
What are the elements of a SOAP note?
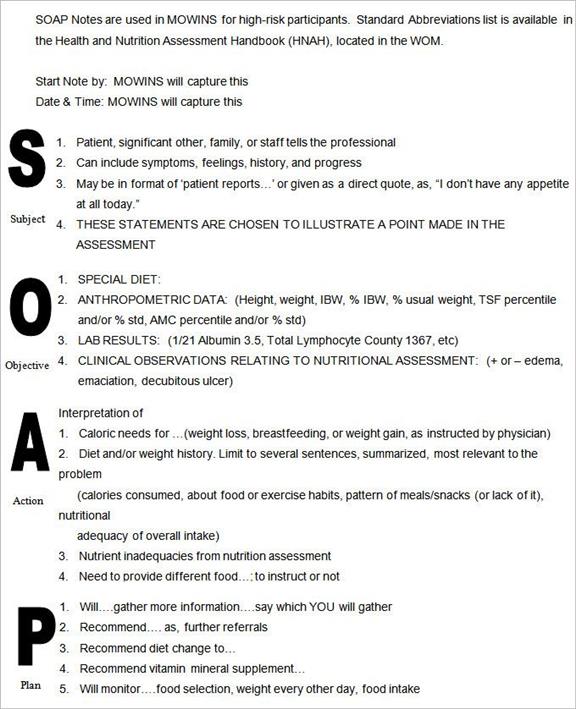
SOAP is an acronym that stands for subjective, objective, assessment, and plan. The elements of a SOAP note are: Subjective (S): Focused on the client's information regarding their experience and perceptions of symptoms, needs, and progress toward treatment goals.
What is the first heading of a SOAP note?
This is the first heading of the SOAP note. Documentation under this heading comes from the “subjective” experiences, personal views or feelings of a patient or someone close to them. In the inpatient setting, interim information is included here.
What are SOAP notes used for in medical billing?
It often meant that a client had to remember from visit to visit what they said to one doctor and then to another. Now, medical professionals use SOAP notes for this purpose. This type of note-taking system offers one clear advantage: consistent, clear information about each patient during each visit to a provider.
What is a weakness of the SOAP note?
A weakness of the SOAP note is the inability to document changes over time. In many clinical situations, evidence changes over time, requiring providers to reconsider diagnoses and treatments. An important gap in the SOAP model is that it does not explicitly integrate time into its cognitive framework.
What does the P in soap mean?
The Subjective, Objective, Assessment and Plan (SOAP) note is an acronym representing a widely used method of documentation for healthcare providers.
What does the P in soap stand for quizlet?
What does SOAP stand for? S=Subjective (something patient tells you) O=Objective (something clinician does to patient) A=Assessment (Putting info together, and figure out what it means) P=Plan (how to get the patient to their highest lvl of function)
How do you read a SOAP note?
0:436:33SOAP NOTES - YouTubeYouTubeStart of suggested clipEnd of suggested clipThe subjective section of your soap note should contain information gathered by talking to theMoreThe subjective section of your soap note should contain information gathered by talking to the patient. The family members and the medical record review depending. Upon the nature of the encounter.
What is the O in SOAP note?
The Objective (O) part of the note is the section where the results of tests and measures performed and the therapist's objective observations of the patient are recorded. Objective data are the measurable or observable pieces of information used to formulate the Plan of Care.
When it comes to injury assessment What does the P stand for in HOPS?
1. Differentiate between the history of the injury, observation and inspection, palpation, and special tests (HOPS) injury assessment format and the subjective evaluation, objective evaluation, assessment, and plan (SOAP) note format used to assess and manage musculoskeletal injuries. 2.
What does the acronym SOAP represent define the terms represented by each letter?
Subjective, Objective, Assessment, and Plan.
How do doctors write SOAP notes?
What's the SOAP note definition?Introduction:Record checklist details.Subjective:Document what the patient tells you.Objective:Document your observations of patient vital signs.Assessment:Document your assessment results.More items...•
How do you write a SOAP note in nursing?
0:105:59How to Make SOAP Notes Easy (NCLEX RN Review) - YouTubeYouTubeStart of suggested clipEnd of suggested clipUse the soap note as a documentation method to write out notes in the patient's chart. So stands forMoreUse the soap note as a documentation method to write out notes in the patient's chart. So stands for subjective objective assessment and plan let's take a look at each of the four components.
What is the subjective in a SOAP note?
SOAP is an acronym for: Subjective - What the patient says about the problem / intervention. Objective - The therapists objective observations and treatment interventions. (e.g. ROM, Outcome Measures)
Where does Ros go in SOAP note?
If the provider uses a subjective, objective, assessment, and plan (SOAP) documentation format, the ROS elements should appear under the heading “Subjective.”
