What spinal nerve controls the bowel?
Sacral nerves are located in the pelvic area just above the tailbone. These nerves control the muscles and organs that contribute to overall bowel control, such as the anal sphincter and pelvic floor.
Which nerve Innervates the large intestine?
The vagus nerve (CNX) enters the abdominal cavity via the oesophageal hiatus of the diaphragm to provide parasympathetic innervation to the large intestines.
Can nerve damage affect bowel movements?
A spinal cord injury or a nerve disease may damage the nerves that help control the lower part of your colon. This is the part of the body that sends solid waste out of the body. This condition gets in the way of your normal ability to store and get rid of waste. It often causes constipation and bowel accidents.
What Innervates the descending colon?
The hindgut-derived structures, which include the distal one-third of the transverse colon, descending, and sigmoid colon, receive parasympathetic, sympathetic, and sensory nerve innervation from the inferior mesenteric plexus.
What spinal nerves affect the colon?
(A) The colon and rectum are innervated by two distinct spinal pathways, the lumbar splanchnic and sacral pelvic nerves. The cell bodies of these splanchnic and pelvic afferents are located within the thoracolumbar (T10-L1) and lumbosacral (L6-S1) DRG, respectively.
Can neuropathy affect your colon?
Diabetic neuropathy may distort the control of intestinal motility, which can lead to diverse symptoms such as diarrhoea, constipation, intestinal distension and abdominal pain.
What nerve stimulates bowel movement?
The sacral nerves control your bladder, your bowel, your rectum and the muscles related to urinary and anal functions. By stimulating these nerves with a mild electric current, the neurostimulator helps your bowel, rectum and bladder to work as they should.
Can the vagus nerve affect your bowels?
When vagus function is out of whack, digestion is out of whack. Symptoms can include heartburn or GERD, IBD or inflammatory bowel disease like ulcerative colitis, and can prevent the body from healing Small Intestine Bacterial Overgrowth (SIBO), a frequent root cause of Irritable Bowel Syndrome (IBS).
Does sciatic nerve affect bowels?
Changes in bowel and/or bladder control These changes may include: An inability to control your bowel and/or bladder movements. Difficulty in passing urine, a reduced urinary sensation, a loss of desire to pass urine, or a poor stream.
What is the parasympathetic nerve supply to the descending colon?
pelvic nerveParasympathetic innervation to the descending colon and rectum is provided by the pelvic nerve, which exits from the spinal cord at segments S2-S4. The somatic pudendal nerve, also originating from segments S2-S4, innervates the external anal sphincter and pelvic floor musculature.
What does the vagus nerve innervate?
Functions. The vagus nerve has a very extensive distribution. Sensory: Innervates the skin of the external acoustic meatus and the internal surfaces of the laryngopharynx and larynx. Provides visceral sensation to the heart and abdominal viscera.
Does the colon have sensory nerves?
The colon and rectum are innervated by a surprisingly diverse and distinct set of sensory afferent subclasses. These afferents innervate all layers of the colon and rectum and have activation thresholds ranging from the imperceptible through to the noxious range.
What does the vagus nerve innervate?
Functions. The vagus nerve has a very extensive distribution. Sensory: Innervates the skin of the external acoustic meatus and the internal surfaces of the laryngopharynx and larynx. Provides visceral sensation to the heart and abdominal viscera.
What supplies the large intestine?
The large intestine is supplied by branches of the superior mesenteric artery (SMA), as follows:Ileocolic artery through its cecal and appendicular branches.Right colic artery, which has a descending (anastomoses with the cecal artery) and an ascending branch.More items...•
What is the parasympathetic nerve supply to the descending colon?
pelvic nerveParasympathetic innervation to the descending colon and rectum is provided by the pelvic nerve, which exits from the spinal cord at segments S2-S4. The somatic pudendal nerve, also originating from segments S2-S4, innervates the external anal sphincter and pelvic floor musculature.
What is the parasympathetic innervation of the sigmoid colon?
pelvic splanchnic nervesThe pelvic splanchnic nerves provide parasympathetic innervation to the descending and sigmoid colon, the rectum, and pelvic viscera via the inferior hypogastric plexus. Parasympathetic innervation to the colon and rectum increases peristalsis, and inhibits the internal anal sphincter to allow for defecation.
What is the function of the colon?
