
What is transcortical motor aphasia (TMA)?
Transcortical Motor Aphasia (TMA or TMoA) is a type of aphasia that is similar to Broca’s aphasia. TMA is due to stroke or brain injury that impacts, but does not directly affect, Broca’s area. Broca’s area is the area of the brain responsible for language production.
How is transcortical aphasia treated?
How Aphasia Is Treated Treatment for transcortical aphasia is similar to other types of aphasia. One of the most effective ways to treat sensory and motor aphasia is through speech therapy. Speech therapy exercises work by activating neuroplasticity, the brain’s natural repair mechanism.
What is the difference between Broca’s aphasia and transcortical motor aphasia?
Transcortical Motor Aphasia. The principal difference between transcortical motor aphasia and Broca’s aphasia is in verbal repetition, which is possible in the former and impaired in the latter. Patients with transcortical motor aphasia often have echolalia in the setting of an otherwise nonfluent speech.
What are the causes of mixed transcortical aphasia?
The most common cause of mixed transcortical aphasia is a watershed stroke of the language association areas as a result of severe internal carotid stenosis. 5 Aphasia is one of the most difficult disabilities to live with after a stroke.
What are the symptoms of Transcortical sensory aphasia?
One type of aphasia, called transcortical sensory aphasia, can cause poor auditory comprehension. It most commonly occurs after damage to the temporal lobe....Transcortical Sensory Aphasia SymptomsReading difficulties.Naming problems.Paraphasia (error-prone speech)Echolalia (compulsively repeating what others say)
What type of aphasia is Transcortical sensory aphasia?
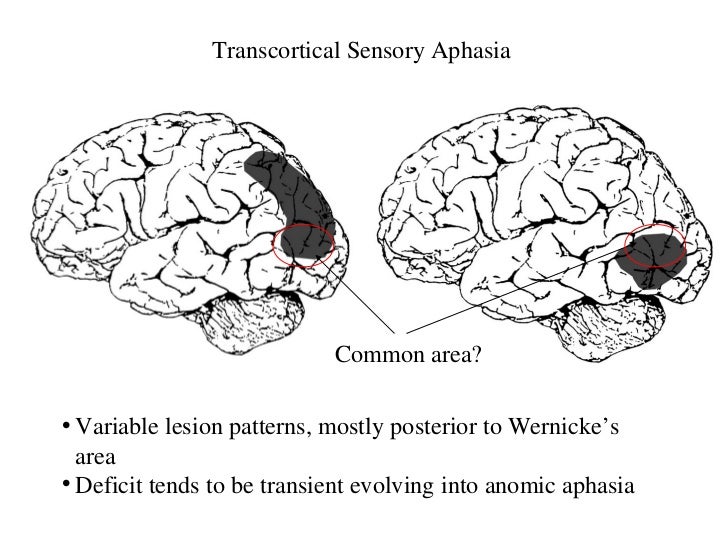
Transcortical sensory aphasia (TSA) is a kind of aphasia that involves damage to specific areas of the temporal lobe of the brain, resulting in symptoms such as poor auditory comprehension, relatively intact repetition, and fluent speech with semantic paraphasias present.
How do you test for Transcortical aphasia?
Diagnosing Transcortical Aphasia Screening can include evaluation of oral motor functions, speech production skills, comprehension, use of written and verbal language, cognitive-communication, swallowing, and hearing.
What part of the brain is affected by Transcortical motor aphasia?
anterior left frontal lobeThe lesions that lead to transcortical motor aphasia are typically found on the mesial surface of the anterior left frontal lobe, near supplementary motor cortex, or along the lateral aspect of the left frontal lobe; in either case these lesions fall outside of what is traditionally thought of as Broca's area.
What is the difference between motor and sensory aphasia?
Motor aphasia had high levels of 'quiet', 'passive' 'dumb', 'unstable' and 'gloomy' images, while sensory aphasia had high levels of 'noisy', 'unstable', 'cheerful', 'sensitive', 'fluctuating in emotions', 'active', 'dumb' and 'gloomy' images.
How do you get Transcortical motor aphasia?
