The axial wall is the internal wall formed by the surface of the long axis (axial or vertical plane) of the tooth. The pulpal wall is the internal wall in the horizontal plane." If it's in the horizontal plane...it must be the same thing as the pulpal floor, just another name for it.
Full Answer
What is the pulpal response?
Pulpal Reactions to Caries and Dental Procedures The dental pulp is a dynamic tissue that responds to external stimuli in many ways. However, there are certain unique features about the dental pulp response that distinguish it from other connective tissues in the body.
What is the role of magnification in the evaluation of pulpal cracks?
Magnification is paramount for aiding in evaluation of the extent of the crack. The crack may be visualized extending along the pulpal floor from mesial to distal. Extending the pulpal floor to “follow” the crack apically can provide information on depth and nerve proximity.
Do consistent patterns of anatomy exist in the pulp-chamber floor?
Therefore, the only way to provide the best environment for success is to establish the full extent of the root-canal system. This study showed that consistent patterns of anatomy of both the chamber and the pulp-chamber floor exist. These consistent patterns were analyzed and from them laws were proposed.
What is the role of pulp testing in pulpal inflammation?
Thermal pulp testing is valuable for reproducing a symptom of thermal sensitivity and allowing the practitioner to assess the reaction of the patient to a stimulus and the duration of the response. However, pulp testing cannot determine the degree of pulpal inflammation.
How many books are in Pathways of the Pulp?
What is gingival bevel?
What to use to smooth a baby's floor?
Is a gingival bevel for Class II amalgam bad?
About this website
What is the pulpal floor of a tooth?
The bottom line. Your tooth pulp is the innermost layer of your tooth that contains nerves and blood vessels. Your tooth pulp is protected by layers of dentin and enamel.
What is floor of pulp chamber?
Law of centrality: the floor of the pulp chamber is always located. in the center of the tooth at the level of the CEJ (Figs. 1–3). Law of concentricity: the walls of the pulp chamber are always. JOURNAL OF ENDODONTICS.
What is the floor of the tooth?
The pulp is the connective tissue, nerves, blood vessels, and odontoblasts that comprise the innermost layer of a tooth.
What is a pulpal?
Introduction. The pulp is a mass of connective tissue that resides within the center of the tooth, directly beneath the layer of dentin. Referred to as part of the “dentin-pulp” complex, and also known as the endodontium, these two tissues are closely interrelated and dependent on each other's development and survival.
How deep is the pulp in a tooth?
The height of a pulp chamber is between 1.5 to 2.0 mm (Figure 5a). This 1.5-mm to 2.0-mm measurement is the most variable due to calcifications because of aging, caries, and restorations.
How many pulp chambers are there?
There is one pulp chamber in each tooth. It may be located partly in the crown of anterior teeth, but in posterior teeth, it is mostly in the cervical part of the root. Its walls are the innermost surface of the dentin.
How many mm deep is the pulp?
The average distance of the pulp chamber's floor from the furcation was found to be 2.47 ± 0.11 mm.
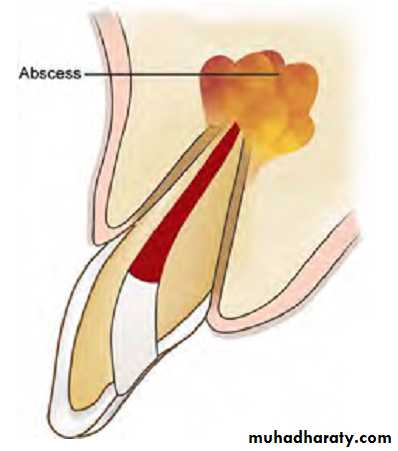
What is the most common symptom of pulpal damage?
The most common symptoms of damaged pulp include pain in your tooth, and swelling and a sensation of heat in your gums. Your dentist will examine the painful tooth and take X-rays to confirm the diagnosis.
What forms dental pulp?