Function. The main task of the colon is the temporary storage and transport of the feces. Thereby it daily absorbs about 1 liter of water which leads to a thickening of the stool. Furthermore it absorbs sodium, potassium and chloride but can also secrete potassium into the lumen itself.
Which part of the colon is attached to the posterior abdominal wall?
From there the transverse colon runs intraperitoneally towards the spleen forming the left colic flexure. This part is attached to the posterior abdominal wall by the mesocolon and is therefore very flexible.
What are the parts of the colon?
The colon may be subdivided into four parts: ascending, transverse, descending and sigmoid colon. The ascending colon lies secondary retroperitoneally on the right side of the abdominal cavity and moves towards the right colic flexure at the bottom side of the liver. From there the transverse colon runs intraperitoneally towards ...
What are the morphological features of the sigmoid colon?
ascending. transverse. descending. sigmoid colon. You can recognize it easily through several distinct morphological features like semilunar folds and pouches called haustra . In addition, taeniae coli are specific to the colon together with appendices epiploicae.
What is the structure of the colon?
The colon has the typical histological structure as the digestive tube: mucosa , submucosa, muscularis and serosa/adventitia. The mucosa is lined by simple columnar epithelium (lamina epithelialis) with long microvilli. It is covered by a layer of mucus which aids the transport of the feces.
Which arteries supply the ascending and transverse colon?
Branches of the superior mesenteric artery ( right colic artery, middle colic artery and colic branch of ileocolic artery) supply the ascending and transverse colon. The descending and sigmoid colon are supplied by branches of the inferior mesenteric artery ( left colic artery and sigmoid arteries ). The middle and left colic arteries form the ...
Where does the colon begin?
It begins from the caecum at the ileocecal valve and ends in the rectum. The colon is about 1.5 meters long and frames the convolute of the small intestine in the abdominal cavity. However it can be shortened and lie quite flexibly in case of an incomplete rotation of the umbilical loop during embryogenesis.
Where does the neurovascular supply to the colon come from?
The neurovascular supply to the colon is closely linked to its embryological origin: Ascending colon and proximal 2/3 of the transverse colon – derived from the midgut. Distal 1/3 of the transverse colon, descending colon and sigmoid colon – derived from the hindgut.
What part of the digestive system is the colon?
The colon (large intestine) is the distal part of the gastrointestinal tract, extending from the cecum to the anal canal. It receives digested food from the small intestine, from which it absorbs water and electrolytes to form faeces.
What is the transverse colon?
Transverse Colon. The transverse colon extends from the right colic flexure to the spleen, where it turns another 90 degrees to point inferiorly. This turn is known as the left colic flexure (or splenic flexure). Here, the colon is attached to the diaphragm by the phrenicocolic ligament.
Which artery supplies the descending colon?
The descending colon is supplied by a single branch of the inferior mesenteric artery; the left colic artery . The sigmoid colon receives arterial supply via the sigmoid arteries (branches of the inferior mesenteric artery).
Which artery supplies the midgut?
As a general rule, midgut-derived structures are supplied by the superior mesenteric artery, and hindgut-derived structures by the inferior mesenteric artery. The ascending colon receives arterial supply from two branches of the superior mesenteric artery; the ileocolic and right colic arteries.
Where is the transverse colon located?
The transverse colon extends from the right colic flexure to the spleen, where it turns another 90 degrees to point inferiorly. This turn is known as the left colic flexure (or splenic flexure). Here, the colon is attached to the diaphragm by the phrenicocolic ligament.
How many parts does the colon have?
Anatomically, the colon can be divided into four parts – ascending, transverse, descending and sigmoid. These sections form an arch, which encircles the small intestine. In this article, we shall look at the anatomy of the colon – its anatomical structure and relations, neurovascular supply, and clinical correlations.
What is the innervation of the large intestine?
Innervation. The large intestine is innervated by intrinsic and extrinsic sources. Extrinsic innervation is received primarily by both the parasympathetic and sympathetic divisions of the autonomic nervous system.
What is the neurovascular supply of the large intestine?
Neurovascular supply of the large intestine. The large intestines (distal midgut and hindgut) mark the beginning of the terminal segment of the alimentary canal. It's initial portion comprises the the cecum and veriform appendix, which continues on as the ascending, transverse, descending and sigmoid colon.
Which artery supplies the colon?