TMA is due to stroke or brain injury that impacts, but does not directly affect, Broca's area. Broca's area is the area of the brain responsible for language production. TMA is the result of a stroke or brain injury that is near Broca's area.
What is the most severe type of aphasia?
Global aphasia is the most severe type of aphasia. It is caused by injuries to multiple parts of the brain that are responsible for processing language. Patients with global aphasia can only produce a few recognizable words. They can understand very little or no spoken language.
Can you fully recover from aphasia?
Some people with aphasia recover completely without treatment. But for most people, some amount of aphasia typically remains. Treatments such as speech therapy can often help recover some speech and language functions over time, but many people continue to have problems communicating.
What are the 4 types of aphasia?
The most common types of aphasia are: Broca's aphasia. Wernicke's aphasia. Anomic aphasia....Primary progressive aphasia (PPA)Read.Write.Speak.Understand what other people are saying.
What is the difference between Wernicke's aphasia and Transcortical sensory aphasia?
TSA is similar to Wernicke's aphasia because TSA is due to damage in the brain that occurs close to Wernicke's area. Wernicke's area is the part of the brain that is responsible for language comprehension. However, in TSA there is no damage to Wernicke's area itself.
What are the 3 types of aphasia?
The three most common types of aphasia are: Broca's aphasia. Wernicke' s aphasia. Global aphasia1.
What kind of aphasia does Willis have?
Expressive aphasia (also called Broca's aphasia) involves difficulty in conveying thoughts through speech or writing. The person knows what they want to say but cannot find the words needed.
What is transcortical aphasia?
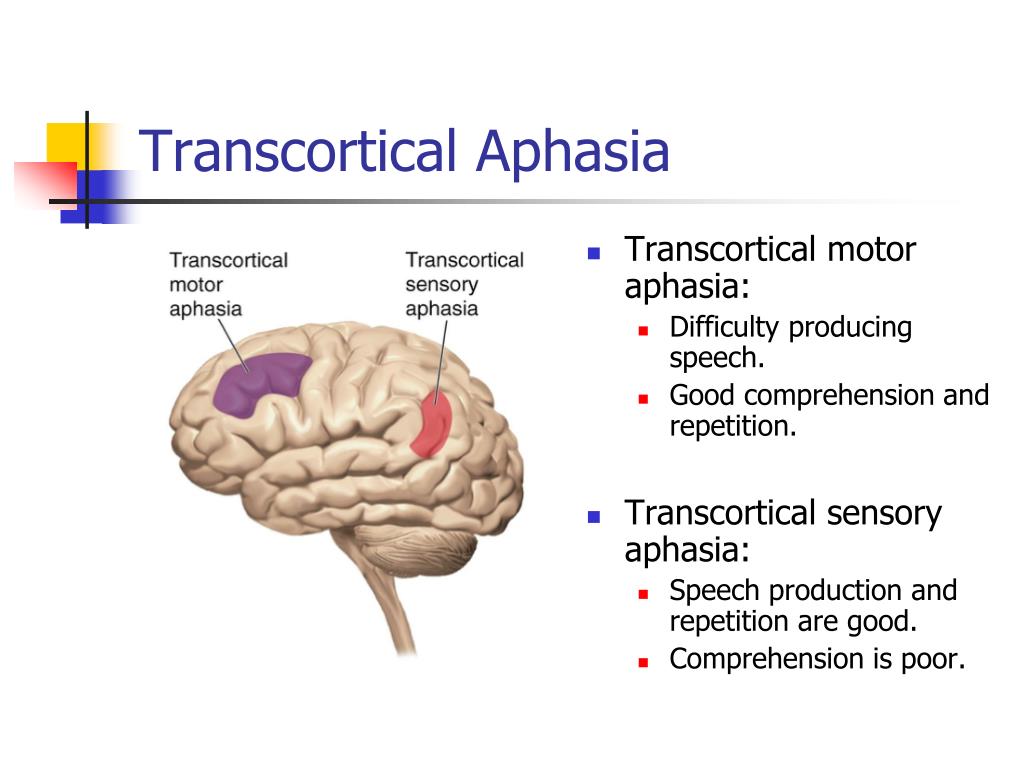
The transcortical aphasias are a group of aphasia syndromes that all have in common a relatively preserved ability to repeat, despite other significant language deficits. Transcortical motor aphasia is similar to Broca’s aphasia; that is, patients exhibit nonfluent speech and relatively good comprehension, but the ability to repeat is relatively preserved. Transcortical sensory aphasia is similar to Wernicke’s aphasia, with patients exhibiting fluent speech and poor comprehension and also a relatively preserved ability to repeat. Finally, mixed transcortical aphasia is similar to global aphasia but with relatively preserved repetition. Compared to the other aphasias, the transcortical aphasias are relatively rare.
