How do viruses invade cells?
New Biosensor Illuminates in Real-Time How Viruses Invade Cell Protein-Making Machinery
- Hijacking the host. Since viruses do not encode their own replication machinery, they hijack that of their host cells by stealing cellular machines called ribosomes, which are essential for making ...
- Cellular stress. ...
- Future COVID-19 applications. ...
How are viruses harmful to living cells?
- Viruses do not carry out binary fission or cell division the same way that the eukaryotic or prokaryotic cells do.
- Viruses lack a metabolic process or system of their own. Instead, they take advantage of the cellular and metabolic processes of their host cells to generate their own energy and ...
- They are not inhibited or killed by antibiotics. ...
Do viruses attach to any kind of cell?
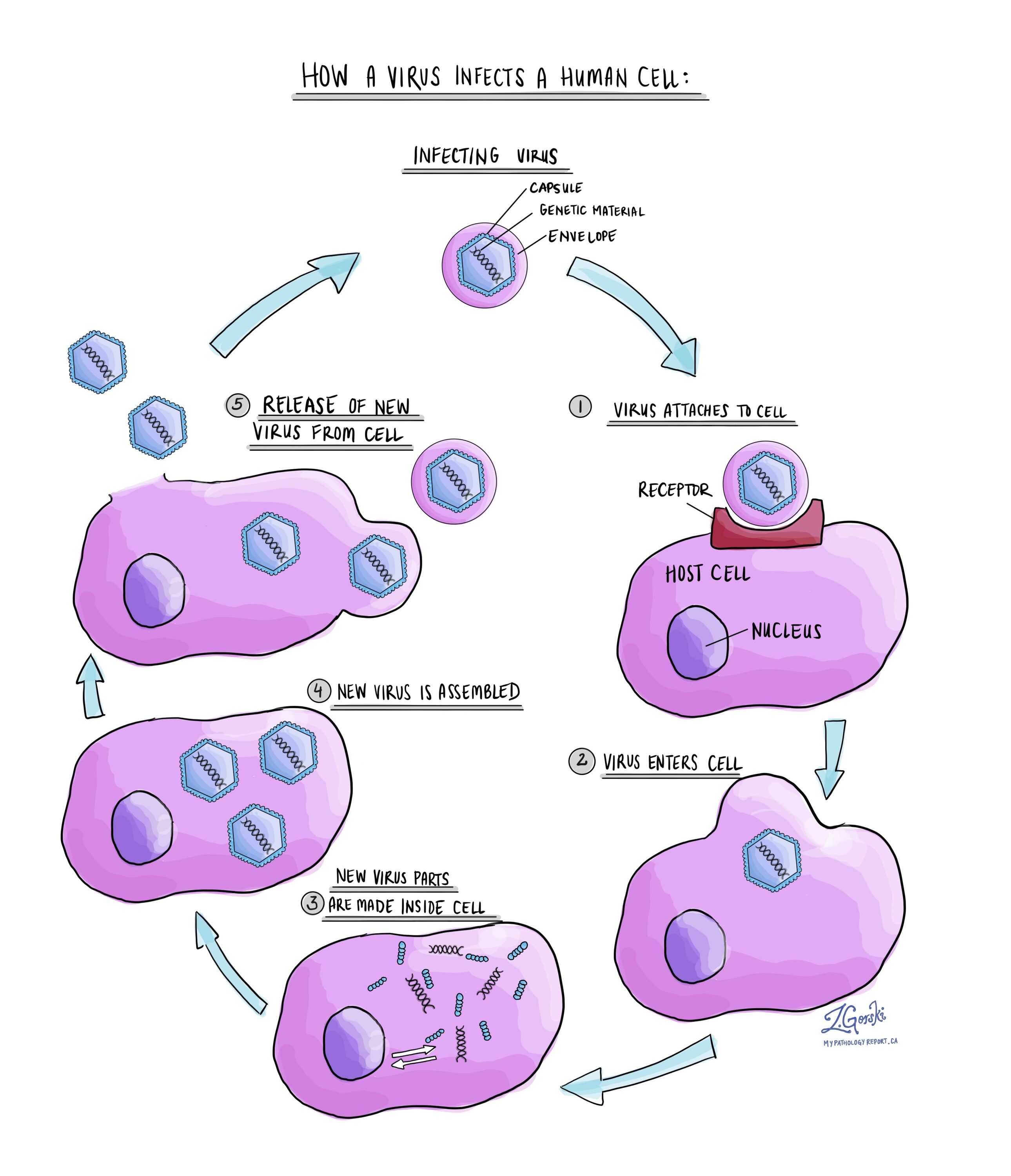
Viruses are obligate, intracellular parasites. A virus must first recognize and attach to a specific living cell prior to entering it. After penetration, the invading virus must copy its genome and manufacture its own proteins.