The dental pulp develops from the neural crest cells in the fetus which condense to form the dental papilla. The mature pulp has a layer of highly specialized cells called odontoblasts that lie around the outer borders of the pulp. The dental pulp itself has a rich supply of blood vessels and nerves.
Can a tooth survive without pulp?
This tissue contains blood vessels, nerves and connective tissue, which help grow the root of your tooth during its development. A fully developed tooth can survive without the pulp because the tooth continues to be nourished by the tissues surrounding it.
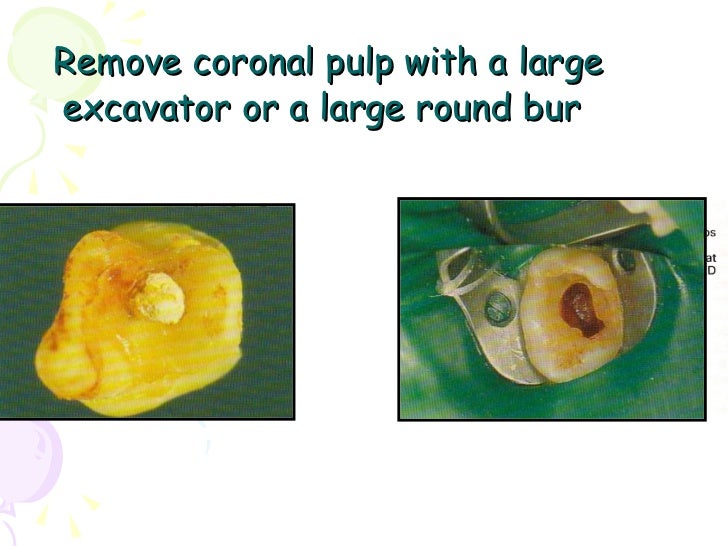
Is pulp removed during root canal?
Root canal treatment is a dental procedure that relieves pain caused by an infected or abscessed tooth. During the root canal process, the inflamed pulp is removed. The surfaces inside the tooth are then cleaned and disinfected, and a filling is placed to seal the space.
What is the term for the deepest layer of the tooth?
Teeth are made up of different layers — enamel, dentin, pulp, and cementum. Enamel, which is the hardest substance in the body, is on the outside of the tooth. The second layer is dentin, which is softer than enamel, and the deepest layer inside the tooth is pulp, which consists of nerves and blood vessels.
Why pulp chamber is darker?
The junction of pulp chamber floor and walls was marked by the former being a darker colour. Root canal orifices were always at this junction, at its angles, and at the terminus of developmental root fusion lines where these were present. Such fusion lines were darker than the pulp chamber floor.
What is Odontoblast cell?
Odontoblasts are specialized cells that produce dentin and exhibit unique morphological characteristics; i.e., they extend cytoplasmic processes into dentinal tubules.
What is the axial wall of tooth?
AXIAL WALL-An axial wall is an internal wall parallel with the long axis of the tooth. • PULPAL WALL-A pulpal wall is an internal wall that is perpendicular to the long axis of the tooth and occlusal of the pulp.
Where is the root canal located?
A root canal is the naturally occurring anatomic space within the root of a tooth. It consists of the pulp chamber (within the coronal part of the tooth), the main canal(s), and more intricate anatomical branches that may connect the root canals to each other or to the surface of the root.
Why is pulpal blood flow important?