Where is transcortical motor aphasia found?
The lesions that lead to transcortical motor aphasia are typically found on the mesial surface of the anterior left frontal lobe, near supplementary motor cortex, or along the lateral aspect of the left frontal lobe; in either case these lesions fall outside of what is traditionally thought of as Broca's area.
What is the difference between Broca's aphasia and transcortical motor apha?
Transcortical Motor Aphasia. The principal difference between transcortical motor aphasia and Broca’s aphasia is in verbal repetition , which is possible in the former and impaired in the latter. Patients with transcortical motor aphasia often have echolalia in the setting of an otherwise nonfluent speech.
What is the term for a lesion that separates the processing of speech from the mechanisms for initiating the action?
Transcortical motor aphasia , another form of the transcortical aphasias, is sometimes known as dynamic aphasia or anterior isolation syndrome. Functionally, the causal lesion separates the processing of speech from the mechanisms for initiating the action to speak.
What is TCMA in medical terms?
Transcortical motor aphasia (TCMA) involves lesions of the left frontal lobe–supplementary motor area (SMA), just anterior and superior to Broca's area. During acute phases, patients may initially present as mute but later develop a clinical profile characterized by normal repetition and comprehension, with limited, slow, and perseverative spontaneous speech.
How can an occupational therapist help with transcortical motor aphasia?
Since the individual is dependent on the listener to initiate, maintain, and repair conversation breakdowns, 56 the occupational therapist can facilitate communication with a patient who has transcortical motor aphasia by providing cues for communication. In addition, the patient will need prompting to use his or her calendar, notebook, and other augmentative systems (see Table 29-3 ).
What are the cognitive limitations of transcortical motor aphasia?
When working with a patient with transcortical motor aphasia, cognitive limitations are subtle and may impede the therapeutic process. Because the cognitive changes are not obvious, the staff may overestimate the patient's ability to perform and become frustrated by the patient's difficulty appreciating the rationale between the goal and the assigned therapeutic activities. The failure to initiate is not limited to speech but also includes ADL. Moreover, the patient's flat affect and lack of engagement with others are notable features of the patient's communication problem.
What is transcortical motor aphasia?
However, transcortical motor aphasia occurs when a stroke or brain injury damages the nerve fibers that send information back and forth between these two areas. As a result, Broca’s and Wernicke’s area are essentially isolated from each other.
What is the defining feature of transcortical motor aphasia?
The defining feature of transcortical motor aphasia is halting, laborious speech. The person might make multiple starts and stops. This makes motor aphasia similar to expressive aphasia.
How to treat transcortical aphasia?
One of the most effective ways to treat sensory and motor aphasia is through speech therapy. Speech therapy exercises work by activating neuroplasticity, the brain’s natural repair mechanism.
What is the condition that makes it difficult to speak?
Transcortical motor aphasia is a rare category of aphasia that can make it difficult to speak or understand others. The symptoms can very greatly between patients, which makes it critical to work alongside a speech therapist.
What is the diagnosis of transcortical aphasia?
Diagnosing Transcortical Aphasia. Diagnosis for transcortical motor aphasia is typically performed by a speech-language pathologist. While there no specific tests for motor aphasia exist, therapists can use different screening and assessment protocols to identify the type of aphasia you have.
Why is pace therapy appropriate for people with aphasia?
