-2 inhibitors, paracetamol does not suppress the inflammation of rheumatoid arthritis. It does, however, decrease swelling after oral surgery in humans and suppresses inflammation in rats and mice. Paracetamol is a weak inhibitor of PG synthesis ...
Does paracetamol inhibit PG synthesis?
Paracetamol is a weak inhibitor of PG synthesis of COX -1 and COX-2 in broken cell systems, but, by contrast, therapeutic concentrations of paracetamol inhibit PG synthesis in intact cells in vitro when the levels of the substrate arachidonic acid are low (less than about 5 mumol/L).
Is paracetamol a weak inhibitor?
Mechanism of action of paracetamol. Paracetamol (acetaminophen) is generally considered to be a weak inhibitor of the synthesis of prostaglandins (PGs). However, the in vivo effects of paracetamol are similar to those of the selective cyclooxygenase-2 (COX-2) inhibitors.
Does paracetamol decrease PG?
Paracetamol also decreases PG concentrations in vivo, but, unlik …. Paracetamol (acetaminophen) is generally considered to be a weak inhibitor of the synthesis of prostaglandins (PGs). However, the in vivo effects of paracetamol are similar to those of the selective cyclooxygenase-2 (COX-2) inhibitors.
Which is better, ibuprofen or acetaminophen?
Acetaminophen works best for treating conditions such as arthritis, body aches, fever, and minor aches, while NSAIDs like ibuprofen are better suited for bigger headaches, menstrual cramps, toothaches, minor injuries, and inflammatory pain. Unlike NSAIDs, acetaminophen doesn’t have to be taken with food.
What are pain relievers?
Pain relievers, also known as analgesics, come in many forms, including NSAIDs, COX-2 inhibitors, acetaminophen, antidepress ants, and opioids. Some of these are available over-the-counter without a prescription. Researchers classify these medications based on the chemical reaction the medications trigger to relieve pain.
Is acetaminophen good for minors?
Acetaminophen is useful for minors aches and pains. Despite its widespread usage, we still don't know exactly how it works, but there are several promising hypotheses currently being investigated by the medical research community.
Is acetaminophen an over the counter pain reliever?
Acetaminophen is yet another over-the-counter pain reliever. As we’ll see, its mechanism of action differs significantly from NSAIDs and COX-2 inhibitors. As a result, it's useful for different kinds of pain and offers a different side effect profile than other over-the-counter medications.
Does acetaminophen block the central nervous system?
Scientists initially thought that acetaminophen blocked a hormone in the central nervous system ( 6 ). Later, they came to believe that acetaminophen reacted with a new COX enzyme called COX-3 ( 7 ). This hypothesis was debunked, however, by the results of subsequent experiments with animals ( 8 ).
Can you take acetaminophen orally?
All of these forms are taken orally, and you don’t need to eat food beforehand.
Can acetaminophen be used as a supplement?
Both acetamino phen and NSAIDs can lead to complications if used chronically ( 12 ). As long as you keep an eye on your daily limit of both NSAIDs and acetaminophen, and you have talked with your doctor, you can use these drugs as supplements.