Do viruses require specific receptors to infect cells?
Viruses can infect only certain species of hosts and only certain cells within that host. Specific host cells that a virus must occupy and use to replicate are called permissive. In most cases, the molecular basis for this specificity is due to a particular surface molecule known as the viral receptor on the host cell surface.
What are the protein spikes in the virus envelope?
The protein spikes covering the virus's envelope allow it to bind to receptors on the host cell's lipid membrane, leading to infection and sometimes illness. Read more about testing for coronavirus infection on the Caltech Science Exchange >.
How many viruses are there in the world?
Scientists have identified more than 200 virus species with the potential to infect humans. New viruses are discovered every year. Some of them, such as SARS-CoV-2, the virus responsible for COVID-19, cause disease.
What to do if playback doesn't begin?
If playback doesn't begin shortly, try restarting your device.
Can a virus reproduce on its own?
Viruses cannot reproduce on their own. Instead, they depend on a host cell to reproduce. After entering the body (in the case of coronavirus, this is thought to occur through the nose, mouth, or eyes), a virus attaches itself to a host cell and inserts its genetic instructions.
What happens when a virus bursts out?
When the new virus particles are complete, the virus needs a way to release them to infect more cells. ‘Lytic’ viruses simply burst out, releasing all their virions in one huge pop and killing the cell in the process. ‘Lysogenic’ viruses release new virions one by one, allowing the host cell to survive and reproduce.
How many genes do viruses need?
The simplest living organisms need between 150 and 300 genes to make all the proteins they need to survive, but viruses get by on as few as four. They simply hijack other cells and turn them into virus factories. Viruses are clever; they make up for their genetic shortfall by borrowing from the cells they infect.
What are the two types of proteins that help viruses make more copies of their own genes?
The first are enzymes that enable the virus to construct more copies of its own genes. The second are proteins that interfere with the cell’s normal manufacturing processes. The third type are the structural proteins that work to build new virus particles.
How do cells make proteins?
They make temporary copies of their genes and pump them through molecular machines called ribosomes. These read the genetic code and use it as a template to assemble proteins. The simplest living organisms need between 150 and 300 genes to make all the proteins they need to survive, but viruses get by on as few as four. They simply hijack other cells and turn them into virus factories.
What are the most serious problems that viruses cause?
Some of the most serious problems arise when viruses infect immune cells, preventing the body from fighting back. Ebola, Marburg and HIV all harm the immune system.
How do viruses make copies of their genes?
This molecule is like DNA but with a different chemical letter, and it’s used by living cells to make temporary copies of genes. Some viruses also carry the code to make an enzyme called reverse transcriptase, which allows them to convert RNA into DNA inside a living cell.
What are the instructions for making a protective coat called?
Some of their most important genes provide the instructions to build proteins that make a protective coat called a capsid. The capsid proteins form repeating structures that lock together to make a 3D shape. This crystal-like patterning means that viruses only need a few genes to make a complete shield.
Why is energy needed in a bilayer?
Energy is also needed because of another fundamental property of bilayer membranes. Though bilayers are fluid, they don’t entirely behave like water or oil, in that they do not assume the shape of their container. Biological membranes have shapes that are determined by their precise lipids and the proteins associated with them (7). Work is required to force membranes out of their spontaneous shape, which is the shape of lowest energy. The fusion pore that connects the virus and cell is roughly an hourglass shape (8). The wall of a fusion pore is a membrane with components that are a mixture of the two original membranes. An hourglass shape deviates significantly from the spontaneous shape of the initial membranes that constitute the pore. The greater the diameter of the pore, the greater is the area of the lining membrane, and so pore expansion is a highly energy consuming process. Viral genetic material, the genome, is rather large, on the order of ∼100 nm. The initial fusion pore is only ∼1 nm, so considerably more membrane must line a pore as it enlarges to a size sufficient to allow passage of a viral genome from a virus to a cell interior. In fact, it appears that more energy is required for pore expansion than for hemifusion or pore formation.
Why is a virion engulfed into an endosome like a Trojan horse?
A virion engulfed into an endosome is like a Trojan horse, because the cell perceives the virus particle as food. Endosomes become increasingly acidified as they move from the cell surface further into the cell’s interior. Fusion of viruses within endosomes depends critically on the acidic environment.
How can infection be prevented?
Infection can be prevented if fusion of the viral envelope with the cell or endosomal membrane can be blocked. Similarly, if a vaccine can be directed against the viral fusion protein, infection can be prevented. Vaccines against the influenza virus, for example, target the fusion proteins of the virus.
How many copies of HIV are there?
Influenza virus, for example, typically contains 500–1000 copies, whereas HIV contains only about a dozen copies (1, 2). A virion’s machinery is so efficient that each cell infected by even a single virion can produce about a million new virions.
What is the shape of a fusion pore?
