The trigone is a triangular muscular structure located between the bladder and urethra. Effective connection between the ureters and the trigone are vital for proper functioning of the ureteral valve mechanism.
What are the anatomic boundaries of the trigone of the bladder?
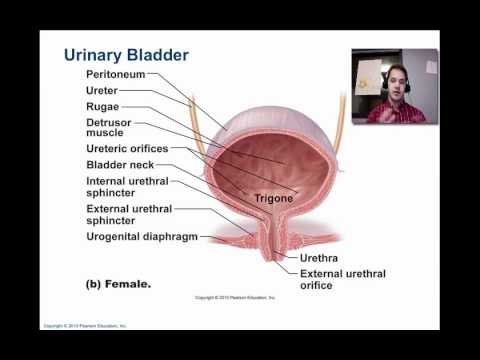
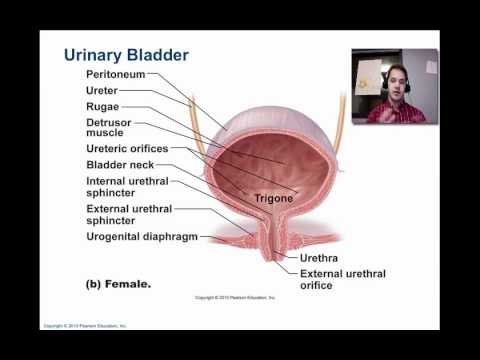
The trigone is a triangular area on the internal face of the posterior wall of the bladder. The posterior vertices are the ureteric orifices and the anterior vertex is the neck of the bladder. It sends urine into the urethra when the bladder contracts.
What are signs of bladder problems?
- Being unable to urinate
- Lower back pain on one side
- Loss of appetite and weight loss
- Feeling tired or weak
- Swelling in the feet
- Bone pain
What diseases are in the bladder?
Types of bladder cancer include:
- Urothelial carcinoma. Urothelial carcinoma, previously called transitional cell carcinoma, occurs in the cells that line the inside of the bladder. ...
- Squamous cell carcinoma. Squamous cell carcinoma is associated with chronic irritation of the bladder — for instance, from an infection or from long-term use of a urinary catheter. ...
- Adenocarcinoma. ...
Why am I leaking urine all of a sudden?
Total incontinence can be caused by:
- a problem with your bladder from birth
- injury to your spinal cord – this can disrupt the nerve signals between your brain and your bladder
- a bladder fistula – a small, tunnel like hole that can form between the bladder and a nearby area, such as the vagina

What is the function of the trigone in the bladder?
The trigone is the site of the anti-reflux mechanism. (A). Schematic of the trigone at the bladder base and its connections with the ureters showing the intramural ureter segment that is normally compressed to prevent back-flow of urine to the ureters and kidneys.
Where is the trigone of the bladder located?
Trigone. The trigone is a triangular portion of the bladder floor bordered (ventrally) by the internal urethral opening or bladder neck and (dorsolaterally) by the orifices of the right ureter and left ureter.
Why is the trigone clinically important?
Why is the trigone of the urinary bladder clinically important? Infections tend to persist in the trigone. Urine moves down the ureters into the bladder due to gravitational pull alone. Urine may routinely contain sodium, potassium, proteins, and red blood cells.
What is a trigone?
tri·gone ˈtrī-ˌgōn. variants also trigon. -ˌgän. : a triangular body part. specifically : a smooth triangular area on the inner surface of the bladder limited by the apertures of the ureters and urethra.
Can trigonitis go away on its own?
Trigonitis may pass on its own. Others may need treatment to ease symptoms. Medicine may help to: Ease bladder spasms or pain.
Is trigonitis an infection?
Trigonitis, although its name suggests inflammation, is a metaplastic process. The precise underlying cause is not known, but squamous metaplasia in the bladder usually occurs in response to irritation (eg, from a long-term indwelling catheter) or infection.
What 3 structures are connected by the trigone?
Urinary Bladder, Ureter, and Urethra The urothelium of the trigone and the musculature and other connective tissue components of the bladder and urethral walls are of mesodermal origin. The ureters are derived entirely from mesoderm.
How long does trigonitis last?
Resolution of trigonitis at 6 months was noted in 25 (76%) patients.
What three structures are connected by the trigone?
The three structures that outline the triangular region of the bladder known as the trigone are the two openings of the ureters (on the left and right side) as well as the inner urethral orifice.
Do men have trigone?