Because PACE therapy can be adapted to different skill levels, it is appropriate for people with many types and severities of aphasia, including transcortical motor aphasia.
How to treat motor aphasia?
One of the most effective ways to treat sensory and motor aphasia is through speech therapy . Speech therapy exercises work by activating neuroplasticity, the brain’s natural repair mechanism. Neuroplasticity refers to the brain’s ability to form new neural pathways in response to repetition.
What is transcortical motor aphasia?
Transcortical motor aphasia ( TMoA ), also known as commissural dysphasia or white matter dysphasia, results from damage in the anterior superior frontal lobe of the language-dominant hemisphere. This damage is typically due to cerebrovascular accident (CVA). TMoA is generally characterized by reduced speech output, which is a result of dysfunction of the affected region of the brain. The left hemisphere is usually responsible for performing language functions, although left-handed individuals have been shown to perform language functions using either their left or right hemisphere depending on the individual. The anterior frontal lobes of the language-dominant hemisphere are essential for initiating and maintaining speech. Because of this, individuals with TMoA often present with difficulty in speech maintenance and initiation.
What is a dynamic aphasia?
For instance, adynamic aphasia is a form of TMoA that is characterized by sparse speech. This occurs as a result of executive functioning in the frontal lobe. Another form of aphasia related to TMoA is dynamic aphasia.
Why do people with TMOA have a low speech output?
Due to damage in the anterior superior frontal lobe, people with TMoA have deficits in initiation and maintenance of conversations, which results in reduced speech output. A person with TMoA may seldomly produce utterances and typically remain silent.
How is TMoA diagnosed?
TMoA, or any other type of aphasia, is identified and diagnosed through the screening and assessment process. Screening can be conducted by a SLP or other professional when there is a suspected aphasia. The screening does not diagnose aphasia, rather it points to the need for a further comprehensive assessment. A screening typically includes evaluation of oral motor functions, speech production skills, comprehension, use of written and verbal language, cognitive communication, swallowing, and hearing. Both the screening and assessment must be sensitive to the patient's linguistic and cultural differences. An individual will be recommended to receive a comprehensive assessment if their screening shows signs of aphasia. Under the American Speech-Language-Hearing Association (ASHA) and World Health Organization (WHO) guidelines and the International Classification of Functioning, Disability and Health (ICF) framework, the comprehensive assessment encompasses not only speech and language, but also impairments in body structure and function, co-morbid deficits, limitations in activity and participation, and contextual (environmental and personal) factors. The assessment can be static (current functioning) or dynamic (ongoing) and the assessment tools can be standardized or nonstandardized. Typically, the assessment for aphasia includes a gathering of a case history, a self-report from the patient, an oral-motor examination, assessment of expressive and receptive language in spoken and written forms, and identification of facilitators and barriers to patient success. From this assessment, the SLP will determine type of aphasia and the patient's communicative strengths and weaknesses and how their diagnosis may impact their overall quality of life.
What is the assessment of aphasia?
Typically, the assessment for aphasia includes a gathering of a case history, a self-report from the patient, an oral-motor examination, assessment of expressive and receptive language in spoken and written forms, and identification of facilitators and barriers to patient success.
Does aphasia affect intensity?
Research has shown that treatment has a direct effect on aphasia outcomes. Intensity, duration and timing of treatment all need to be taken in to consideration when choosing a course of treatment and determining a prognosis. In general, greater intensity leads to greater improvement.
Which lobe is responsible for the initiation and ideation of verbal speech?
The anterior superior frontal lobe is known as the prefrontal cortex which is responsible for the initiation and ideation of verbal speech. The damage leaves the major language networks, Broca's and Wernicke’s areas and the arcuate fasiculus, unaffected.
What are the different types of transcortical aphasia?
There are three main types of transcortical aphasia: Transcortical motor aphasia. Transcortical sensory aphasia. Mixed transcortical aphasia.
What is aphasia in psychology?
Aphasia is a language deficit that occurs as a result of damage to one or more of the speech areas in the brain. There is more than one speech area in the brain, and the exact location of damage from a stroke determines the pattern of speech loss.
What is a form of hesitant speech called?