The fusion pore that connects the virus and cell is roughly an hourglass shape (8). The wall of a fusion pore is a membrane with components that are a mixture of the two original membranes. An hourglass shape deviates significantly from the spontaneous shape of the initial membranes that constitute the pore.
How do viruses get into the cell?
Some types of enveloped virus fuse directly to the cell’s outer (plasma) membrane , whereas others are engulfed whole by endocytosis or similar processes and then fuse their envelope with the membrane of the engulfing internal organelle (e.g., an endosome) to gain access to the interior of the cell. In either case, the genetic material of the virus has invaded the cell through the barrier of its membrane, and infection will inevitably follow (Fig. 1). Infection can be prevented if fusion of the viral envelope with the cell or endosomal membrane can be blocked. Similarly, if a vaccine can be directed against the viral fusion protein, infection can be prevented. Vaccines against the influenza virus, for example, target the fusion proteins of the virus.
How do viruses stick to the cell membrane?
Viruses initially stick to cell membranes through interactions unrelated to fusion proteins. The virus surfs along the fluid surface of the cell and eventually the viral fusion proteins bind to receptor molecules on the cell membrane (4). If only binding occurred, the two membranes would remain distinct.
How does interferon help fight off infection?
Interferon helps to fight off infection by interfering with viral replication and helping to activate immune cells. It also turns on a distinctive set of genes that help cells fight off infection. Previous studies have suggested that ACE2 plays a role in helping lung cells to tolerate damage, but this is the first time that ACE2 has been connected with the interferon response.
What is the protein that binds to a receptor on human cells called?
Not long after the SARS-CoV-2 outbreak began, scientists discovered that the viral “spike” protein binds to a receptor on human cells known as angiotensin-converting enzyme 2 (ACE2). Another human protein, an enzyme called TMPRSS2, helps to activate the coronavirus spike protein, to allow for cell entry. The combined binding and activation allows the virus to get into host cells.
Where did the data come from in the Human Cell Atlas?
Much of the data came from labs that belong to the Human Cell Atlas project, whose goal is to catalog the distinctive patterns of gene activity for every cell type in the human body. The datasets that the MIT team used for this study included hundreds of cell types from the lungs, nasal passages, and intestine. The researchers chose those organs for the Covid-19 study because previous evidence had indicated that the virus can infect each of them. They then compared their results to cell types from unaffected organs.
Which cells are responsible for the absorption of nutrients?
In the intestine, they found that cells called absorptive enterocytes, which are responsible for the absorption of some nutrients, express the RNAs for these two proteins more than any other intestinal cell type.
Which cells produce mucus?
In the nasal passages, the researchers found that goblet secretory cells, which produce mucus, express RNAs for both of the proteins that SARS-CoV-2 uses to infect cells. In the lungs, they found the RNAs for these proteins mainly in cells called type II pneumocytes.
Does interferon help with hepatitis?
Because interferon has so many beneficial effects against viral infection, it is sometimes used to treat infections such as hepatitis B and hepatitis C . The findings of the MIT team suggest that interferon’s potential role in fighting Covid-19 may be complex. On one hand, it can stimulate genes that fight off infection or help cells survive damage, but on the other hand, it may provide extra targets that help the virus infect more cells.
Does ACE2 turn on interferon?
Fighting infection. In their data, the researchers also saw a surprising phenomenon — expression of the A CE2 gene appeared to be cor related with activation of genes that are known to be turned on by interferon, a protein that the body produces in response to viral infection.
How does mRNA transcription work?
Transcription of IAV mRNAs by the viral polymerase. Viral mRNA transcription occurs when the viral ribonucleoproteins reach the host cell nucleus and is assisted by the association of the viral polymerase (PA subunit) with the cellular RNA polymerase II C-terminal domain (RNA pol II CTD). Transcription initiates by a “cap-snatching” mechanism where the PB2 subunit binds to the 5′ cap of a host mRNA (red). Cap binding positions the region of the mRNA 10–13 nucleotides downstream for cleavage by the endonuclease domain in the PA subunit. Following cleavage, a conformational shift repositions the acquired mRNA capped primer to the PB1 subunit where the 3′ end base-pairs with a complimentary sequence at the vRNA 3′ end. Following the priming event, the viral polymerase extends the mRNA transcript. The transcription is terminated by a “reiterative stuttering” process (depicted in the box), which occurs when the polymerase encounters the 5–7 consecutive uracil bases at the vRNA 5′ end. The “reiterative stuttering” function likely involves multiple cycles of dissociation and reannealing, and effectively polyadenylates [A(n)] the viral mRNA by continuously repositioning the elongating 3′ end on the uracil-rich region of the vRNA template.
How long does it take for a vRNA to enter the nucleus?
