Full Answer
What is the purpose of a health information exchange?
Health Information Exchange allows health care professionals and patients to appropriately access and securely share a patient’s medical information electronically. There are many health care delivery scenarios driving the technology behind the different forms of health information exchange available today.
What are the different types of health information exchange?
Directed Exchange: This type of health information exchange allows medical professionals the ability to send and receive secure documentation over the internet using secure, encrypted messaging. Using this method, information that can be shared includes lab results, discharge summaries, patient referrals, and more.
What is directed exchange in health care?
Directed Exchange: Directed exchange gives health care providers the ability to electronically send and receive secure information – such as such as laboratory orders and results, patient referrals, or discharge summaries – to other health care providers involved in a patient’s care over the Internet via encrypted, secure, and reliable messaging.
What is an example of information exchange?
This form of information exchange enables coordinated care that benefits both clinicians and patients. A primary care clinician can, for example, directly send electronic care summaries that include medications, problems, and lab results to a specialist when referring their patients. This information helps to inform the visit and prevents:

What are the forms of health information exchange?
Three forms of HIE currently exist, each providing a different type of access to health information and in a different manner.Directed Exchange. Through directed exchange, health care providers can simply and securely share patient data with other providers directly. ... Query-Based Exchange. ... Consumer-Mediated Exchange.
What are the 6 components of a health information system?
Part 2: Components and Standards of a Health Information System – describes the components and standards of a health information system, as shown in the left-hand column of Fig. 1. These are health information system resources, indicators, data sources, data management, information products, and dissemination and use.
How many forms of health information exchange are there?
three key formsThere are currently three key forms of health information exchange (HIE):
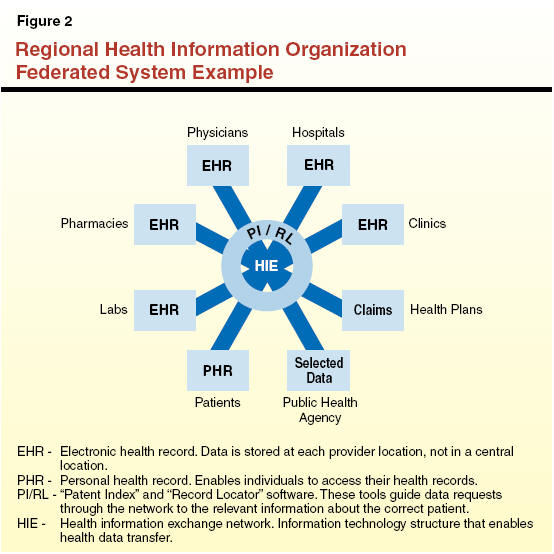
What is HIE architecture?
A true HIE involves multi-directional flow of information electronically between providers (hospitals, physicians, clinics, labs) and other sources of administrative or clinical information provided by consumers, health plans, employers, local, state or national organizations.
What are the 5 main components of an information system?
5 Components of Information SystemsComputer hardware. This is the physical technology that works with information. ... Computer software. The hardware needs to know what to do, and that is the role of software. ... Telecommunications. ... Databases and data warehouses. ... Human resources and procedures.
What are the 5 primary components of an information system?
An information system is essentially made up of five components hardware, software, database, network and people. These five components integrate to perform input, process, output, feedback and control. Hardware consists of input/output device, processor, operating system and media devices.
What are the 3 exchanges?
The New York Stock Exchange is the largest stock exchange in the world, with an equity market capitalization of just over 24.1 trillion U.S. dollars as of August 2022. The following three exchanges were the NASDAQ, the Shanghai Stock Exchange, and the Euronext. What is a stock exchange?
What are the functions of health information exchange?
Electronic health information exchange (HIE) allows doctors, nurses, pharmacists, other health care providers and patients to appropriately access and securely share a patient's vital medical information electronically—improving the speed, quality, safety and cost of patient care.
What are the 3 three fundamental components of the health information technology structure?
The components of a national health information infrastructure can be divided into three interrelated categories: (1) health care data standards and technical infrastructure; (2) core clinical applications, including EHRs, CPOE systems, digital sources of medical knowledge, and decision-support tools; and (3) ...
What are the 2 types of HIE data models?
The hybrid HIE model The most common structure for a health information exchange combines both the centralized and federated model into a hybrid structure.
Which of the following are models of HIE?
This report will analyze the three key HIE models: centralized, decentralized, and hybrid, and explain why the last approach should be applied and how to extract data using this model. The various types of HIE models include centralized, decentralized, and hybrid.
How are health information exchanges funded?
Authorized by the HITECH Act, the federal government covers 90% of administrative funding for HIE activities, while states cover the remaining 10%. The funding assists with incorporating providers into the state's HIE and making infrastructure improvements.
What is the main components of health information system?
Health information system resources: These consist of the legislative, regulatory, and planning frameworks required to ensure a fully functioning HIS and the resources that are required for such a system to be functional, such as personnel, financing, information and communications technology (ICT) etc.
What are the 6 categories of information?
