What to expect during pacemaker?
Possible risks of pacemaker include, but are not limited to, the following:
- Bleeding from the incision or catheter insertion site
- Damage to the vessel at the catheter insertion site
- Infection of the incision or catheter site
- Pneumothorax. If the nearby lung is inadvertently punctured during the procedure, leaking air becomes trapped in the pleural space (outside the lung but within the chest wall); this can cause ...
Is it possible to have malfunctioning pacemaker?
You can tell if your pacemaker is malfunctioning if you are starting to experience symptoms of arrhythmia. You might have chest pain, difficulty breathing, dizziness, or lightheadedness. There are several reasons why your pacemaker might stop working. These include the following: Your condition has changed and it needs to be reprogrammed.
What are the complications of a pacemaker?
Complications related to pacemaker surgery or having a pacemaker are uncommon, but could include: Infection near the site in the heart where the device is implanted; Swelling, bruising or bleeding ...
What is the intrinsic pacemaker of the heart?
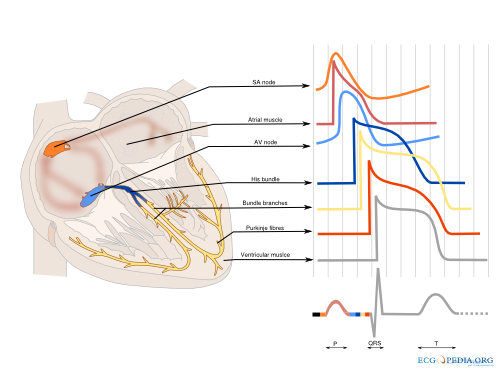
To coordinate these two tasks, the heart has an intrinsic pacemaker–i.e the sinus node –and an electrical conduction system composed of specialized myocardial cells. Conduction cells form bundles of fibers that spread the action potential rapidly and sequentially to the contractile myocardium.

How does pacemaker potential affect heart rate?
Since each pacemaker firing triggers a heartbeat, the steeper the pacemaker potential, the higher the heart rate. In pacemaker cells, the AP upstroke (phase 0) is generated by calcium currents, and not by sodium current as in the nonpacemaker tissues. Pacemaker APs do not have such a long plateau phase as ventricular myocytes. In contrast, after attaining the peak voltage, membrane potential immediately starts to return toward the diastolic level (phase 3). Thus pacemaker APs have only three phases; 4, 0 and 3.
What factors contribute to the pacemaker potential in nodal cells?
Several factors contribute to the pacemaker potential in nodal cells. Because of the very low density of IK1 channels in nodal cells, the resting K + permeability is much lower in nodal cells than in ventricular cells. The large resting K + permeability in ventricular cells generated by I K1 tends to keep the interior of the cells negative, opposing depolarization of the cell toward threshold by “clamping” the membrane potential near E K. A much smaller current is sufficient to depolarize the nodal cells due to the much lower resting K + permeability, leading to a very high input resistance. Thus, currents which may be too small to measure accurately using present electrophysiological techniques (small background currents or currents produced by various electrogenic transport mechanisms) could produce sufficient current to affect the pacemaker potential. Because of this limitation, the analysis of the relative contribution of various currents to the pacemaker potential in nodal cells is much less clear than for Purkinje cells, leading to considerable controversy regarding the precise mechanism of automaticity in SA node cells.
What is the action potential in a pacemaker cell?
When threshold is reached in a pacemaker cell, an action potential occurs. The upstroke of the action potential is quite slow compared with the rapid (phase 0) depolarization in a normal atrial or ventricular cell, because there are no fast, voltage-gated Na + channels in pacemaker cells and therefore no sudden influx of Na + upon reaching threshold. The ion primarily responsible for the action potential in a pacemaker cell is Ca 2+. When threshold is reached, many of the cell's slow Ca 2+ channels open. The permeability to Ca 2+ increases, and extracellular Ca 2+ flows into the cell. The action potentials in pacemaker cells are often called slow action potentials, because they lack a rapid, phase 0 depolarization and because they are caused primarily by the opening of slow Ca 2+ channels. In contrast, normal atrial or ventricular action potentials are called fast action potentials. Note, however, that all cardiac action potentials (whether “slow” or “fast”) have a very long duration compared with action potentials in nerve or skeletal muscle cells.
What is the upstroke of nodal cells?