What are 3 guidelines to follow when writing SOAP notes?
Tips for Effective SOAP NotesFind the appropriate time to write SOAP notes.Maintain a professional voice.Avoid overly wordy phrasing.Avoid biased overly positive or negative phrasing.Be specific and concise.Avoid overly subjective statement without evidence.Avoid pronoun confusion.Be accurate but nonjudgmental.
How long should a SOAP note be?
1-2 pagesYour SOAP notes should be no more than 1-2 pages long for each session. A given section will probably have 1-2 paragraphs in all (up to 3 when absolutely necessary).
What is soap quizlet?
A SOAP note is a documentation method employed by health care providers to create a patient's chart. There are four parts of a SOAP note: 'Subjective, Objective, Assessment, and Plan.
What is the benefit of using SOAP notes quizlet?
What is the benefit of using SOAP notes? Employees know where to look for information. How should subjective statements by the patient be documented?
What does O stand for in HOPS?
H.O.P.S. History, Observation, Palpation, Special Tests.
What is included in the assessment section of a SOAP note quizlet?
- The assessment section ( or interpretation of the data) is the MOST important section of the progress note. It should inform the reader about the effectiveness of the treatment plan and the progress the patient is making toward goals.
What is the purpose of a SOAP note?
SOAP notes are a clinical method used by healthcare professionals to simplify and organize a patient's information. Healthcare practitioners use the SOAP note format to record information in a consistent and structured way.
What is SOAP Note format?
SOAP is an acronym that stands for subjective, objective, assessment, and plan. The elements of a SOAP note are:
How do you write a SOAP note?
What are the four parts of a SOAP note? What should be included in a SOAP note assessment?
SOAP Note Examples
Ms. M. states that she has "been doing ok." Her depressive symptoms have improved slightly; however, she still often feels "low." Ms. M. says she is sleeping "well" and getting "7 hours sleep per night" She expresses concern with my note-taking, causing her to be anxious during the session.
Free SOAP notes templates
There are many free SOAP note templates available for download. These templates are typically in word or PDF format, so you can easily make changes to them.
Tips for Writing SOAP Notes
Here are our top tips on maximizing the value of SOAP notes regardless of your profession or clinical discipline.
Final thoughts
Whether you're an Nurse, Allied health practitioner, therapist, mental health worker, or medical professional, you'll spend less time creating better documentation with SOAP Notes. The best place to start is with free SOAP note software or with a SOAP note template.
What is a soap note?
SOAP refers to a common template healthcare providers use to document sessions or evaluations. Although different work settings include different information in their SOAP notes, the following are some general guidelines for what a SOAP note should (and should not) include.
Why do we need to take a soap note?
SOAP notes are a common way for healthcare and other teams to organize information they need to share with each other when they are working together or taking over where someone else left off. SOAP notes should be clear, well-written, and easy to follow so that your team can find the information they need.
What is the P section of a medical exam?
The P section is where you answer “Now what?” Knowing the information from the sections above, write your suggestions for treatment, referrals, resources recommended, and discharge plans. For an initial eval session, this may also include long-term and short-term goals. Remember that all information in this section should connect back to your 3 P’s and Needs from your A section.
What is the A section in a book?
The A section is where you describe and explain why things happened and what might be going on. This is the appropriate place for informed opinions, theories, explanation, and (last but not least) interpretations! The most important thing to remember is that the A section is where you make sense of what you wrote in the O section and S section. It should not include any new information, just like your O section should not include anything besides facts.
What is subjective S section?
Subjective means personal and not measurable. The S section is the place to report anything the client says or feels that is relevant to their session or case . This includes any report of limitations, concerns, and problems. Often living situations and personal history (ex. PMH or Occupational Profile) are also included in the S section. [NOTE: This does not include any answers to an evaluation or screening such as pain scale.]
What is a therapy soap note?
Therapy SOAP notes follow a distinct structure that allows medical and mental health professionals to organize their progress notes precisely. [1] As standardized documentation guidelines, they help practitioners assess, diagnose, and treat clients using information from their observations and interactions.
Why are soap notes important?
SOAP notes also play a valuable role in Applied Behavior Analysis, by allowing professionals to organize sessions better and communicate with a client’s other medical professionals. Legally, they may also accompany insurance claims to evidence the service being provided. [4]
How does software help with progress notes?
Many therapy software systems help to speed up the documentation of progress notes through in-built templates and diagnostic codes. At the end of the day, however, clinically valuable notes require careful thought and judgment when it comes to their content.
What format are therapy notes in?
Laid out in the S, O, A, P format on therapy notes software, they might look like this:
Why do we write notes immediately after therapy?
