What is a ve alarm on a ventilator?
Low Minute Ventilation (Ve): This alarm will sound when the amount of air taken in perminute drops below a set value. It will act similar to a low pressure alarm and usually indicates some kind of a leak or disconnect in the system. High pressure alarm: This will sound when the pressure in the circuit has increased.
What is a mechanical ventilator?
Mechanical Ventilation. A mechanical ventilator is a machine that helps a patient breathe (ventilate) when he or she cannot breathe on his or her own for any reason.
What are the basic principles of mechanical ventilation?
Basics of Mechanical Ventilation. 1 Volume Controlled (volume limited, volume targeted) and Pressure is variable. 2 Pressure Controlled (pressure limited, pressure targeted) and Volume is variable. 3 Dual Controlled (volume targeted (guaranteed) pressure limited)
What are the components of airway pressure during mechanical ventilation?
Components of airway pressure during mechanical ventilation, illustrated by an inspiratory-hold maneuver. PEEP = positive end-expiratory pressure. Elastic pressure is the product of the elastic recoil of the lungs and chest wall (elastance) and the volume of gas delivered.

What does total ve mean on a ventilator?
Minute ventilation (VE) is the quantity of air moved into and out of the lungs in a minute and dictates CO2 elimination from alveoli.
What is VE on vent?
End-Tidal Volume (Vte): Is the amount of air the patient's lungs return to the ventilator with exhalation. Total Respiratory Rate: This includes breaths delivered by the ventilator and if they are able to breath on their own, the patient's natural breaths.
How is ve ventilation calculated?
Minute ventilation (VE) is the total volume of gas entering (or leaving) the lung per minute. It is equal to the tidal volume (TV) multiplied by the respiratory rate (f). Minute ventilation = VE = TV x f At rest, a normal person moves ~450 ml/breath x 10 breath/min = 4500 ml/min.
How is ve measured?
Minute Ventilation and Tidal Volume Minute ventilation (VE) is an important measurement that's related to tidal volume. It's a measurement of the volume of inhaled and exhaled air over 60 seconds. A typical adult VE ranges around 4 to 6 liters in 60 seconds.
What is VTE in ventilator normal range?
In a normal lung, the VDaw/Vte ratio is between 25% and 30%.
What is PIP and PEEP?
PEEP improves gas exchange by increasing the functional residual capacity, reduces the respiratory effort, lowers requirements for respiratory mixture oxygen, and enables to decrease the peak inspiratory pressure (PIP) without decreasing the mean airway pressure.
What is the formula for VE?
*VE is the total flow exhaled per minute. VE = VA + VD (all flows).
What is normal range of tidal volume?
Respiratory Rate, Tidal Volume, and Monitoring There are some differences in pulmonary mechanics between males and females. Mean tidal volume for males is 38.9 mL and mean tidal volume for females is 46 mL. The respiratory rate is similar: 38 breaths per minute for males and 40 for females.
How is total lung capacity calculated?
The total lung capacity (TLC) is the volume of gas in the lung at the end of a full inspiration. It is either calculated from: TLC = RV+IVC, or from: TLC = FRC+IC; the latter is the preferred method in body plethysmography. It can also be measured directly by the radiologic technique.
What is a good lung capacity?
Lung capacity or total lung capacity (TLC) is the volume of air in the lungs upon the maximum effort of inspiration. Among healthy adults, the average lung capacity is about 6 liters.
What is a normal inspiratory reserve volume?
1900-3300mlInspiratory Reserve Volume(IRV) It is the amount of air that can be forcibly inhaled after a normal tidal volume. IRV is usually kept in reserve, but is used during deep breathing. The normal adult value is 1900-3300ml.
What are the 4 lung volumes?
Background. Four standard lung volumes, namely, tidal (TV), inspiratory reserve (IRV), expiratory reserve (ERV), and residual volumes (RV) are described in the literature. Alternatively, the standard lung capacities are inspiratory (IC), functional residual (FRC), vital (VC) and total lung capacities (TLC).