Mild transcortical motor aphasia can produce a form of hesitant speech known as telegraphic speech. Transcortical motor aphasia is typically caused by a stroke located nearby Broca’s area, just to the front of it.
What is the most common form of aphasia?
Transcortical aphasia is one of the less common types of aphasia. The more common and well-known forms of aphasia, Broca's aphasia, and Wernicke's aphasia, result from injuries to areas involved in the production of speech (Broca’s aphasia) or the comprehension of speech (Wernicke’s aphasia).
How to help a stroke survivor with aphasia?
Living with aphasia requires patience, as does caring for a stroke survivor who has aphasia. There are several approaches to speech therapy which can help improve speech and communication to help optimize daily life after a stroke. Be sure to convey your concerns about your speech problems to your medical team so that you can be directed to the best rehabilitation available to you, which may help in improving your overall quality of life as you recover from your stroke.
Where is the speech area located?
Speech areas of the brain are located in the dominant hemisphere, which is half of the brain opposite your dominant hand. Transcortical aphasia is one of the less common types of aphasia.
What are the areas of the brain that are affected by language deficits?
Other, less common language deficits can also result when there are injuries to the nerve fibers that carry information between the Wernicke's or the Broca's area , or between these areas and other areas of the brain that process the subtle aspects of language, such as emotion, vocal tone, thinking and facial expressions. 1
Transcortical Motor Aphasia Symptoms
Transcortical motor aphasia is a speech disorder in which patient cant speak properly. He cannot even start a conversation and further maintain it. Executive functions of language are affected which mainly involve Grammer (Syntex) control, patient can't narrate a story or any thing he wants to and language response center is not properly activated.
Transcortical Motor Aphasia Causes
Transcortical motor aphasia occurs due to damage in the frontal lobe of brain. Frontal lobe specifically left hemisphere contains language control center. Usually damage in anterior superior frontal lobe is responsible for transcortical motor aphasia. This damage occurs due to cerebrovascular problem I.e. infarction.
Transcortical Motor Aphasia Treatment
Treatment of transcortical motor aphasia involves speech therapy. Its treatment mainly focus on patients strong hearing conversation and skills of repetition and correcting the reduced speech output of patient. Treatment also covers maintenance of speech and initiation of speech including language.
What is the cause of transcortical motor aphasia?
Transcortical motor aphasia is usually due to Ischemia In the left middle cerebral artery or nearby areas that may involve the anterior cerebral artery. Usually appears due to a stroke in the Frontal lobe Superior of the dominant hemisphere for language (usually the left).
Who studied a case of aphasia, examining the postmortem brain?
Norman Geschwind studied a case of this type of aphasia, examining the postmortem brain.
How many cases of aphasia are there?
According to the Copenhagen Aphasia Study, of 270 cases of aphasia, only 25 patients (9%) had transcortical aphasia. Specifically, 2% was motor type. On the other hand, transcortical motor aphasia is more frequent (8%) than sensory (3%) when it has been longer after the injury (during the first month after damage).
What does it mean that the damage left incommunicado the areas of the language of the rest of the cortex?
So that the damage left incommunicado the areas of the language of the rest of the cortex and conserved more areas of Wernicke and of Broca , in addition to the connections between them. This means that the areas of language and production understanding are preserved, but not enough.
Why is it characterized by the absence of the initiative to speak?
It is characterized by the absence of the initiative to speak, because there is a deficit in strategies in the lexical and semantic search or not know how to choose between several verbal responses. On the other hand, understanding, naming and repetition are intact.
Which area of the brain is associated with the auditory aspect of words and understanding of language?
And it would be associated with both Wernicke area (Focusing on the auditory aspect of words and understanding of language) and with the Broca area (Centered on the motor aspect of words and expression of speech).
Is aphasia common in Broca?
As we said, it is common for patients with Broca or global aphasia to evolve to this type of aphasia.