The middle colic artery goes on to supply the colon from the right colic (hepatic) flexure, along the transverse colon almost to the left colic (splenic) flexure. The right colic artery typically arises independently from the superior mesenteric artery; but it may also be given off with the ileocolic artery.
Which artery travels inferolaterally?
The artery travels inferolaterally towards (but not reaching) the right iliac fossa. The superior mesenteric artery gives off the inferior pancreaticoduodenal artery posteriorly, the middle colic, right colic and ileocolic arteries from the right side and several anastomosing jejunoileal branches from the left side.
Where does the inferior ileocolic branch travel?
The inferior ileocolic branch travels to the ileocolic junction, where it gives of an anterior and a posterior caecal artery, and an appendicular artery before continuing to the left and anastomosing with the terminal segment of the superior mesenteric artery.
Where is the superior mesenteric vein?
The superior mesenteric vein lies just to the right of its artery. The relatively large trunk receives deoxygenated blood from the ileocecal junction to the proximal 2/3 of the transverse colon via the right colic, ileocolic and middle colic veins. The superior rectal vein travels superiorly to the left of its artery.
Where is the large intestine located?
The large intestine is a part of the midgut (from the ileocecal junction, the cecum and vermiform appendix to the proximal two-thirds of the transverse colon) and the hindgut (from the distal ⅓ of the transverse colon to the sigmoid colon). The midgut region receives arterial supply from the superior mesenteric artery and the hindgut is supplied by the inferior mesenteric artery.
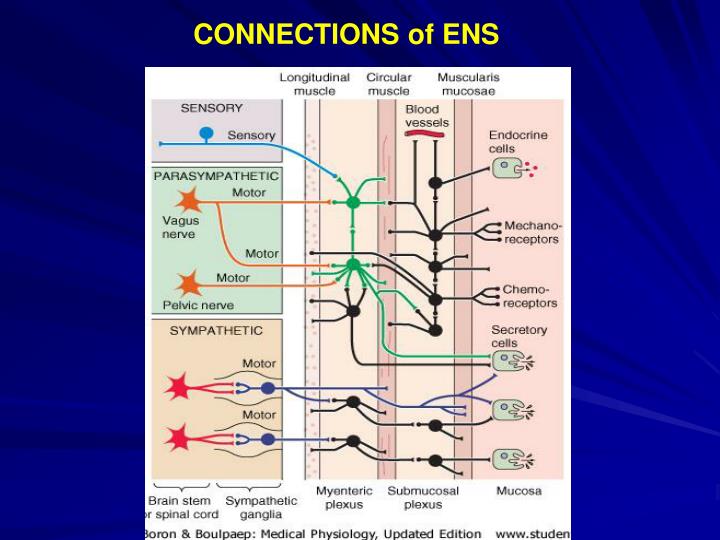
Parasympathetic Innervation
Down to the level of the transverse colon, parasym-pathetic innervation to the GI tract is supplied by the vagus nerve. The pelvic nerve innervates the descending colon, sigmoid colon, rectum, and anal canal (Fig. 2).
Sympathetic Innervation
Unlike the parasympathetic system, preganglionic fibers from the sympathetic system synapse outside of the GI tract in prevertebral ganglia (Fig. 2). Preganglionic, cholinergic efferent fibers from the cord synapse in four major ganglia: the celiac, superior mesenteric, inferior mesenteric, and hypogastric.
Intrinsic Innervation
Intrinsic innervation of the gut is provided by the enteric nervous system consisting primarily of the networks formed by the submucosal and myenteric plexuses. The elements of the enteric nervous system not only relay information to and from the gut via the parasympathetic and sympathetic systems, but also relay information along the gut.
Overview
The pudendal nerve is a major nerve in your pelvic region. This nerve sends movement (motor) and sensation information from your genital area. The pudendal nerve runs through .your pelvic floor muscles that support organs and ends at your external genitalia.
Function
The pudendal nerve is crucial for sensation and function in your pelvic region, including the genitals and anus. This nerve is part of your peripheral nervous system. Peripheral nerves send signals from your central nervous system (brain and spine) to your limbs and certain organs.
Anatomy
You have a pudendal nerve for each side of your body (left and right). The pudendal nerve arises from the sacral plexus in the very lowest part of your spine. The sacral plexus is a bundle of nerves located on the back of your pelvis.
Conditions and Disorders
Pressure on your pudendal nerve can cause pain or neuropathy (nerve damage).