What is VT on ventilator?
When AC mode is selected in the ventilator, four parameters may be quickly modified: Tidal Volume (VT) This is the set amount of volume that will be delivered with each breath.
What causes high VTE on ventilator?
Inadequate inflation of the tracheostomy tube cuff. Poorly fitting noninvasive masks or nasal pillows/prongs. Loose circuit and tubing connections. The patient demands higher levels of air than the ventilator is putting out.
How do I adjust my ventilator settings?
Initial ventilator settingsSet the machine to deliver the TV required (10 to 15 mL/kg).Adjust the machine to deliver the lowest concentration of oxygen to maintain normal PaO 2 (80 to 100 mm Hg). ... Record peak inspiratory pressure.Set mode (AC or SIMV) and rate according to the healthcare provider's order.More items...
What does a high tidal volume indicate?
Tidal volume is a measure of the amount of air a person inhales during a normal breath. Traditional preset tidal volumes higher than 10 ml/kg have been proved to be associated with increased risk of pulmonary barotrauma and should be avoided. High tidal volumes also decrease venous return and reduce cardiac output.
What Is A Mechanical Ventilator?
A mechanical ventilator is a machine that helps a patient breathe (ventilate) when he or she is recovering from surgery or critical illness, or can...
Why Do We Use Mechanical Ventilators?
A mechanical ventilator is mainly used to make it easier for very sick people to breathe. Another reason is to help raise the oxygen level for thes...
What Are The Benefits of Mechanical Ventilation?
The main benefits of mechanical ventilation are the following: 1. The patient doesn’t have to work as hard to breathe; 2. The patient's breathing h...
What Are The Risks of Mechanical Ventilation?
The main risk of mechanical ventilation is infection, as the artificial airway may allow germs to enter the lung. Another risk factor is lung damag...
What Procedures Can Help A Patient With An Artificial Airway Connected to A Mechanical Ventilator?
1. Suctioning: This is a procedure in which a catheter (a thin, hollow tube) is inserted into the breathing tube to help remove secretions and wast...
How Long Does The Patient Stay Connected to The Mechanical Ventilator?
The main purpose for using a mechanical ventilator is to allow the patient time to heal. Usually, as soon as a patient can breathe effectively on h...
Who Are The Caregivers Who Take Care of The Patient on A Mechanical Ventilator?
1. Physician: The physician is usually an anesthesiologist, pulmonologist, intensivist, or critical care physician. These doctors have special trai...
What is a mechanical ventilator?
A mechanical ventilator is a machine that helps a patient breathe (ventilate) when they are having surgery or cannot breathe on their own due to a critical illness. The patient is connected to the ventilator with a hollow tube (artificial airway) that goes in their mouth and down into their main airway or trachea. They remain on the ventilator until they improve enough to breathe on their own.
What is the medical term for a physician who treats mechanical ventilation?
Physician: The physician is usually an anesthesiologist, pulmonologist, or intensivist (critical care physician). These doctors have special training in the art and science of mechanical ventilation and take care of these patients every day.
Why is mechanical ventilation dangerous?
The main risk of mechanical ventilation is an infection, as the artificial airway (breathing tube) may allow germs to enter the lung. This risk of infection increases the longer mechanical ventilation is needed and is highest around two weeks. Another risk is lung damage caused by either over inflation or repetitive opening and collapsing of the small air sacs Ialveoli) of the lungs. Sometimes, patients are unable to be weaned off of a ventilator and may require prolonged support. When this occurs, the tube is removed from the mouth and changed to a smaller airway in the neck. This is called a tracheostomy. Using a ventilator may prolong the dying process if the patient is considered unlikely to recover.