This way, a practitioner’s in-session time is spent focused on patient engagement and care; writing notes immediately after helps minimize common mistakes such as forgetting details or recall bias.
Is ABA SOAP a private document?
It is important to remember that ABA SOAP notes, as psychotherapeutic documents, must be stored privately. They may form part of a client’s overall medical file other therapy notes.
Can you make a soap note on the spot?
This way, notes can be made on the spot from a tablet or smartphone.
What are the components of a soap note?
Components of SOAP Note 1 Subjective. The subjective part details the observation of a health care provider to a patient. This could also be the observations that are verbally expressed by the patient. 2 Objective. All measurable data such as vital signs, pulse rate, temperature, etc. are written here. It means that all the data that you can hear, see, smell, feel, and taste are objective observations. If there are any changes regarding of the patient’s data, it will also be written here. 3 Assessment. The assessment is where the diagnoses of the patient are addressed and interpreted. The assessment plan should explain well the reason behind the decision to clarify the diagnoses expressed by the health care providers. 4 Plan. The plan refers to the treatment that the patient need or advised by the doctor. Such as additional lab test to verify the findings. The changes in the intervention are also written here.
Who Uses SOAP Notes?
As mentioned above, the SOAP note is widely used in medical industry. The SOAP note is used by physicians, clinicians, doctors, psychiatrists, and nurses. Medical interns also use a SOAP note to make them familiarize with the note and give them knowledge on how to use it.
What should a soap note start with?
Health care providers must follow the SOAP note format. It should start with the subjective, objective, assessment, and then the plan.
What is subjective part?
The subjective part details the observation of a health care provider to a patient. This could also be the observations that are verbally expressed by the patient. Objective. All measurable data such as vital signs, pulse rate, temperature, etc. are written here.
Is medical terminology allowed in a soap note?
Medical terminologies and jargon are allowed in the SOAP note. This is to make the note concise and coherent. However, the terminologies and jargon must be known to all health care providers.
What does SOAP stand for?
The acronym SOAP stands for Subjective, Objective, Assessment, and Plan. Each category is described below:
What does P mean in medical terminology?
P = Plan or Procedure . The initial plan for treatment should be stated in “P” section of the patient’s first visit. A complete treatment plan includes treatment frequency, duration, procedures, expected outcomes and goals of treatment.
What does O mean in a medical note?
O = Objective or observations . This section includes inspection (e.g., “ patient still walks with antalgic gait ”) as well as a more formalized reevaluations such ranges of motion, provocative tests, specialized tests (fixations, tongue, pulse, BP, labs). The extent of the reevaluation at each office visit is determined by the information gathered in “S” together with the original positive clinical findings as well as changes in “O” at previous office visits. Usually only the critical indictors need be repeated. Findings should be qualified and quantified in order to be able to ascertain progress/response to care over time. Indicators for treatment should always be identified in order to document necessity of the treatment provided and described in “Plan” section of the note, for example motion palpation findings, stagnation of blood and chi, or abnormal lab values.
What is the P component of a plan?
Other components of “A” may include the following where appropriate: patient risk factors or other health concerns, review of medications, laboratory or procedure results, and outside consultation reports. P = Plan or Procedure. The initial plan for treatment should be stated in “P” section of the patient’s first visit.
What is the S in a follow up note?
In follow-up notes, “S” is a reiteration of the chief complaints elicited during the initial evaluation of the patient. The complaints should reflect change over time.
What does P mean in a follow up visit?
On each follow-up visit, “P” should indicate modalities and procedures performed that day, continuation or changes in the overall treatment plan.
Why do medical professionals use soap notes?
This type of note-taking system offers one clear advantage: consistent, clear information about each patient during each visit to a provider. When the providers are part of the same group, this information can be easily shared.
Who created the soap notes?
SOAP notes are structured and ordered so that only vital and pertinent information is included. Initially developed by Larry Weed 50 years ago, these notes provide a “ framework for evaluating information [and a] cognitive framework for clinical reasoning ” (Gossman, Lew, & Ghassemzadeh, 2020).
Why Are SOAP Notes Important?
Cynthia Moreno Tuohy, executive director of the Association for Addiction Professionals, has highlighted the importance of quality SOAP notes for more than 40 years.
Why do we use soap notes?
SOAP notes are easy to use and designed to communicate the most relevant information about the individual . They can also provide documentation of progress.
What is a symptom in a note?
Symptoms are what the person tells you is going on physically, psychologically, and emotionally. They are the client’s subjective opinion and should be included in the “S” part of your notes.
What is subjective descriptor?
The descriptor ‘subjective’ comes from the client’s perspective regarding their experiences and feelings. It might also include the view of others who are close to the client.