As noted earlier, the upstroke (phase 0) of nodal cells is generated by an L-type Ca 2+ current (I Ca (L)) rather than a voltage-gated Na + current (I Na ). The channel responsible appears identical to the classic L-type Ca 2+ channel (Ca v 1.2) for the plateau in ventricular cells. Interestingly, in nodal cells, another I Ca (L) channel isoform (Ca v 1.3) has been reported that has a slightly more negative threshold (approximately −50 mV). This component of I Ca (L) is thought to contribute to the late phase of the pacemaker potential and effectively lower the threshold for I Ca (L) (for review, see Mangoni et al., 2003 ).
What is the depolarizing current in Purkinje cells?
The major depolarizing current during the pacemaker potential of Purkinje cells, I f, is also present in nodal cells. The hyperpolarization-activated cyclic nucleotide-gated (HCN) channels responsible for I f are encoded by four gene isoforms (HCN1–4) (for review, see Baruscotti et al., 2010 ). HCN2 and HCN4 are expressed in the heart, with HCN4 being the predominant isoform in the SA node. As noted earlier, I f is an unusual depolarizing current in that it is activated by hyperpolarization ( DiFrancesco, 1993 ). As a result, I f is thought to contribute significantly to the early part of the pacemaker potential in SA node cells.
How do vagal efferents affect heart rate?
Vagal efferents originating mainly in the nucleus ambiguus, but some in the dorsal motor nucleus of the vagus in the medulla, inhibit the heart rate by reducing the slope of the pacemaker potential in SA nodal cells. Baroreceptors tonically activate cells in the NTS, and this tonic excitation is relayed to the nucleus ambiguus where vagal efferents are tonically active. Thus in humans there is a constant vagal tone that continuously inhibits the heart rate. Reductions in blood pressure relieve this tonic inhibition, thereby accelerating the heart rate by removing parasympathetic tone. This completes a negative feedback loop: the accelerated heart rate increases the cardiac output and tends to restore the blood pressure. When blood pressure rises, the reverse occurs: NTS stimulates the NA more and there is greater vagal inhibition of heart rate (see Figure 5.13.5 ).
What are the properties of cultured heart cells?
These reverted cells are helpful for examining certain myocyte properties such as changes in type of cation channels, K + permeability, and the electrogenesis of pacemaker potentials. Reaggregated cultured heart cells can be prepared that retain highly differentiated electrical properties and their normal pharmacological receptors. Simultaneous monitoring of transmembrane potentials and contractions can be made on single cells by using appropriate microelectrode and photoelectric techniques. Since the cells are denervated, the direct effect of various chemicals and pharmacological agents on the myocyte can be evaluated without involvement of neural and systemic influences.
What factors contribute to the pacemaker potential in nodal cells?
Several factors contribute to the pacemaker potential in nodal cells. Because of the very low density of IK1 channels in nodal cells, the resting K + permeability is much lower in nodal cells than in ventricular cells. The large resting K + permeability in ventricular cells generated by I K1 tends to keep the interior of the cells negative, opposing depolarization of the cell toward threshold by “clamping” the membrane potential near EK. A much smaller current is sufficient to depolarize the nodal cells due to the much lower resting K + permeability, leading to a very high input resistance. Thus, currents which may be too small to measure accurately using present electrophysiological techniques (small background currents or currents produced by various electrogenic transport mechanisms) could produce sufficient current to affect the pacemaker potential. Because of this limitation, the analysis of the relative contribution of various currents to the pacemaker potential in nodal cells is much less clear than for Purkinje cells, leading to considerable controversy regarding the precise mechanism of automaticity in SA node cells.
What is the pathological condition of a pacemaker?
The existence of an alternative, albeit slower pacemaker is revealed in a pathological condition called ‘heart block’ , in which there is a blockage of the normal electrical connection across the annulus fibrosus.
What is the action potential of ventricular cardiocytes?
In ventricular cardiocytes, the membrane potential at rest remains near E K. Activation from pacemaker cells via the conduction system can stimulate another action potential. An excitatory stimulus or pacemaker potential that depolarizes the cell membrane beyond its threshold potential (∼−70 mV) triggers an intricately woven cascade of channel openings and closings that generates the ventricular action potential shown in Figure 18-3B. The fast upstroke in atrial and ventricular cells is accomplished by Na + channels (I Na ). Once the threshold potential of −70 mV is reached, Na + channels are activated, resulting in an enormous (>−380 microamps/microfarad) albeit brief (<5 msec) inward Na + current. I Na is 50 to 1000 times larger in net conductance than any other population of ion channels. The depolarizing current carried by the influx of sodium drives the cell toward E Na. More Na + channels are opened as the current peaks at −20 mV, producing the regenerative depolarization responsible for the propagation of the cardiac action potential.
What is the upstroke of nodal cells?