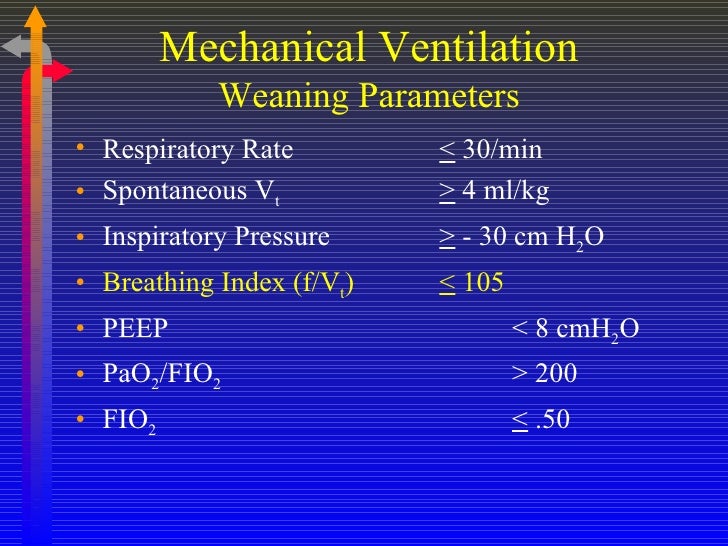
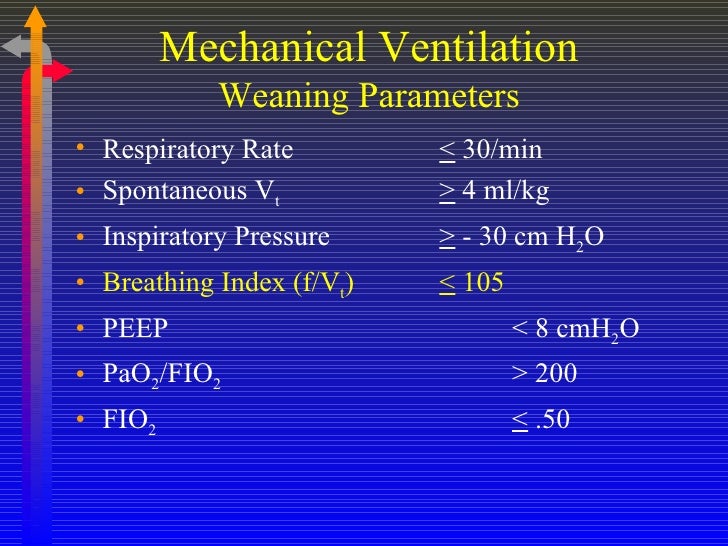
When do you take a patient off a ventilator?
Usually, as soon as a patient can breathe effectively on their own , they are taken off the mechanical ventilator. The caregivers will perform a series of tests to check the patient's ability to breathe on their own.
Does mechanical ventilation heal?
Preserves a stable airway and preventing injury from aspiration. It is important to note that mechanical ventilation does not heal the patient. Rather, it allows the patient a chance to be stable while the medications and treatments help them to recover.
How does mechanical ventilation work?
Mechanical ventilation works by applying a positive pressure breath and is dependent on the compliance and resistance of the airway system , which is affected by how much pressure must be generated by the ventilator to provide a given tidal volume (TV). The TV is the volume of air entering the lung during inhalation.[1] Compliance and resistance are dynamic and can be affected by the disease state(s) that led to the intubation. Understanding the changes in compliance and resistance will allow you to pick the proper ventilator strategies.
What are the stages of mechanical ventilation?
There are four stages of mechanical ventilation. There is the trigger phase, the inspiratory phase, the cycling phase, and the expiratory phase. The trigger phase is the initiation of an inhalation which is triggered by an effort from the patient or by set parameters by the mechanical ventilator. The inhalation of air into the patient defines the inspiratory phase. The cycling phase is the brief moment when inhalation has ceased but before exhalation has begun. The expiratory phase is the passive exhalation of air from the patient.
How to manage ventilator for obstructive patient?