Overview
Transcortical motor aphasia (TMoA), also known as commissural dysphasia or white matter dysphasia, results from damage in the anterior superior frontal lobe of the language-dominant hemisphere. This damage is typically due to cerebrovascular accident (CVA). TMoA is generally characterized by reduced speech output, which is a result of dysfunction of the affected region of the brain. The left hemisphere is usually responsible for performing language functions, althoug…
Symptoms and signs
TMoA is classified as a non-fluent aphasia that is characterized by a significantly reduced output of speech, but good auditory comprehension. Auditory comprehension skills remain intact because the arcuate fasciculus and Wernicke's area are not impaired. Individuals with TMoA also exhibit good repetition skills and can repeat long, complex phrases effortlessly and without error. However, spontaneous speech often presents with paraphasias (a wide category of speech error…
Causes
Neurological imaging has shown that TMoA is typically caused by an infarct of the anterior superior frontal lobe in the perisylvian area of the left, or language-dominant, hemisphere. The anterior superior frontal lobe is known as the prefrontal cortex which is responsible for the initiation and ideation of verbal speech. The damage leaves the major language networks, Broca's and Wernicke’s areas and the arcuate fasiculus, unaffected. Brain injury can result from a stroke c…
Diagnosis
TMoA is diagnosed by the referring physician and speech-language pathologist (SLP). The overall sign of TMoA is nonfluent, reduced, fragmentary echoic, and perseverative speech with frequent hesitations and pauses. Patients with TMoA also have difficulty initiating and maintaining speech. However, speech articulation and auditory comprehension remain typical. The hallmark sign of TMoA is intact repetition in the presence of these signs and symptoms.
Treatment
Treatment for all types of aphasia, including transcortical motor aphasia, is usually provided by a speech-language pathologist. The SLP chooses specific therapy tasks and goals based on the speech and language abilities and needs of the individual. In general for individuals with TMoA, treatment should capitalize on their strong auditory comprehension and repetition skills and address the individual's reduced speech output and difficulty initiating and maintaining a conver…
Prognosis
In relation to other types of aphasia, TMoA occurs less frequently, so there is less information on its prognosis. In general, for individuals with aphasia, most recovery is seen within 6 months of the stroke or injury although more recovery may continue in the following months or years. The timeline of recovery may look different depending on the type of stroke that caused the aphasia. With an ischemic stroke, recovery is greatest within the first two weeks and then diminishes ove…
See also
• Transcortical sensory aphasia
Causes
Classification
- Transcortical aphasia is one of the less common types of aphasia. The more common and well-known forms of aphasia, Broca's aphasia, and Wernicke's aphasia, result from injuries to areas involved in the production of speech (Brocas aphasia) or the comprehension of speech (Wernickes aphasia).
Language
- Other, less common language deficits can also result when there are injuries to the nerve fibers that carry information between the Wernicke's or the Broca's area, or between these areas and other areas of the brain that process the subtle aspects of language, such as emotion, vocal tone, thinking and facial expressions.
Types
- Transcortical aphasias include types of aphasias that are produced by injuries to or from the many connections that integrate the language areas in the brain. There are three main types of transcortical aphasia:
Symptoms
- Mild transcortical motor aphasia can produce a form of hesitant speech known as telegraphic speech. Transcortical motor aphasia is typically caused by a stroke located nearby Brocas area, just to the front of it. Stroke survivors with this rare type of aphasia cannot comprehend what others say but can speak fluently. Someone with transcortical sens...
Example
- For instance, if your loved one has transcortical sensory aphasia, then when hearing a phrase such as, \"are you home?\" they might repeat a part of the question and say you home or respond to the question with the same phrase are you home?\"This type of aphasia is caused by injuries to areas of the brain which surround Wernickes language area, an area that plays a major role in co…
Prognosis
- Aphasia is one of the most difficult disabilities to live with after a stroke. There are several different speech patterns that can develop after a stroke, and they all make communication difficult, and possibly frustrating for a stroke survivor and loved ones.
Treatment
- Living with aphasia requires patience, as does caring for a stroke survivor who has aphasia. There are several approaches to speech therapy which can help improve speech and communication to help optimize daily life after a stroke. Be sure to convey your concerns about your speech problems to your medical team so that you can be directed to the best rehabilitation available t…