As noted earlier, the upstroke (phase 0) of nodal cells is generated by an L-type Ca 2+ current (I Ca (L)) rather than a voltage-gated Na + current (I Na ). The channel responsible appears identical to the classic L-type Ca 2+ channel (Ca v 1.2) for the plateau in ventricular cells. Interestingly, in nodal cells, another I Ca (L) channel isoform (Ca v 1.3) has been reported that has a slightly more negative threshold (approximately −50 mV). This component of I Ca (L) is thought to contribute to the late phase of the pacemaker potential and effectively lower the threshold for I Ca (L) (for review, see Mangoni et al., 2003 ).
What is the depolarizing current in Purkinje cells?
The major depolarizing current during the pacemaker potential of Purkinje cells, I f, is also present in nodal cells. The hyperpolarization-activated cyclic nucleotide-gated (HCN) channels responsible for I f are encoded by four gene isoforms (HCN1–4) (for review, see Baruscotti et al., 2010 ). HCN2 and HCN4 are expressed in the heart, with HCN4 being the predominant isoform in the SA node. As noted earlier, I f is an unusual depolarizing current in that it is activated by hyperpolarization ( DiFrancesco, 1993 ). As a result, I f is thought to contribute significantly to the early part of the pacemaker potential in SA node cells.
How do vagal efferents affect heart rate?
Vagal efferents originating mainly in the nucleus ambiguus, but some in the dorsal motor nucleus of the vagus in the medulla, inhibit the heart rate by reducing the slope of the pacemaker potential in SA nodal cells. Baroreceptors tonically activate cells in the NTS, and this tonic excitation is relayed to the nucleus ambiguus where vagal efferents are tonically active. Thus in humans there is a constant vagal tone that continuously inhibits the heart rate. Reductions in blood pressure relieve this tonic inhibition, thereby accelerating the heart rate by removing parasympathetic tone. This completes a negative feedback loop: the accelerated heart rate increases the cardiac output and tends to restore the blood pressure. When blood pressure rises, the reverse occurs: NTS stimulates the NA more and there is greater vagal inhibition of heart rate (see Figure 5.13.5 ).
Why does a seal's heart rate drop during a dive?
The seal's heart rate can fall to 20 beats/min during a dive, owing to vagal inhibition of the pacemaker potential. Many human subjects display a pronounced bradycardia during facial immersion in cold water (see Figure 14.8), and facial immersion in cold water has even been used successfully to interrupt human supraventricular tachycardias.
How does the pacemaker potential work?
The pacemaker potential is achieved by activation of hyperpolarisation activated cyclic nucleotide gated channels (HCN channels). These allow Na+ entry into the cells, enabling slow depolarisation. These channels are activated when the membrane potential is lower than -50mV. Once the membrane potential gets depolarised to reach the threshold, an action potential can be fired.
Which system alters the slope of the pacemaker potential in order to alter heart rate?
The autonomic nervous system (ANS) alters the slope of the pacemaker potential, in order to alter heart rate.
What causes arrhythmias in the heart?
Causes of arrhythmias include: 1 Ectopic Pacemaker Activity: This is when another area of the myocardium becomes spontaneously active and its depolarisations dominate over the SA node. A latent pacemaker region can become activated due to ischaemic damage. 2 After-Depolarisations: This is when abnormal depolarisations follow the action potential – thought to be caused by high intracellular Ca 2+. 3 Re-entry loop: This occurs when the normal spread of excitation across the heart is disrupted due to a damaged area. When the conduction damage is incomplete, it allows the impulse to spread the wrong way through the damaged area and create a circle of excitation. Multiple small re-entry loops can occur in the atria, leading to atrial fibrillation.
What happens to HCN channels at the peak of the action potential?
HCN channels then start to inactivate. At the peak of the action potential, Ca 2+ channels inactivate, and K + channels open.
What is after depolarization?
After-Depolarisations: This is when abnormal depolarisations follow the action potential – thought to be caused by high intracellular Ca 2+.
What is the term for a heartbeat with an irregular rate and/or rhythm?
Disturbance to the natural pacemaker activity of the heart can lead to arrhythmias i.e. a heartbeat with an irregular rate and/or rhythm.
What is the intrinsic heart rate?
If all autonomic inputs are blocked, the intrinsic heart rate is about 100 beats per minute (bpm). The normal resting rate of about 60bpm is produced because the parasympathetic system dominates at rest. Initial increases in heart rate are brought about by a reduction in the parasympathetic outflow.
Why do you need a pacemaker?
A pacemaker is a small device that's placed under the skin in your chest to help control your heartbeat. It's used to help your heart beat more regularly if you have an irregular heartbeat (arrhythmia), particularly a slow one. Implanting a pacemaker in your chest requires a surgical procedure.