The most important thing to accomplish when managing the ventilator for an obstructive patient is to increase the expiratory phase, allowing for more time to exhale, which will reduce auto-PEEP and dynamic hyperinflation. [1][3][11] It is important to recall that most patients will require deep sedation in order not to over-breathe the ventilator and inspire too often. The tidal volume should be set at 8ml/kg, while the respiratory rate should start at ten breaths per minute.[3] These settings will allow for ample time for a full expiration and hence decreased auto-PEEP, which tends to employ the above described permissive hypercapnia strategy by focussing on lowered tidal volumes and oxygenation over elevated PaCO2. The inspiratory flow rate should be set at 60 L/minute. FI02 should be set at 40% after the initiation of ventilation. As obstructive lung disease is typically a problem with ventilation and not oxygenation, the FIO2 should not need to be increased. Minimal PEEP should be employed, with some studies advocating for a PEEP of zero while some advocate for a small amount of PEEP to help overcome auto-PEEP. The plateau pressure should be less than 30.
How to set up APRV?
Setting up APRV requires adjusting four main variables, P-high, P-low, T-high, and T-low. [17][18] P-high is the continuous pressure set, while P-low is the pressure release part of the cycle. T-high is how long the continuous pressure is set to last, while T-low is the release phase duration. The patient should initially be set on AC/VC immediately post intubation until paralysis wears off. Then, an inspiratory hold should be performed to determine the plateau pressure. This plateau pressure becomes the P-high and should generally be around 27-29cm H2O, though obese patients may require higher pressure. The P-low is generally set to 0. However, there is generally intrinsic PEEP as full exhalation does not occur. The T-high is generally set to 4-6 seconds, while the T-low to .2-.8 seconds in restrictive lung disease and .8-1.5 seconds in obstructive lung disease. To properly set the T-low, you should examine the Flow-Time Waveform on the ventilator. The T-low should be set to approximately 75% of the Peak Expiratory Flow Rate (PEFR). [19][17](See Figure 3) The T-low needs to be continuously readjusted to 75% of the PEFR as lung recruits over time. FI02 should be titrated downwards once the patient is on APRV and comfortable.
What is APRV in CPAP?
APRV is a form of continuous positive airway pressure (CPAP) characterized by a timed pressure release while allowing for spontaneous breathing.[16] ( See Figure 1) While previously considered a rescue strategy, APRV has recently gained acceptance as a primary ventilatory mode. Its indications for Acute Lung Injury (ALI)/Acute Respiratory distress syndrome (ARDS), multifocal pneumonia, and severe atelectasis make it a very attractive ventilatory option.
How does APRV work?
APRV functions by providing continuous pressure to keep the lungs open with a timed-release to lower set pressure. [17][18] The continuous pressure phase of APRV transmits pressure to the chest wall, which allows for the recruitment of both proximal and distal alveoli. The prolonged continuous pressure phase with the short release phase avoids the continuous cycles of recruitment-derecruitment in pressure/volume control vent settings.[19] This helps to avoid atelectrauma, barotrauma, and resulting ventilator-induced lung injury.[19] ( See Figure 2) The timed release allows for a passive exhalation and improved clearance of CO2. Since APRV relies upon spontaneous ventilation, it requires less sedation than conventional modalities, thus mitigating adverse events due to sedation. Spontaneous breathing has the benefit of increasing end-expiratory lung volume, decreasing atelectasis, and improves ventilation to dependent lung regions. [19]Spontaneous breathing further improves the hemodynamic profile by decreasing intrathoracic pressure, thus improving preload and cardiac output.
What is obstructive lung disease?