Ureter and the superficial bladder trigone: The superficial trigone extends into the prostatic urethra to the seminal colliculus in men and to the external urethral orifice in women.
What type of problem most commonly affects the urinary system organs?
The most common urinary issues are bladder infections and urinary tract infections (UTIs). UTIs are more common in women than in men. More than 60% of women will get a UTI in their lifetime.
How did the trigone get its name?
The name trigone comes from the Latin word trigonum, meaning triangle. It is commonly used as a descriptor for parts of human anatomy that have a triangular shape, but is most commonly used for part of the urinary tract. It is also used to describe the space where three or four more plant cells meet.
What 3 structures are connected by the trigone?
Urinary Bladder, Ureter, and Urethra The urothelium of the trigone and the musculature and other connective tissue components of the bladder and urethral walls are of mesodermal origin. The ureters are derived entirely from mesoderm.
What three structures are connected by the trigone?
The three structures that outline the triangular region of the bladder known as the trigone are the two openings of the ureters (on the left and right side) as well as the inner urethral orifice.
Do men have trigone?
Ureter and the superficial bladder trigone: The superficial trigone extends into the prostatic urethra to the seminal colliculus in men and to the external urethral orifice in women.
What openings form the trigone quizlet?
The trigone is the triangular area made up of the openings from the ureters and the opening into the urethra. The urethra is the tube from the bladder to the outside of the body. Urethra, duct that transmits urine from the bladder to the exterior of the body during urination.
How do ureters work?
This intramural segment of the ureter functions as a one-way valve to prevent vesicoureteral reflux with progressive bladder distention. 1 Ureters are muscular tubes, similar to the esophagus. As a “bolus” of urine accumulates in the renal pelvis, pacemaker activity induces a muscular contraction that propagates the bolus of urine down the ureter to the bladder. With changes in urine flow in other species, the length of the “urine bolus” changes while the rate of transport down the ureter remains the same. 3 Passage of “urine boluses” can be appreciated in horses during either cystoscopy or transrectal ultrasonographic examination. During cystoscopy, streams of urine can be seen to intermittently exit each ureter. These urine streams are asynchronous and vary in volume and frequency with changes in urine flow. 5 During transrectal ultrasonography, forceful passage of urine from the ureters into the bladder can be appreciated by swirling of the echogenic urine in the bladder near the trigone.
Where are the receptors located in the lower urinary tract?
Lower Urinary Tract Pharmacology: Receptors and Neurotransmitters (eSlide 20.1)#N#Cholinergic muscarinic (M 2 and M 3) receptors are distributed in the body of the bladder, trigone, bladder neck, and urethra. The M 2 cholinergic muscarinic receptors structurally predominate in normal bladders, but the M 3 receptors may be functionally more important for bladder contraction. Cholinergic nicotinic receptors are primarily located in the striated sphincter. Adrenergic receptors (predominantly α 1) are concentrated in the trigone, bladder neck, and urethra. Norepinephrine-containing nerve cells are distributed in the paravesical and intramural ganglia, which maintain continence by producing contraction of the bladder neck and urethral smooth muscle. β 2 -Adrenergic and β 3 -adrenergic receptors produce relaxation at the bladder neck on initiation of voiding and relax the bladder body to enhance storage. The main effector transmitter for urethra contraction is norepinephrine (via the α 1 receptors), and the relaxation of the urethra is caused by the release of nitric oxide in the urethral wall, which is mediated by acetylcholine in the pelvic ganglia.
Where does the ureter open?
The ureter traverses beneath mucosa and opens in a distal location.
Does estrogen help with urinary incontinence?
Topical estrogen may be effective in helping to treat some urinary incontinence symptoms , especially urgency, by reversing vaginal mucosal atrophy and augmenting local support tissues. However, evidence regarding estrogen therapy is mixed, with some studies showing higher rates of incontinence in those taking oral estrogen. An α‐adrenergic agonist like pseudoephedrine can be used to treat mild SUI by increasing internal sphincter tone and bladder outflow resistance. A new serotonin and norepinephrine dual‐reuptake inhibitor (duloxetine) has been found to be efficacious and safe for use in women with SUI and has also demonstrated efficacy in the treatment of major depressive disorder. Mechanical devices including vaginal inserts like a pessary, periurethral injections (bulking agents), and urethral blockers such as a supersized vaginal tampon can also all be considered for SUI.
What is the trigone?
The interior of bladder. The trigone (a.k.a. vesical trigone) is a smooth triangular region of the internal urinary bladder formed by the two ureteric orifices and the internal urethral orifice .