Why do pacemakers help with fatigue?
Because most of today's pacemakers automatically adjust the heart rate to match the level of physical activity , they may can allow you to resume a more active lifestyle.
How many wires are in a pacemaker?
Depending on your condition, you may have a pacemaker with one to three flexible, insulated wires (leads) placed in a chamber, or chambers, of your heart. These wires deliver the electrical pulses to adjust your heart rate. Pacemakers are implanted to help control your heartbeat. They can be implanted temporarily to treat a slow heartbeat ...
What is a biventricular pacemaker?
Biventricular pacemaker. Biventricular pacing, also called cardiac resynchronization therapy, is for people with heart failure with abnormal electrical systems. This type of pacemaker stimulates the lower chambers of the heart (the right and left ventricles) to make the heart beat more efficiently.
What is a pacemaker called?
A pacemaker is also called a cardiac pacing device.
How long does it take to get a pacemaker implanted?
You'll likely be awake during the surgery to implant the pacemaker, which typically takes a few hours. You'll have an intravenous line placed, through which you might receive medication to help you relax.
What is a pulse generator?
Pulse generator. This small metal container houses a battery and the electrical circuitry that controls the rate of electrical pulses sent to the heart.
Why do you need a pacemaker?
A pacemaker may be inserted in order to stimulate a faster heart rate when the heart is beating too slowly, and causing problems that cannot otherwise be corrected. Problems with the heart rhythm may cause difficulties because the heart is unable to pump an adequate amount of blood to the body.
What is a pacemaker insertion?
A pacemaker insertion is the implantation of a small electronic device that is usually placed in the chest (just below the collarbone) to help regulate slow electrical problems with the heart. A pacemaker may be recommended toensure that the heartbeat does not slow to a dangerously low rate.
What type of pacemaker is used for heart failure?
A newer type of pacemaker, called a biventricular pacemaker, is currently used in the treatment of specific types of heart failure.
What is the treatment for a heart failure that causes less blood to be pumped?
This type of treatment is called cardiac resynchronization therapy or CRT.
What are the parts of a pacemaker?
A pacemaker is composed of three parts: a pulse generator, one or more leads, and an electrode on each lead. A pacemaker signals the heart to beat when the heartbeat is too slow or irregular.
How long does it take to recover from a pacemaker?
You should be able to return to your daily routine within a few days. Your doctor will tell you if you will need to take more time in returning to your normal activities. You should not do any lifting or pulling on anything for a few weeks. You may be instructed to limit movement of the arm on the side that the pacemaker was placed, based on your doctor's preferences.
What is alternating fast and slow heartbeats?
This is characterized by alternating fast and slow heartbeats. Heart block. This occurs when the electrical signal is delayed or blocked after leaving the SA node; there are several types of heart blocks. There may be other reasons for your doctor to recommend a pacemaker insertion.

Overview
Why It's Done
Risks
- Complications related to pacemaker surgery or having a pacemaker are uncommon, but could include: 1. Infection near the site in the heart where the device is implanted 2. Swelling, bruising or bleeding at the pacemaker site, especially if you take blood thinners 3. Blood clots (thromboembolism) near the pacemaker site 4. Damage to blood vessels or nerves near the pac…
How You Prepare
- Before your doctor decides if you need a pacemaker, you'll have several tests done to find the cause of your irregular heartbeat. Tests done before you get a pacemaker could include: 1. Electrocardiogram (ECG or EKG). This quick and painless test measures the electrical activity of the heart. Sticky patches (electrodes) are placed on the chest and sometimes the arms and legs…
What You Can Expect
- Before the procedure
You'll likely be awake during the surgery to implant the pacemaker, which typically takes a few hours. A specialist will insert an IV into your forearm or hand and give you a medication called a sedative to help you relax. Your chest is cleaned with special soap. Most pacemaker implantatio… - During the procedure
One or more wires are inserted into a major vein under or near your collarbone and guided to your heart using X-ray images. One end of each wire is secured at the appropriate position in your heart, while the other end is attached to the pulse generator, which is usually implanted under th…
Results
- Having a pacemaker should improve symptoms caused by a slow heartbeat such as fatigue, lightheadedness and fainting. Because most of today's pacemakers automatically adjust the heart rate to match the level of physical activity, they may can allow you to resume a more active lifestyle. Your doctor should check your pacemaker every 3 to 6 months. Te...
Clinical Trials
- Explore Mayo Clinic studiesof tests and procedures to help prevent, detect, treat or manage conditions.