Obstructive lung disease is characterized by narrowed airways and the collapse of the small airways on expiration . [1] This condition leads to increased airflow resistance and decreases the expiratory flow, resulting in more time required to exhale the tidal volume fully. If inhalation begins before the full tidal volume has been exhaled, then some residual air is left inside the chest. The intrathoracic pressure increases as more and more air gets trapped inside the alveoli. This pressure is termed auto-PEEP, and this pressure must be overcome during inhalation. As the amount of air trapped inside the chest increases, you have to flatten off the diaphragm and expand the lungs, decreasing compliance, called dynamic hyperinflation. As auto-PEEP and dynamic hyperinflation progress, there is an increased work of breathing, decreased efficiency of inhalation, and potential for hemodynamic instability due to the high intrathoracic pressure. Given these unique circumstances in OLD, the ventilator strategy employed must offset these pathologically increased intrathoracic pressures. Furthermore, ventilatory management must be combined with maximal medical therapy such as in-line nebulizers to reverse the obstructive process.
What is a Mechanical Ventilator?
As I mentioned, a Mechanical Ventilator is a machine that aids in a patient’s ability to ventilate. That’s where it gets its name. In other words, it helps the patient take in oxygen and remove carbon dioxide from the lungs.
What is Noninvasive Mechanical Ventilation?
Noninvasive ventilation (NIV) involves the administration of ventilatory support without using any type of invasive artificial airway. Instead, NIV uses a mask that tightly seals to the face in order to provide ventilatory support.
What is Ventilator-Associated Pneumonia?
Ventilator-Associated Pneumonia (VAP) is a lung infection that develops 48 hours or more after a patient has been intubated and placed on the ventilator.
How Long is a Patient Connected to a Ventilator?
As I mentioned earlier, the primary use of a Mechanical Ventilator is to keep the patient stable long enough to heal.
What are the Risks and Complications of Mechanical Ventilation?
While Mechanical Ventilation has its benefits, it also comes with associated risks and complications as well. Some of which can actually endanger a patient’s life. The following are the most common complications of Mechanical Ventilation:
What is the flow setting on a ventilator?
It’s a setting on the ventilator that can be adjusted depending on the patient’s inspiratory needs and demands.
What is a VAP in a ventilator?
Ventilator-Associated Pneumonia (VAP) – This condition is a lung infection that develops 48 hours or more after a patient has been intubated and placed on the ventilator.
When should mechanical ventilation be considered?
There are numerous indications for endotracheal intubation and mechanical ventilation (see table Situations Requiring Airway Control ), but, in general, mechanical ventilation should be considered when there are clinical or laboratory signs that the patient cannot maintain an airway or adequate oxygenation or ventilation.
What is the pressure gradient in mechanical ventilation?
In mechanical ventilation, the pressure gradient results from increased (positive) pressure of the air source.
How to reduce intrinsic PEEP?
If the cause is airflow limitation, intrinsic PEEP can be reduced by shortening inspiratory time (ie, increasing inspiratory flow) or reducing the respiratory rate , thereby allowing a greater fraction of the respiratory cycle to be spent in exhalation.
How much inspiratory flow should I use for a patient?
The inspiratory flow should generally be set at about 60 L/minute but can be increased up to 120 L/minute for patients with airflow limitation to facilitate having more time in exhalation, thereby limiting autoPEEP.
Where does resistance to airflow occur?
In the mechanically ventilated patient, resistance to airflow occurs in the ventilator circuit, the endotracheal tube, and, most importantly, the patient’s airways. (NOTE: Even when these factors are constant, an increase in airflow increases resistive pressure.)
Should mechanical ventilation be delayed?
However, mechanical ventilation should not be delayed until the patient is in extremis.
Is airway pressure fixed?
The resultant airway pressure is not fixed but varies with the resistance and elastance of the respiratory system and with the flow rate selected.
How many variables can a ventilator control?
Ventilator can control only one variable at a time.
Why is PEEP not used in ventilation?
Such patients illustrate why PEEP should not automatically be applied as treatment for hypoxemic respiratory failure. Respiratory system compliance is much higher in relatively normal areas of lung than in areas of consolidation or collapse. As a result, application of PEEP may preferentially expand these more normal areas and not produce the desired effect in the involved lung. Distention of normal lung tissue stretches and narrows pulmonary vessels, which can raise pulmonary vascular resistance sufficiently to divert blood to the abnormal areas. Accordingly, applying PEEP can worsen rather than improve arterial oxygenation in such instances.