The cumulative results from these studies show that IAVs can deliver their vRNPs from the cell surface to the nucleus in approximately 1 h, with entry and fusion occurring rather quickly (~10 min), and nuclear import requiring the bulk of the time (85). A striking observation from these studies is the efficiency with which the eight vRNAs reach the nucleus, indicating how effectively vRNPs recruit the host nuclear import factors. Supporting this observation, it was shown that NP adaptation to the importin-α isoforms of a particular species is crucial for productive IAV infections (86). While the bulk of the vRNP trafficking work has been carried out using various immortalized cell lines, the potential species related differences, and the essential role of vRNP trafficking in reassortment, emphasize the need for further methodology development to examine the details of IAV entry in primary cells and tissue explants.
How do IAVs get into the host cell?
IAVs initiate the infection process by using the HA molecules on the viral envelope. Upon reaching a potential host cell, the HA receptor-binding site attaches the virus to surface glycoconjugates that contain terminal SA residues (Figure (Figure2A)2A) (18, 48, 49). IAVs then scan the cell surface for the proper sialylated “receptor” by using the sialidase function of NA to remove local SAs and liberate nonproductive HA associations (50). Currently, the “receptor’s” identity remains unknown, but it is generally thought that HAs from avian IAVs have higher specificity for receptors with α-2,3-linked SAs that have a “linear” presentation (51, 52), whereas HAs from human IAVs prefer an α-2,6 linkage, which results in a more “bent” presentation (Figure (Figure2A)2A) (53, 54). While these preferences correlate with SA linkages in the respective hosts (55), several studies have shown that matching HA receptor binding preferences with the SA linkages in a particular host is not essential for infection, but is more critical for transmission (56–59). This implies that the IAV “receptor” either displays significant cell tropism in the airways or that IAVs can potentially use more than one receptor.
What is the type of influenza?
Influenza viruses belong to the Orthomyxoviridaefamily and are classified as either type A, B, C, or the recently identified type D (1, 2) . Influenza A viruses (IAVs) and type B viruses (IBVs) contain 8, negative-sense, single-stranded viral RNA (vRNA) gene segments (Figure (Figure1A)1A) (3, 4), which encode transcripts for 10 essential viral proteins, as well as several strain-dependent accessory proteins (Figure (Figure1B).1B). In comparison, influenza type C and D viruses only possess seven vRNA gene segments, as the hemagglutinin–esterase fusion protein vRNA replaces the hemagglutinin (HA or H) and the neuraminidase (NA or N) vRNAs (1, 2). IAVs will be the main focus of this review since they are the primary agents responsible for influenza pandemics, and a major contributor to the annual influenza epidemics in the human population (5).
Why are IAVs under constant negative selection?
IAVs are also under constant negative selection due to the functional requirements of the viral proteins, and the constraints of the limited genome. Several roles have been reported for most of the IAV proteins. These include the function of HA in receptor binding, as well as membrane fusion, and viral release by the sialidase activity of NA. To perform these functions, the proteins need to correctly fold, oligomerize, and as for the genome itself, they have to be properly trafficked and packaged into new virions. Thus mutations that benefit one property may hinder another. The goal of this review is to highlight these functional requirements by providing a summary of the mechanisms IAVs have evolved to facilitate cell entry, replication, virion assembly and movement, with particular attention to how IAVs coordinate the infection process.
What is the constant evolution of surface antigens?
A significant challenge in battling IAVs is the constant evolution of the surface antigens (HA and NA) in response to pressure from the host immune system, which is referred to as antigenic drift and antigenic shift . Antigenic drift is most evident in circulating seasonal IAVs, where substitutions by the polymerase that cause mutations in the surface antigen epitopes have continuously been selected to enable reinfection of the same host (45). Antigenic shift is responsible for the development of the IAV pandemics, and it relies on the less frequent process of reassortment, which involves the exchange of vRNAs between two IAVs during co-infection of a cell (43, 46, 47). While reassortment can happen between two related IAVs, antigenic shift occurs when the reassortment process yields a new IAV subtype.
What are the subtypes of IAVs?
To date, 16 HA (H1-16) and 9 NA subtypes (N1-9) have been found in IAVs isolated from aquatic birds (13). Two additional subtypes for HA (H17 and H18) and NA (N10 and N11) have recently been identified in bats (38, 39), but in contrast to the HA and NA subtypes from the more traditional avian IAVs, these do not appear to recognize sialic acid (SA) (40–42). Despite the numerous possible subtype combinations, only three have consistently persisted in the human population, causing the following pandemics in the process: 1918 and 2009 (H1N1), 1957 (H2N2), and 1968 (H3N2) (43). Currently, only the H1N1 and H3N2 subtypes, as well as the two antigenically distinct IBV lineages (Victoria and Yamagata), are endemic in the human population (44), which is why many IAV vaccines include two representative IAV and IBV strains (5).