6 types of informationConceptual information. Conceptual information comes from ideas, theories, concepts, hypotheses and more. ... Procedural information. ... Policy information. ... Stimulatory information. ... Empirical information. ... Directive information.
What are the components of a health system?
Instead, it is structured around the WHO framework that describes health systems in terms of six core components or “building blocks”: (i) service delivery, (ii) health workforce, (iii) health information systems, (iv) access to essential medicines, (v) financing, and (vi) leadership/governance (see Figure 1).
What are the 7 health components?
The Seven Dimensions of WellnessPhysical.Emotional.Intellectual.Social.Spiritual.Environmental.Occupational.
What is HIE exchange?
There are currently three key forms of health information exchange (HIE): 1 Directed Exchange: Directed exchange gives health care providers the ability to electronically send and receive secure information – such as such as laboratory orders and results, patient referrals, or discharge summaries – to other health care providers involved in a patient’s care over the Internet via encrypted, secure, and reliable messaging. 2 Query-Based Exchange: Query-based exchange gives health care providers the ability to find and/or request information on a patient from other providers and is often used for unplanned/emergency care. 3 Consumer Mediated Exchange: Consumer Mediated Exchange gives patients the ability to aggregate and manage their health information on the Internet. When in control of their own health information, patients can help transfer information between providers, correct inaccurate demographic, medical, or billing information, and track and monitor their own health.
What is a query based exchange?
Query-Based Exchange: Query-based exchange gives health care providers the ability to find and/or request information on a patient from other providers and is often used for unplanned/emergency care.
What is being done to improve health information exchange and advance interoperability?
To address these challenges and improve health information exchange — most notably, in relation to nationwide interoperability and information blocking — Congress passed the 21st Century Cures Act of 2016 (known as “the Cures Act”) with bipartisan support.
What is the Trusted Exchange Framework and Common Agreement (TEFCA)?
The Trusted Exchange Framework and the Common Agreement will outline a policy and technical approach for nationwide electronic health information exchange. TEFCA is mandated as part of the 21st Century Cures Act. Once finalized, it will allow clinicians and other healthcare providers to access patient health data from a variety of health information networks (HINs).
How do Application Programming Interfaces (APIs) support health information exchange and interoperability?
Online and smart phone banking are enabled by APIs. APIs can also help healthcare professionals improve and simplify care delivery in a number of ways .
What is SAFR in EMS?
Overview#N#Explains how health information exchange services can give EMS clinicians the ability to use full Search, Alert, File, Reconcile (SAFR) functionality. Also includes statistics related to the benefits of, and opportunities for, health information exchange
What is TEFCA in healthcare?
TEFCA is mandated as part of the 21st Century Cures Act. Once finalized, it will allow clinicians and other healthcare providers to access patient health data from a variety of health information networks (HINs).
Why do healthcare professionals send information over the internet?
Healthcare professionals, who already know and trust each other, send this information over the internet in an encrypted, secure, and reliable way; it’s commonly compared to sending a secured email. This form of information exchange enables coordinated care that benefits both clinicians and patients.
What is an overview#N#A fact sheet?
Overview#N#A fact sheet on how the use of EHR and health information exchange services among behavioral-health and physical-care teams encourages the bi-directional exchange of critical health data to improve knowledge-sharing and health-care outcomes. Also includes statistics related to the benefits of, and opportunities for, exchanging health information
What is health information exchange?
It is a way for healthcare professionals to share healthcare information about a patient across different healthcare organizations. This is done electronically through different information systems. A great example to better understand this is the doctor electronically sending a prescription to the pharmacy. Of course, this isn’t the only way health information is exchanged through systems, but it is the best way to visualize and understand it.
Is there an exchange for health information in New Jersey?
In New Jersey, there is a statewide health information exchange network that was launched relatively recently, as well as smaller health information exchange networks. The New Jersey Health Information Network is also looking to eventually exchange health information nationally with eHealth exchange. The current focuses include a statewide admission transfer notification service that could improve post-discharge outcomes, a common key service which provides a consistent and reliable way to match patients across multiple organizations, a health provider directory service, and a state health data hub. Another really interesting project is one that could help providers reduce the problems associated with opioid over-prescribing.
What is HIE in health care?
An HIE is an organization that oversees the collection and secure exchange of health information. This coordination and sharing of information is crucial to the health of a patient.
How many HIEs are there in Michigan?
The Michigan Health Information Network Shared Services (MiHIN) is the network for Michigan. You can learn more about MiHIN here. There are thirteen HIEs currently in the state of Michigan.
What is HIE exchange?
To understand what makes up a Health Information Exchange (HIE), a person must first understand what is considered health information. Health Information is any medical information created or received by a health professional (your doctor or pharmacist, for example) and relates to the past, present, or future physical or mental health of a patient.
What is EHR in China?