What does flow mean in PC-CMV?
Flow (v̇) = Tidal Volume / Inspiratory time. Hence, in PC-CMV, when Inspiratory time is fixed and if tidal volumes are increased, that means flow rate is increased.
How to understand the equation of motion in volume control mode?
A set tidal volume/flow is delivered into the lungs. When air flows through the airways against the inherent resitance, it generates some pressure which is equal to flow x resistance. After air flows though the airways, it tries to open the alveoli against the elastic recoil thereby generating some pressure which is equal to the volume/ compliance. Then, finally you add the PEEP to these two pressures, it would give you the peak pressure.
What is the difference between PEEP and set pressure?
Understanding Equation of Motion in Pressure control mode ( PC-CMV): A set pressure is applied ( please note that driving pressure is the difference between set pressure and PEEP) to overcome the resistance and elastic recoil. Part of this driving pressure is used to overcome the resistance and thus air will flow into alveoli. The remaining pressure is used to overcome the elastic recoil force, resulting in alveolar distension. Now add the driving pressure to the extrinsic PEEP, you get the peak pressure.
Why is right ventricular afterload increased?
Impaired cardiac function due to reduced right ventricular preload as a result of raised mean intrathoracic pressure and increased right ventricular afterload because of increased lung volume (which may not happen if gas trapping does not occur and if tidal residual volumes are physiologic).
What is the work of breath?
Work of breath = Volume x Pressure. It is the work required to overcome the mechanical impedance to respiration. In other words, it is the work needed to overcome both elastic and airflow resistance. The time constant is a measure of the time needed for alveolar pressure to reach 63% of the change in airway pressure.
What is a Mechanical Ventilation System?
Mechanical Ventilation systems work by extracting stale air or supplying fresh air into rooms in a house or building. Systems such as mechanical ventilation heat recovery systems extract and supply. There are four different types of mechanical ventilation systems:
What is a D-MEV system?
A D-MEV is a Decentralised Mechanical Extract System which is designed to replace conventional bathroom fans and draw out moisture laden air from wet rooms such as bathrooms and utility rooms. D-MEV systems provide a more efficient and a quieter system than separate fans.
What is decentralised mechanical extract ventilation?
Decentralised Mechanical Extract Ventilation systems are low energy systems, they are usually installed in a bathroom wall or ceiling and extracts continuously at a normal low rate of ventilation.
How does MVHR work?
A MVHR system works to eliminate condensation and mould within a building by constantly ventilating a property.
How does a PIV system work?
It works by supply fresh filtered air a continuous rate throughout a property and is a very popular option in existing houses or landlord lets. In combating condensation, a PIV system reduces the risk of mould, damp and dust population which creates a range of health benefits like reducing risks of asthma and other respiratory issues.
What is a PIV unit?
Loft mounted PIV units use free solar energy generated from the natural solar gain in lofts which, in turn, maximises comfort and contributes to annual energy savings. By eliminating condensation, a PIV system created a fresh and healthier living environment.
How does a heat recovery unit work?
It works by supply and extracting airflows in and out of homes and buildings to ensure a better indoor air quality. Heat recovery units can recover up to 90% of normally lost heat depending on the unit and the application.
Respiratory Therapy Formulas and Equations
Alveolar Minute Ventilation (VA) VA = Respiratory Rate x (Tidal Volume – Deadspace)
Respiratory Therapy Calculations Practice Questions
1. What is the most important calculation for the TMC Exam? Ideal Body Weight (IBW) because it is needed to determine the patient’s initial tidal volume setting for mechanical ventilation. You will need to calculate a patient’s IBW multiple times on the TMC Exam.
Final Thoughts
So there you have it. You now have access to all of the most important Respiratory Therapy Formulas, Calculations, and Equations. You will probably be required to learn most of these in Respiratory Therapy School. Not to mention, some of them will be on the TMC Exam as well.