Where does the trigone come from?
The signals become stronger as the bladder continues to fill. Embryologically, the trigone of the bladder is derived from the caudal end of mesonephric ducts, which is of mesodermal origin (the rest of the bladder is endodermal ).
Where is the trigone located?
The trigone is the neck of the bladder. It’s a triangular piece of tissue located in the lower part of your bladder. It’s near the opening of your urethra, the duct that carries urine from your bladder outside of your body. When this area becomes inflamed, it’s known as trigonitis. However, trigonitis isn’t always the result of inflammation.
What is it called when the trigone is inflamed?
When this area becomes inflamed, it’s known as trigonitis. However, trigonitis isn’t always the result of inflammation. Sometimes it’s due to benign cellular changes in the trigone. Medically, these changes are called nonkeratinizing squamous metaplasia. This results in a condition called pseudomembranous trigonitis.
How many people have trigonitis?
The majority of people with trigonitis are women of childbearing age as well as men undergoing hormone therapy for things like prostate cancer. According to research, pseudomembranous trigonitis occurs in 40 percent of adult women — but fewer than 5 percent of men.
What to do if you think you have trigonitis?
If you think you have trigonitis or any other bladder issues, see your doctor or urologist to discuss your symptoms, get a thorough examination, and receive the appropriate treatment. Last medically reviewed on June 28, 2018.
What are the symptoms of trigonitis?
They include: an urgent need to urinate. pelvic pain or pressure. difficulty urinating. pain during urination. blood in the urine.
Where is trigonitis seen?
While they share some of the same symptoms, trigonitis differs from IC in several ways: The inflammation that occurs with trigonitis is only seen in the trigone region of the bladder. IC can cause inflammation throughout the bladder.
What is the pain in the bladder called?
Interstitial cystitis (IC) — also called painful bladder syndrome — is a chronic condition that produces intense pain and inflammation in and above the bladder.
Where is the bladder located?
Generally, the bladder is a hollow, muscular, and pear-shaped distensible elastic organ that sits on the pelvic floor. It receives urine via the ureters, which are thick tubes running from each kidney down to the superior part of the bladder.
What is the base of the bladder?
The fundus is the base of the bladder, which is formed by the posterior wall and contains the trigone of the bladder, and is lymphatically drained by the external iliac lymph nodes. The trigone is the structure that contains the outlet (urethra) of the bladder.
What is the detrusor muscle?
The detrusor muscle is a layer of the bladder wall made of smooth muscle fibers that are arranged in spiral, longitudinal, and circular bundles. This signal will encourage the bladder to expel urine through the urethra. Sensations from the bladder are transmitted to the central nervous system (CNS) via general visceral afferent fibers (GVA). Whereas GVA fibers on the superior surface of the bladder follow the course of the sympathetic effect nerves back to the CNS, GVA fibers on the inferior portion follow along with the parasympathetic efferent fibers. Surprisingly (or maybe not), a meta-analysis conducted on the effects of different voiding positions in male urodynamics reports that sitting down allows for improved contraction of the detrusor muscle.
Why do babies have incontinence?
Problems with the muscles of the urinary bladder or sphincters can lead to incontinence (involuntary urination). In babies, the nervous system has not yet developed further, so a baby's bladder fills to a set point, then automatically contracts and empties. As the child matures, so does the nervous system, which means the brain can now receive messages from the filling bladder and prevent it from automatically emptying until convenient. Failures in this control mechanism results in incontinence, but there are many different ways that lead to mechanism failure (e.g. neurologic injury, congenital defects, strokes, multiple sclerosis, and aging).
Which organ collects urine?
The urinary bladder is an organ that serves to collect urine to be voided through urination after the urine is filtered through the kidneys (where the necessary ions are reabsorbed if physiologically needed through feedback mechanisms found throughout the body and in the nephrons of the kidneys, such as the macula densa).
Where do GVA fibers follow?
Whereas GVA fibers on the superior surface of the bladder follow the course of the sympathetic effect nerves back to the CNS, GVA fibers on the inferior portion follow along with the parasympathetic efferent fibers.
Does the urinary bladder produce mucus?
Histologically, the urinary bladder is lined with transitional epithelium and does not produce mucus. This article will describe the anatomy of the urinary bladder. Key facts about the urinary bladder. Parts. Body, which collects the urine. Fundus (base), which contains the trigone. Trigone, which houses the urethra.