There is a somewhat unique feature of Electronic Health Records (EHR) in China, with somewhat different definitions from commonly adopted definitions. For hospitals of level 2 or 3, electronic medical records system (EMRs) are routinely adopted to manage all pertinent medical information, internal clinical information exchanges, patient care and services. In contrast, the level 1 hospitals (and also those primary health clinics throughout countryside or local communities) have adopted Electronic Health Record systems (EHRs), which are constructed for managing and sharing basic medical and health information among hospitals in the region and, most importantly, for public health information management. While the EMRs and EHRs share some medical-related contents, they have been optimized for fairly different objectives and hence include many components that are fairly different. Currently, most of these two systems are independent of each other, and are not inter-connected. Through recent promotion and organization of the National Health Commission of China (formerly the Ministry of Health), EMRs in level 2 and 3 hospitals have been generally adopted, and are well developed for hospital operation, management, patient-care, and patient services inside the hospitals. Indeed, the development of health information technology is an important criterion for hospital evaluation and for designation of hospital competencies. In contrast, EHR systems in level 1 hospitals or other health clinics have not been developed aswell, despite major effort by governmental promotions and supports. There remain substantial gaps and challenges for health data exchanges between regions, even though some within-region exchange systems are reasonably developed. Additionally, even for those well-developed regions, information sharing between EMR and EHR is still lacking. A primary contributing factor for this lack is that EMRs and EHRs are generally developed by different groups of companies in different years. Because of different requirements and purposes for developing EMR and EHR systems, these companies have adopted different information standards, infrastructures, and data formats for their respective objectives. Consequently, these two systems are not easily integrated, and the differences present a major challenge for health information and data sharing across hospital-oriented and public health-oriented systems for a foreseeable future.
How is the NHS funded?
The English National Health Service (NHS) was created in 1948 to provide health care free at the point of delivery. The NHS is funded through general taxation. Funds are distributed by parliamentary vote through regional and local organizations for health care. Recently a key organizational change has brought Clinical Commissioning Groups (CCGs) together into Sustainability and Transformation Partnerships (STPs), which usually combine 5 CCGs covering populations of 1-2 million. This has had consequences for health IT expenditure. In 2003, the UK government created the National Programme for IT (NPfIT). The aim of this nationwide initiative was to fully computerize the NHS over 10 years. While the NPfIT did not achieve all of its goals, it did develop a national framework for connectivity and standards implementation, and these have now been adopted by the STPs who have now taken charge of local health IT development and the implementation of a new health information exchange initiative named the Local Health Care Record Exemplar programme (LHCRE). The underlying concepts behind the LHCRE are patient use and ownership of health data, data exchange across traditional boundaries of health economies and service transformation driven by data and system interoperability using clinical and technology standards. For example, the One London LHCRE is designed to provide HIE and service transformation for the whole of London by extending local HIE services, application of interoperability standards for data and image exchange and includes social care organizations.
How are authors selected for health informatics?
Authors were selected for their involvement and connections in health informatics from an academic, policy or professional standpoint, or through a combination of these connections. The scenarios used to scaffold this exercise were initially developed for an international HIE workshop delivered by the authors at the Medinfo 2013 conference in Copenhagen, Denmark. The country status reports have been reviewed and updated periodically since that time by the authors and their contacts, most recently in April 2019 during the development of this manuscript, which also benefits from peer-review. To the best of our knowledge, they provide an up-to-date summary of current practices, mindful of the caveats noted in the discussion.
Why is health information exchange important?
Health information exchange (HIE) is frequently cited as an important objective of health information technology investment because of its potential to improve quality, reduce cost, and increase patient satisfaction. In this paper we examine the status and practices of HIE in six countries, drawn from a range of higher and lower income regions.
What is access to digital services resident on the private NHS network formerly known as?
Access to digital services resident on the private NHS network formerly known as N3.
What is NHS Spine?
NHS Spine – a set of services, applications and directories. The Spine now supports over one billion monthly transactions.
Why are hospitals public?
Most hospitals are public and are overloaded in meeting the country’s health care needs. The primary incentives for hospital leaders who are taking on the development of health IT are reputational gains and recognition for being progressive in adopting information technologies and actively engaging in the health care reform.
History
- Historically most Americans medical information was stored on paper in filing cabinets at various medical offices, or in boxes and folders in patients homes. There has been a tremendous push over the past several years to digitize the health care experience and to allow for increased accessibility and portability of health information.
Advantages
- Appropriate and timely sharing of vital patient information better informs decision-making at the point of care and allows clinicians to:
Introduction
- Standardizing data is an important factor in electronically exchanging health information. Once standardized, the transferred data can be integrated into the recipients' electronic health record (EHR), further improving patient care. There are currently 3 key forms of health information exchange:
Purpose
- The Trusted Exchange Framework and the Common Agreement will outline a policy and technical approach for nationwide electronic health information exchange. TEFCA is mandated as part of the 21st Century Cures Act. Once finalized, it will allow clinicians and other health care providers to access patient health data from a variety of health information networks (HINs).
Benefits
- Health care practices will only have to connect to 1 HIN in order to access patient information from HINs across the country. Being able to access this information can ensure patient safety and better care quality especially when providing unplanned care.
Qualification
- To participate in health information exchange through the TEF and the Common Agreement, health care providers can: