Insulin activates several signaling pathways that regulate gluconeogenesis
- IRS1 and IRS2. Among the numerous downstream signaling components of the insulin receptor, the insulin receptor substrates (IRS) play a key role in the regulation of hepatic glucose production.
- PI3K. ...
- PDK1. ...
- Akt. ...
- MAPK. ...
- CDC-like kinase. ...
How does gluconeogenesis happen?
In a nutshell, this is how gluconeogenesis happens: The raw materials (lactate, alanine, glutamine, or glycerol) go to the liver or kidney, where they are converted to pyruvate — the first substance in gluconeogenesis. In the mitochondria, pyruvate is turned into oxaloacetate.
What are the precursors of gluconeogenesis?
Gluconeogenesis is the pathway by which glucose is synthesized from non-carbohydrate metabolites. The principal gluconeogenic precursors are pyruvate and lactate, certain gluconeogenic amino acids, and glycerol, which is derived mainly from fat metabolism.
Which hormone triggers glycogenesis?
It is the hormone insulin that triggers glycogenesis. This particular hormone has a huge impact on the metabolism of glucose in the liver cells. It stimulates glycogenesis and at the same time inhibit the breakdown of glycogen into glucose (glycogenolysis). (4, 5, and 6)
What are the sources of gluconeogenesis in the liver?
The liver preferentially uses lactate, glycerol, and glucogenic amino acids (especially alanine) while the kidney preferentially uses lactate, glutamine and glycerol. Lactate from the Cori cycle is quantitatively the largest source of substrate for gluconeogenesis, especially for the kidney.

How is gluconeogenesis triggered?
Gluconeogenesis contributes to hepatic glucose production Starting from lactate or an α-keto acid derived from amino acid breakdown, pyruvate can be generated for gluconeogenesis. Pyruvate is converted via carboxylation to oxaloacetate in the mitochondria.
Which stimulates the gluconeogenesis?
hormone glucagonThe hormone glucagon stimulates gluconeogenesis and glycogenolysis.
What factors increase gluconeogenesis?
Gluconeogenesis is the formation of glucose from noncarbohydrate sources. The rate of gluconeogenesis increases when the blood sugar level is low, at the time of fasting, taking the low-carb diet, etc. Hormones like catecholamines, glucagon and glucocorticoids, etc. stimulate gluconeogenesis.
What is glycogenolysis triggered by?
Glycogenolysis occurs primarily in the liver and is stimulated by the hormones glucagon and epinephrine (adrenaline).
What activates glycolysis and inhibits gluconeogenesis?
When ADP and AMP are high (low ATP), this enzyme stimulates glycolysis and inhibits gluconeogenesis.
Which hormone stimulates gluconeogenesis and glycogenolysis?
GlucagonWhich hormone stimulates glycogenolysis and gluconeogenesis? Glucagon stimulates glycogenolysis and gluconeogenesis, thereby increasing blood sugar level. Glucagon also decreases cellular glucose uptake, therefore it is a hyperglycemic hormone.
Does cortisol stimulate gluconeogenesis?
In the liver, high cortisol levels increase gluconeogenesis and decrease glycogen synthesis.
What hormone regulates gluconeogenesis?
Insulin and glucagon are the most important hormones regulating hepatic gluconeogenesis. They demonstrated antagonistic effects on blood glucose levels.
What enzyme regulates gluconeogenesis?
PEPCK has been shown to be the key regulatory enzyme in gluconeogenesis as well as glyceroneogenesis, serine synthesis, and amino acid metabolism (Yang et al. 2009a). Both PEPCK transcription and enzyme activity are tightly regulated (Yang et al. 2009b).
Does glucagon stimulate glycogenolysis?
Specifically, glucagon promotes hepatic conversion of glycogen to glucose (glycogenolysis), stimulates de novo glucose synthesis (gluconeogenesis), and inhibits glucose breakdown (glycolysis) and glycogen formation (glycogenesis) (Fig.
What enzyme regulates glycogenolysis?
Glycogenolysis is the biochemical pathway in which glycogen breaks down into glucose-1-phosphate and glucose. The reaction takes place in the hepatocytes and the myocytes. The process is under the regulation of two key enzymes: phosphorylase kinase and glycogen phosphorylase.
What triggers glycogenolysis in muscle?
In muscle cells, glycogenolysis is stimulated by adrenaline, and regulated by positive and negative allosteric effectors, AMP and calcium ion (Ca2+), and ATP and glucose 6-phosphate, respectively.
Where does gluconeogenesis occur?
During the first 18 to 24 hours of a fast, the vast majority of gluconeogenesis occurs in the liver. Following prolonged periods of starvation, however, the kidneys adapt to generate as much as 20% of total glucose produced. Only the liver and kidney can release free glucose from glucose 6-phosphate; other tissues lack the enzyme glucose 6-phosphatase. [1][2]
How do gluconeogenic amino acids enter gluconeogenesis?
Glucogenic amino acids enter gluconeogenesis via the citric acid cycle. Glucogenic amino acids are catabolized into citric acid cycle metabolites such as alpha-ketoglutarate, succinyl CoA, and fumarate. Through the citric acid cycle, these alpha-ketoacids converts to oxaloacetate, the substrate for the gluconeogenic enzyme PEP carboxykinase.
How does glucagon affect glucose production?
It regulates glucose production by altering the activity of both glycolytic and gluconeogenic enzymes. In response to glucagon, fructose 1,6-bisphosphatase activity is upregulated while its glycolytic counterpart, phosphofructokinase-1, is suppressed.[6] Moreover, glucagon binds to an extracellular G protein-coupled receptor that results in the activation of adenylate cyclase and a subsequent increase in the concentration of cAMP. [7]cAMP activates cAMP-dependent protein kinase, which then phosphorylates and inactivates the glycolytic enzyme pyruvate kinase. Pyruvate kinase is the enzyme responsible for converting PEP to pyruvate, one of the irreversible reactions of glycolysis. Lastly, glucagon upregulates expression of the gene encoding PEP-carboxykinase, further increasing PEP concentrations and favoring glucose production. [7]
What enzymes are involved in gluconeogenesis?
However, to bypass the three highly exergonic (and essentially irreversible) steps of glycolysis, gluconeogenesis utilizes four unique enzymes.[1] The enzymes unique to gluconeogenesis are pyruvate carboxylase, PEP carboxykinase, fructose 1,6-bisphosphatase, and glucose 6-phosphatase. Because these enzymes are not present in all cell types, gluconeogenesis can only occur in specific tissues. In humans, gluconeogenesis takes place primarily in the liver and, to a lesser extent, the renal cortex. [2]
How is gluconeogenesis regulated?
Due to the highly endergonic nature of gluconeogenesis, its reactions are regulated at a variety of levels. The bulk of regulation occurs through alterations in circulating glucagon levels and availability of gluconeogenic substrates. However, fluctuations in catecholamines, growth hormone, and cortisol levels also play a role. [4][5]
What enzyme is responsible for phosphorylation of 3-phosphoglycerate?
3-phosphoglycerate is phosphorylated via the enzyme phosphoglycerate kinase to form 1,3-bisphosphoglycerate. This reaction requires ATP as an activating molecule.
Which organs use glucose as their primary fuel?
Some organs, such as the brain, the eye, and the kidney, contain tissues that utilize glucose as their preferred or sole metabolic fuel source. During a prolonged fast or vigorous exercise, glycogen stores become depleted, and glucose must be synthesized de novo in order to maintain blood glucose levels. Gluconeogenesis is the pathway by which glucose is formed from non-hexose precursors such as glycerol, lactate, pyruvate, and glucogenic amino acids. [1]
Where does gluconeogenesis occur?
Gluconeogenesis occurs in the liver and kidneys. Gluconeogenesis supplies the needs for plasma glucose between meals. Gluconeogenesis is stimulated by the diabetogenic hormones (glucagon, growth hormone, epinephrine, and cortisol). Gluconeogenic substrates include glycerol, lactate, propionate, and certain amino acids. PEP carboxykinase catalyzes the rate-limiting reaction in gluconeogenesis. The dicarboxylic acid shuttle moves hydrocarbons from pyruvate to PEP in gluconeogenesis. Gluconeogenesis is a continual process in carnivores and ruminant animals, therefore they have little need to store glycogen in their liver cells. Of the amino acids transported to liver from muscle during exercise and starvation, Ala predominates. b-Aminoisobutyrate, generated from pyrimidine degradation, is a (minor) gluconeogenic substrate.
How does gluconeogenesis work?
Gluconeogenesis is a costly metabolic process. Conversion of two molecules of pyruvate to one of glucose consumes six high-energy phosphate bonds (4ATP+2GTP→4ADP+2GDP+6P i) and results in the oxidation of two NADH molecules ( Figure 14.1 ). In contrast, glycolytic metabolism of one molecule of glucose to two of pyruvate produces two high-energy phosphate bonds (2ADP+2P i →2ATP) and reduces two molecules of NAD +. For gluconeogenesis to operate, the precursor supply and the energy state of the tissue must be greatly increased. Using some gluconeogenic precursors to provide energy (via glycolysis and the TCA cycle) and to convert the remainder of the precursors to glucose would be inefficient, even under aerobic conditions. Usually, the catabolic signals (catecholamines, cortisol, and increase in glucagon/insulin ratio) that increase the supply of gluconeogenic precursors also favor lipolysis, which provides fatty acids to supply the necessary ATP.
What is the process of synthesis of glucose?
Gluconeogenesis is defined as the de novo synthesis of glucose from nonhexose precursors. Gluconeogenesis does not include the conversion of fructose or galactose into glucose in the liver or the generation of glucose from glycogen via glycogenolysis.
What is the role of PEP in gluconeogenesis?
PEP carboxykinase catalyzes the rate-limiting reaction in gluconeogenesis. The dicarboxylic acid shuttle moves hydrocarbons from pyruvate to PEP in gluconeogenesis. Gluconeogenesis is a continual process in carnivores and ruminant animals, therefore they have little need to store glycogen in their liver cells.
What is the synthesis of glucose from nonsugar precursors?
Gluconeogenesis. Gluconeogenesis is the synthesis of glucose from nonsugar precursors, such as lactate, pyruvate, and the carbon skeleton of glucogenic amino acids. From: Encyclopedia of Endocrine Diseases (Second Edition), 2018. Download as PDF.
What are the four reactions of gluconeogenesis?
The four unique reactions of gluconeogenesis are pyruvate carboxylase, located in the mitochondrial matrix, phosphoenolpyruate (PEP) carboxykinase located in mitochondrial matrix and cytosol, fructose-1, 6-bisphosphatase located in the cytosol and glucose-6-phosphatase located in the endoplasmic reticulum (ER). View chapter Purchase book.
How many enzymes are involved in the conversion of pyruvate to phosphoenolpyruv?
Conversion of pyruvate to phosphoenolpyruvate involves two enzymes and the transport of substrates and reactants into and out of the mitochondrion. In glycolysis, conversion of phosphoenolpyruvate to pyruvate results in the formation of one high-energy phosphate bond. In gluconeogenesis, two high-energy phosphate bonds are consumed (ATP→ADP+P i; GTP→GDP+P i) in reversing the reaction. Gluconeogenesis begins when pyruvate, generated in the cytosol, is transported into the mitochondrion—through the action of a specific carrier—and converted to oxaloacetate:
What happens to the body during gluconeogenesis?
During gluconeogenesis, the liver (and occasionally the kidneys) turns non-sugar compounds like amino acids (the building blocks of protein), lactate, and glycerol into sugar that the body uses a fuel. When glycogen (your body’s sugar storage) is low, protein intake is high, or the body is under stress, amino acids from your meals and your muscle become one of your main energy sources.
How to minimize gluconeogenesis?
One of the simplest ways to do this is by combining fasted exercise and intermittent fasting together.
What About Protein Timing for Ketosis?
When you eat your protein is as important as how much protein you eat. To figure out when you should eat your protein, we must understand what happens when we consume a high-protein meal.
How to shift body into ketogenesis?
To shift your body into ketogenesis and away from gluconeogenesis more quickly, it is best to combine the ketogenic diet with fasted exercise and intermittent fasting.
Why are you not in ketosis?
Gluconeogenesis from Excess Protein — The Reason Why You Are Not In Ketosis Yet. Although the ketogenic diet does not contain many insulin-raising carbohydrates, insulin levels will still be higher on a ketogenic diet than during a fast.
Why does it take longer to use ketogenesis?
This is because of the effect that consuming protein has on insulin levels.
Why does insulin affect ketosis?
When insulin levels are higher than normal, it limits the body’s ability to get into ketosis. This is because insulin keeps body fat and ketones from being used as energy. As a result, the liver will favor gluconeogenesis over ketogenesis.
Where does gluconeogenesis occur?
In vertebrates, gluconeogenesis occurs mainly in the liver and, to a lesser extent, in the cortex of the kidneys.
How does insulin affect gluconeogenesis?
Insulin counteracts glucagon by inhibiting gluconeogenesis. Type 2 diabetes is marked by excess glucagon and insulin resistance from the body. Insulin can no longer inhibit the gene expression of enzymes such as PEPCK which leads to increased levels of hyperglycemia in the body. The anti-diabetic drug metformin reduces blood glucose primarily through inhibition of gluconeogenesis, overcoming the failure of insulin to inhibit gluconeogenesis due to insulin resistance.
Why is oxaloacetate converted to malate?
Therefore, in species that lack intra-mitochondrial PEPCK, oxaloacetate must be converted into malate or aspartate, exported from the mitochondrion, and converted back into oxaloacetate in order to allow gluconeogenesis to continue. Gluconeogenesis pathway with key molecules and enzymes.
How is lactate converted into glucose?
Lactate is transported back to the liver where it is converted into pyruvate by the Cori cycle using the enzyme lactate dehydrogenase. Pyruvate, the first designated substrate of the gluconeogenic pathway, can then be used to generate glucose. Transamination or deamination of amino acids facilitates entering of their carbon skeleton into the cycle directly (as pyruvate or oxaloacetate), or indirectly via the citric acid cycle. The contribution of Cori cycle lactate to overall glucose production increases with fasting duration. Specifically, after 12, 20, and 40 hours of fasting by human volunteers, the contribution of Cori cycle lactate to gluconeogenesis was 41%, 71%, and 92%, respectively.
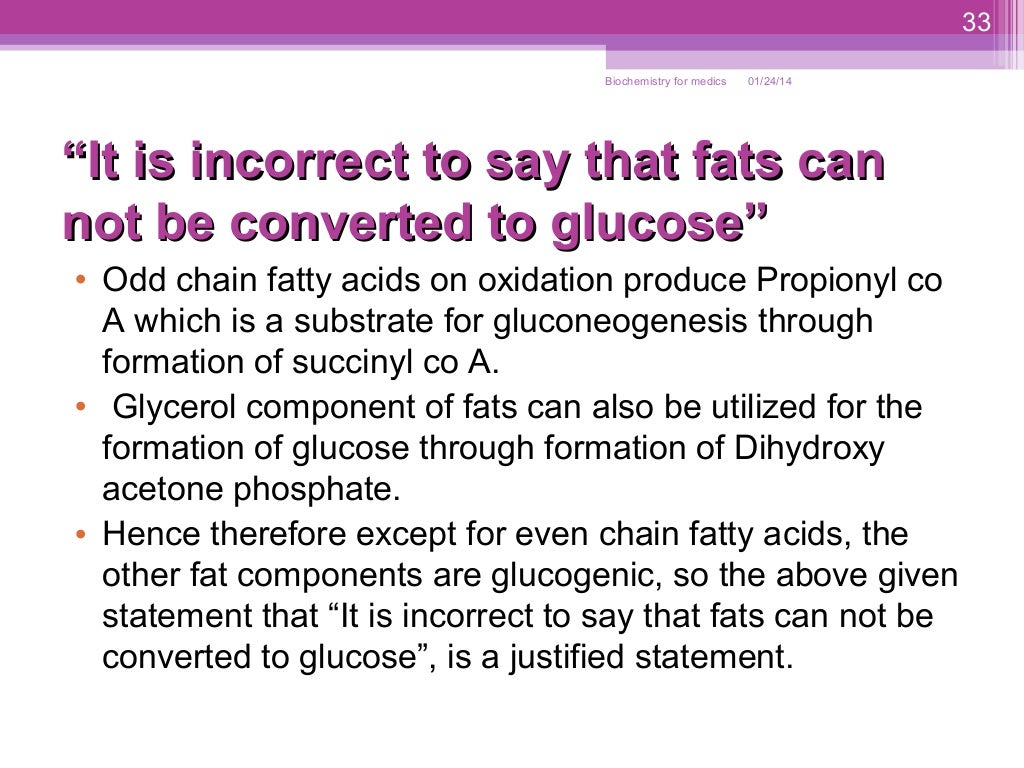
What are the substrates of gluconeogenesis?
For the breakdown of proteins, these substrates include glucogenic amino acids (although not ketogenic amino acids ); from breakdown of lipids (such as triglycerides ), they include glycerol, odd-chain fatty acids (although not even-chain fatty acids, see below); and from other parts of metabolism they include lactate from the Cori cycle. Under conditions of prolonged fasting, acetone derived from ketone bodies can also serve as a substrate, providing a pathway from fatty acids to glucose. Although most gluconeogenesis occurs in the liver, the relative contribution of gluconeogenesis by the kidney is increased in diabetes and prolonged fasting.
Why does gluconeogenesis occur in ruminants?
In ruminants, because dietary carbohydrates tend to be metabolized by rumen organisms, gluconeogenesis occurs regardless of fasting, low-carbohydrate diets, exercise, etc. In many other animals, the process occurs during periods of fasting, starvation, low-carbohydrate diets, or intense exercise. In humans, substrates for gluconeogenesis may come ...
What is the ketone body in ketosis?
During ketosis, however, acetyl-CoA from fatty acids yields ketone bodies, including acetone, and up to ~60% of acetone may be oxidized in the liver to the pyruvate precursors acetol and methylglyoxal. Thus ketone bodies derived from fatty acids could account for up to 11% of gluconeogenesis during starvation.
Where does gluconeogenesis occur?
Very simply put, it is often the conversion of protein or fat to sugar for the body to use as fuel. Gluconeogenesis occurs in the liver and the kidneys and can be seen as the reverse anabolic process of glycolysis—the breakdown, and extraction of energy from glucose.
Where does gluconeogenesis take place?
The process of gluconeogenesis takes place primarily in the liver, where glucose is made from amino acids (protein), glycerol (the backbone of triglycerides, the primary fat storage molecule), and glucose metabolism intermediaries like lactate and pyruvate. 1 .
What is the difference between ketosis and gluconeogenesis?
Those on a very low carb diet are often familiar with a metabolic state called ketosis which is another way of providing fuel to the body if not enough glucose is present. However, ketosis is a metabolic state that differs from the process known as gluconeogenesis. During ketosis, the body essentially learns ...
How are gluconeogenesis and ketogenesis similar?
Ketogenesis and gluconeogenesis are similar in that they are both chemical processes that provide energy to the body when not enough carbohydrate is present in the diet. However, ketogenesis differs in that it produces ketones to be used as fuel, rather than glucose.
Why is gluconeogenesis important?
Gluconeogenesis is a workaround for your body's metabolism to get and maintain the energy it needs to conduct normal bodily functions. People on a low-carb diet have less glucose available for energy because less carbohydrate is consumed. Gluconeogenesis is the body's way of providing energy to the body when glucose is not supplied through the diet.
What is the purpose of pyruvate in glycolysis?
During glycolysis, glucose is split into smaller molecules (called pyruvate) for use as energy throughout the body. Gluconeogenesis ensures that in the absence of glucose from glycolysis that critical limits of glucose are maintained when carbohydrate is absent. Your body's preferred energy source is glucose.
What is the process of synthesizing glucose in the body from non-carbohydrate precursors?
Gluconeogen esis vs. Ketosis. Gluconeogenesis is the process of synthesizing glucose in the body from non-carbohydrate precursors. It is the biosynthesis of new glucose, not derived from the consumption of carbohydrate. Very simply put, it is often the conversion of protein or fat to sugar for the body to use as fuel.
When to use gluconeogenesis or glycogenolysis?
Glycogenolysis is more often used during shorter periods of fasting, such as when a person’s blood sugar drops in between meals or after a good night’s sleep, while gluconeogenesis is used during long periods of fasting.
What is the difference between glycogenolysis and gluconeogenesis?
The main difference between glycogenolysis and gluconeogenesis is that glycogenolysis involves the formation of glucose molecules from a glucose source (glycogen), while gluconeogenesis forms glucose from non-glucose sources, molecules that are not made up of glucose. Also, glycogenolysis is an exergonic process; it releases energy.
What is the process of converting glucose into glucose?
Glycogenolysis is another process that is used when glucose levels in the blood are low. During glycogenolysis, the storage molecule glycogen—which is made up of long chains of glucose—is broken down into glucose which then enters the blood. The main difference between glycogenolysis and gluconeogenesis is that glycogenolysis involves ...
What is the opposite of gluconeogenesis?
Glycolysis is the opposite of gluconeogenesis. It is the breakdown of glucose, and is used in order to form ATP. Choice A, glycogenolysis, is the breakdown of the storage molecule glycogen into glucose. Choice B, glycogenesis, is the formation of glycogen chains from glucose molecules. Choice C, glyceroneogenesis, ...
What happens to blood sugar levels without food?
Without food intake, blood sugar levels become low. During this time, the body does not have an excess of carbohydrates from food that it can break down into glucose, so it uses other molecules for the process of gluconeogenesis such as amino acids, lactate, pyruvate, and glycerol instead. Once glucose is produced through gluconeogenesis in ...
Why do we need glucose?
Glucose levels in the blood must be maintained because it is used by cells to make the energy molecule adenosine triphosphate (ATP). Gluconeogenesis occurs during times when a person has not eaten in a while, such as during a period of famine or starvation. Without food intake, blood sugar levels become low. During this time, the body does not have an excess of carbohydrates from food that it can break down into glucose, so it uses other molecules for the process of gluconeogenesis such as amino acids, lactate, pyruvate, and glycerol instead. Once glucose is produced through gluconeogenesis in the liver, it is then released into the bloodstream, where it can travel to cells of other parts of the body so that it may be used for energy.
Which organelle does gluconeogenesis take place in?
D. Mitochondria. Answer to Question #3. C is correct. Gluconeogenesis mainly takes place in the liver, although some gluconeogenesis also takes place in the kidneys. While it does specifically occur in choice D, mitochondria, the mitochondria are cell organelles, not a body organ.
When Does Gluconeogenesis Happen?
Gluconeogenesis is always happening, however, it increases significantly when your carb consumption is low.
What Is Gluconeogenesis?
Gluconeogenesis (GNG) is a metabolic pathway that allows your liver and kidneys to make glucose from non-carbohydrate sources. It’s always happening in your body, but its rate can increase or decrease depending on your metabolic state.
Why doesn't fasting happen during fat adaptation?
This doesn’t happen during fasting or in the fat adaptation period because your body is using all the glucose from gluconeogenesis for fuel. On keto, your body already has a better, cleaner fuel — ketones –, so it can afford to store up excess glucose as glycogen.
Why can't protein activate gluconeogenesis?
To answer the first part of the question, protein can’t “activate” gluconeogenesis because GNG is already happening during ketosis, as you learned above.
What is the gluconeogenesis rate of the liver?
Glycerol: 0.53 μmol/ (kg min). The liver makes 68% while the kidneys make 32%. The gluconeogenesis rate from the liver and kidneys also change the longer you fast: after an overnight fast, most glucose comes from the liver. After a short fast, the liver and kidneys make equal amounts.
What is the name of the process that allows the liver and kidneys to make glucose?
Gluconeogenesis (GNG) is a metabolic pathway that allows your liver and kidneys to make glucose from non-carbohydrate sources. It’s always happening in your body, but its rate can increase or decrease depending on your metabolic state. Its name has three components: Gluco: Meaning glucose. Neo: Meaning new.
What amino acids are used in gluconeogenesis?
The main amino acids used for gluconeogenesis are alanine and glutamine. On average, you need 1.6 g of amino acids to make 1 g of glucose, which is expensive. That’s one of the reasons your body uses ketones during a ketogenic diet instead of amino acid-derived glucose. More on that later.
What is the difference between gluconeogenesis and Glycogenesis?
Glycogenesis is the formation of glycogen from glucose whereas gluconeogenesis is the formation of glucose from smaller molecules. (3, 4)
What is glycogenesis?
It is a process by which glycogen is formed from glucose. Glycogen is synthesized accordingly as per the demand of energy. If there is a sufficient amount of insulin in the body, excess glucose will not be used and will only be stored in the form of glycogen.
What is the purpose of Glycogenesis?
The primary purpose of glycogenesis is to make sure the body does not run out of glucose. Glucose is important as it is the body’s primary source of energy. Without an adequate supply of glucose in the body, vital organs will eventually shut down. (3, 4)
How is glycogen formed?
It is a process by which glycogen is formed from glucose. Glycogen is synthesized accordingly as per the demand of energy. If there is a sufficient amount of insulin in the body, excess glucose will not be used and will only be stored in the form of glycogen.
What is the reaction of glucose phosphorylation?
Glucose phosphorylation – In the initial phase, glucose is phosphorylated into glucose-6-phosphate, a usual reaction in glycolysis. It is catalyzed by glucokinase (liver) and hexokinase (muscle). Conversion of Glc-6-P to Glc-1- P – An enzyme Phosphoglucomutase will catalyze the conversion of Glucose-6-P is converted to Glc-1-Phosphate.
Why is glycogenesis important?
The primary purpose of glycogenesis is to make sure the body does not run out of glucose. Glucose is important as it is the body’s primary source of energy. Without an adequate supply of glucose in the body, vital organs will eventually shut down. (3, 4)
How many molecules of ATP are needed for glycogenesis?
The process of glycogenesis utilizes two molecules of ATP. One molecule is needed for glucose phosphorylation and another molecule is needed to convert UDP to UTP.
Overview
Regulation
While most steps in gluconeogenesis are the reverse of those found in glycolysis, three regulated and strongly endergonic reactions are replaced with more kinetically favorable reactions. Hexokinase/glucokinase, phosphofructokinase, and pyruvate kinase enzymes of glycolysis are replaced with glucose-6-phosphatase, fructose-1,6-bisphosphatase, and PEP carboxykinase/pyruvate carboxylase. These enzymes are typically regulated by similar molecules, but with opp…
Precursors
In humans the main gluconeogenic precursors are lactate, glycerol (which is a part of the triglyceride molecule), alanine and glutamine. Altogether, they account for over 90% of the overall gluconeogenesis. Other glucogenic amino acids and all citric acid cycle intermediates (through conversion to oxaloacetate) can also function as substrates for gluconeogenesis. Generally, human consumption o…
Location
In mammals, gluconeogenesis has been believed to be restricted to the liver, the kidney, the intestine, and muscle, but recent evidence indicates gluconeogenesis occurring in astrocytes of the brain. These organs use somewhat different gluconeogenic precursors. The liver preferentially uses lactate, glycerol, and glucogenic amino acids (especially alanine) while the kidn…
Pathway
Gluconeogenesis is a pathway consisting of a series of eleven enzyme-catalyzed reactions. The pathway will begin in either the liver or kidney, in the mitochondria or cytoplasm of those cells, this being dependent on the substrate being used. Many of the reactions are the reverse of steps found in glycolysis.
• Gluconeogenesis begins in the mitochondria with the formation of oxaloacetate by the carboxyl…
Insulin resistance
In the liver, the FOX protein FOXO6 normally promotes gluconeogenesis in the fasted state, but insulin blocks FOXO6 upon feeding. In a condition of insulin resistance, insulin fails to block FOXO6 resulting in continued gluconeogenesis even upon feeding, resulting in high blood glucose (hyperglycemia).
Insulin resistance is a common feature of metabolic syndrome and type 2 diabetes. For this reas…
See also
• Bioenergetics
External links
• Overview at indstate.edu
• Interactive diagram at uakron.edu
• The chemical logic behind gluconeogenesis
• metpath: Interactive representation of gluconeogenesis