An intact pulpal blood flow is critical for maintaining the health of the dental pulp. Because the dental pulp is enclosed in a rigid chamber and is supplied by few arterioles through the apical foramina, it cannot benefit from collateral circulation or volumetric changes that compensate for changes in blood flow in other soft tissues. Furthermore, reduction in blood flow has the compounding effect of reducing the clearance of large molecular weight toxins or waste products, thus causing irreversible pulpal pathosis. Vasoconstrictors are added to local anesthetics to enhance the duration of anesthesia. However, vasoconstrictors in local anesthetics could negatively impact the health of the pulp if they reduce blood flow, particularly if the pulp is inflamed preoperatively. Earlier studies have documented that vasoconstrictors in local anesthetics do reduce pulpal blood flow in experimental animals when administered by infiltration and nerve block ( Fig. 13-12 ), and that this effect was more severe with periodontal ligament injections ( Fig. 13-13 ). More recently, clinical trials were conducted in which subjects were given infiltration of different local anesthetics with or without epinephrine at a concentration of 1 : 100,000 and the pulpal blood flow was measured by laser Doppler flowmetry. In groups that received the epinephrine, there were consistently significant reductions in pulpal blood flow, even if the infiltration was palatal to maxillary premolars. Interestingly, in one study the reduction in pulpal blood flow with epinephrine infiltration was more than the reduction in gingival blood flow and did not return to baseline values after 1 hour of injection. Similar reductions in pulpal blood flow were reported when inferior alveolar nerve block injections of lidocaine and 1 : 100,000 or 1 : 80,000 epinephrine were administered. It is important to note a limitation of studies using laser Doppler flowmetry, which is that a large proportion of the signal measured may be from sources other than the dental pulp. Thus, the monitoring of minor changes in pulpal blood flow must be interpreted with caution, particularly if the rubber dam or a similar barrier was not used. Human studies on the effects of periodontal ligament or intraosseous injections on pulpal blood flow are not available, but from animal studies it is probable that these supplemental anesthetic techniques cause a more severe reduction or even transient cessation of pulpal blood flow. It was also shown that intraosseous injection of Depo-Medrol™ (a corticosteroid) in patients with symptomatic irreversible pulpitis causes a significant reduction of prostaglandin E2 in the pulp 1 day after administration, indicating that this route of injection results in significant permeation into the pulpal tissues. Taken together, these findings suggest that local anesthesia with vasoconstrictors may compromise the inflamed pulp’s ability to recover from inflammation, particularly if it is severely inflamed, or if the tooth is subjected to extensive restorative procedures, and if the anesthetic is delivered via a periodontal ligament or an intraosseous route. However, it is important to realize that this hypothesis should be supported or refuted by prospective randomized clinical trials.
What is the pulp response?
The dental pulp is a dynamic tissue that responds to external stimuli in many ways. However, there are certain unique features about the dental pulp response that distinguish it from other connective tissues in the body. The pulp’s exposure to dental caries, a prevalent chronic infectious disease, its encasement in an unyielding environment after complete tooth maturation, and the scarcity of collateral circulation render it susceptible to injury and complicate its regeneration. Moreover, the pulp is endowed with a rich neurovascular supply that regulates the effects of inflammation that may ultimately lead to rapid degeneration and necrosis. The treatment of dental caries and other tooth abnormalities involves removal of the enamel and dentin, the hardest tissues in the body, thus adding to the irritation of the pulp. This chapter discusses the response of the pulp to all of these variables and presents advances in our understanding of dental procedures and their effects on the pulp.
What are the effects of restorative materials on the pulp?
The effects of restorative materials on the dental pulp have been investigated and seem to relate directly to the permeability of the associated dentin. The degree of dentin permeability, however, is often variable and is governed by several factors including age and caries status. The most important variable in dentin permeability to restorative materials is the thickness of dentin between the floor of the cavity preparation and the pulp.
What are the effects of dental caries on the pulp?
Three basic reactions tend to protect the pulp against caries: (1) a decrease in dentin permeability, (2) tertiary dentin formation, and (3) inflammatory and immune reactions. These responses occur concomitantly, and their robustness is highly dependent on the aggressive nature of the advancing lesion as well as host responses such as the age of the patient (see also Chapter 26 ).
Why is the pulp of the tooth compromised?
As stated previously, the dental pulp is compromised in its ability to respond to external irritants because it is enclosed in a noncompliant environment and because it lacks collateral circulation. Thus, the more severe the pulp is inflamed, the less will be its ability to respond to further irritation, such as in the form of restorative procedures.
How does dentin permeability affect pulp?
The permeability of dentin plays an important role in the ingress of potential irritants to the pulp. It is clear from research done since the 1980s that dentin is not uniformly permeable and that permeability depends on factors such as the location within the same tooth, the age of the patient, and the presence of pathologic conditions such as dental caries. Fundamentally, the permeability of dentin depends on the collective sum of the permeability of individual tubules at a particular site in the tooth. The tubular diameter increases from about 0.6 to 0.8 µm close to the DEJ to about 3 µm at the pulp. Given that bacterial cells are about 0.5 to 1 µm in diameter, it is evident that in deep cavity preparations, particularly when total-etch procedures are employed, bacteria can migrate through the remaining dentin into the pulp.
Does age affect resting pulpal blood flow?
Resting pulpal blood flow (PBF), as well as the changes in PBF in response to cold application, will decrease with age. Age may also be associated with reduction in pulpal neuropeptides. However, studies show no differences between young and old pulp in the regenerative capacity of odontoblast-like cells and in the presence of cells positive for class II major histocompatibility complex, heat shock protein 25, or nestin, when subjected to cavity preparation. An examination of young versus old normal human pulp showed that young pulp had increased expression of biologic factors related to cell differentiation, proliferation, and the immune response, whereas older pulp had increased factors related to apoptosis. These analyses cannot translate to the pulp’s ability to deal with irritation and its sequelae. Thus, the net result of the ability of the pulp to cope with external stimulation or irritation in humans with advancing age is not clear.
Craze lines
Craze lines are micro-fractures of the enamel only. They may also be termed enamel infractions. The micro-fractures are contained within the enamel only. They do not penetrate into the dentin layer.
Fractured cusp
Fractured cusp is defined as a complete or incomplete fracture of the crown of the tooth extending subgingivally. The extent and degree of the fractured cusp is variable. The most common cuspal areas to fracture are the lingual cusps of the lower molars and the buccal cusps of the upper molars.
Cracked tooth
A cracked tooth is defined as an incomplete fracture initiated from the crown and extending subgingivally. The crack is usually in a mesial-distal direction. The crack may extend through one marginal ridge or may extend through both proximal surfaces. The vertical depth of the crack is also variable.
Split Tooth
"Split tooth" is defined as the complete fracture initiated from the crown extending subgingivally. It typically extends through both marginal ridges and the proximal surfaces to the proximal root. A split tooth is the end result of a cracked tooth (evolution)! The tooth segments are entirely separated.
Vertical Root Fracture
A vertical root fracture is a complete or incomplete fracture of the root in a buccal lingual direction. The fracture may extend the length of the root or as a shorter segment along any portion of the root. There may or may not be patient symptoms associated with the fracture. Many times they are discovered on routine periapical x-rays.
How many books are in Pathways of the Pulp?
19 alone from Pathways of the Pulp, 61 from Sturdevant's Art and Science of Operative, 8 from Fundamentals of Pediatric Dentistry, 4 from Fundamentals of Prostho., and between 1-3 from ~30 other books.
What is gingival bevel?
It is to compensate for the inverted direction of the enamel rods as the enamel reaches the end of the anatomic crown. It is very slight and you do have to be careful that you don't make a ski slope that will weaken the restoration, but it does seem logical not to leave all that unsupported enamel.
What to use to smooth a baby's floor?
Use a margin trimmer or hatchet to smooth the floor and fill that baby up.
Is a gingival bevel for Class II amalgam bad?
I think a gingival bevel for Class II amalgam is a particularly bad idea. Last time I checked, cavosurface angles for amalgam restorations should be darn near 90 degrees. That thin little lip of amalgam on the bevelled gingival floor is going to chip off and allow you to charge your patient another 80 bucks to do another restoration in the same spot in a few years.