What was schizophrenia called in the 1800s?
The first, formal description of schizophrenia as a mental illness was made in 1887 by Dr. Emile Kraepelin. He used the term "dementia praecox" to describe the symptoms now known as schizophrenia. Dementia praecox means "early dementia".
Who first used schizophrenia mental illness?
Paul Eugen Bleuler and the origin of the term schizophrenia (SCHIZOPRENIEGRUPPE)
How was schizophrenia viewed in the past?
Middle ages. Symptoms associated with schizophrenia — like psychosis and hallucinations — were commonly viewed as proof of demonic possession and sin throughout Europe in the Middle Ages. However, some medieval sources indicate that these mental health conditions were thought to be caused by: imbalances in the body.
How was schizophrenia treated in the 1920s?
Febrile illnesses such as malaria had been observed to temper psychotic symptoms, and in the early 20th century, 'fever therapy' became a common form of treatment for schizophrenia. Psychiatrists attempted to induce fevers in their patients, sometimes by means of injections of sulphur or oil.
What famous person suffers from schizophrenia?
Eduard Einstein The youngest child of Albert Einstein was studying medicine when he was diagnosed with schizophrenia at age 20. He spent many years in and out of a psychiatric clinic in Zurich, Switzerland.
How did they treat schizophrenia in the 1950s?
During the 1940s and 1950s insulin coma treatment, leucotomy and convulsive therapy were all used to treat schizophrenia in the UK and many other countries. Today insulin coma and leucotomy are not used at all in psychiatry.
Has schizophrenia ever disappeared?
Like many of the mental issues we treat, schizophrenia never truly goes away in the sense that we have a cure for it. The good news is that individuals diagnosed as schizophrenic have gone on to live successful, productive lives after seeking treatment.
What are 3 interesting facts about schizophrenia?
9 Facts About Schizophrenia You Should KnowSchizophrenia does not involve split personalities. ... Despite what you may have heard, people with schizophrenia are not inherently violent or dangerous. ... Symptoms of schizophrenia usually emerge in adolescence. ... Schizophrenia manifests both “positive” and “negative” symptoms.More items...•
What is still unknown about schizophrenia?
The exact causes of schizophrenia are unknown. Research suggests a combination of physical, genetic, psychological and environmental factors can make a person more likely to develop the condition. Some people may be prone to schizophrenia, and a stressful or emotional life event might trigger a psychotic episode.
Why did they treat schizophrenia with insulin?
According to the medical staff at the Bronx Veteran's Administration Hospital, writing about their treatment regime in 1960, insulin coma therapy was thought to relieve symptoms including “anxiety, tension, fear, irritability, hostility, elation, paranoid projections, obsessive and compulsive thinking, delusions, and ...
Why is schizophrenia called split mind?
Schizophrenia does mean “split mind,” but the name was meant to describe the 'split' from reality that you experience during an episode of psychosis, as well as changes in thoughts, emotions, and other functions.
What is schizophrenia best known for?
Schizophrenia is a mental health disorder in which a person has an abnormal interpretation of reality. Common symptoms of schizophrenia include hallucinations, delusions, and extremely disordered thinking and behavior.
Who was the first person to treat mental illness?
In the 5th century B.C., Hippocrates was a pioneer in treating mentally ill people with techniques not rooted in religion or superstition; instead, he focused on changing a mentally ill patient's environment or occupation, or administering certain substances as medications.
Who was the first person to discover mental illness?
While diagnoses were recognized as far back as the Greeks, it was not until 1883 that German psychiatrist Emil Kräpelin (1856–1926) published a comprehensive system of psychological disorders that centered around a pattern of symptoms (i.e., syndrome) suggestive of an underlying physiological cause.
When was schizophrenia first discovered?
Kraepelin first carved out schizophrenia from other forms of psychosis in 1887, but that is not to say that schizophrenia— or dementia præcox, as he called it—had not existed long before his day. The oldest available description of an illness closely resembling schizophrenia can be found in the Ebers papyrus, which dates back to the Egypt of 1550 BCE. And archæological finds of Stone Age skulls with burr holes—drilled, presumably, to release evil spirits—have led to speculation that schizophrenia is as old as humankind.
When did Kraepelin first diagnose schizophrenia?
article continues after advertisement. Kraepelin first carved out schizophrenia from other forms of psychosis in 1887, but that is not to say that schizophrenia— or dementia præcox, as he called it—had not existed long before his day.
What is fever therapy?
Febrile illnesses such as malaria had been observed to temper psychotic symptoms, and in the early 20th century, ‘fever therapy ’ became a common form of treatment for schizophrenia. Psychiatrists attempted to induce fevers in their patients, sometimes by means of injections of sulphur or oil.
What does "schizophrenia" not mean?
What does ‘schizophrenia’ not mean? Robert Louis Stevenson’s novel The Strange Case of Dr Jekyll and Mr Hyde (1886) did much to popularize the concept of a ‘split personality’, which is sometimes also referred to as ‘ multiple personality disorder ’ (MPD). However, MPD is a vanishingly rare condition that is entirely unrelated to schizophrenia.
Can schizophrenia mutate?
Unlike Dr Jekyll, schizophrenia sufferers do not suddenly mutate into a different, un recognizable person. Ironically, Bleuler had intended to clarify matters by replacing the older, even more misleading term of dementia præcox [‘dementia of early life’].
When did the burning of heretics begin?
The burning of the so-called heretics—often people suffering from psychotic illnesses such as schizophrenia—began in the early Renaissance and reached its peak in the 14th and 15th centuries. First published in 1563, De præstigiis dæmonum[The Deceptionof Demons] argued that the madness of ‘heretics’ resulted not from divine punishment or demonic possession, but from natural causes. The Church proscribed the book and accused its author, Johann Weyer, of being a sorcerer.
Who was the first person to distinguish schizophrenia from other forms of psychosis?
Despite his shortcomings, Kraepelin was the first to distinguish schizophrenia from other forms of psychosis, and in particular from the ‘affective psychoses’ that can supervene in mood disorders such as depression and bipolar disorder.
What were the asylums in Victorian times?
The enlightened leaders of the Victorian age on both sides of the Atlantic built large institutional asylums into which people with schizophrenia were confined often for many years and sometimes for life. Although some of these asylums were later exposed as abusive, at the time they were built, they were seen as a compassionate alternative to confining lunatics in prison or to life on the streets where they were prey to those criminals who would seek to exploit them.
What was the 3rd Reich?
The Third Reich represents one of the most significant challenges for schizophrenia sufferers in the history of the condition not simply because thousands of people with schizophrenia died as a result but also because this tragic episode in modern European history points up the constant threat that people living with schizophrenia face from the followers of eugenics.
How did schizophrenia work in Germany?
Initially this was carried out by means of lethal injection but later gas chambers were introduced as a more efficient method.
Where did the Victorian asylums in Dartmoor provide asylums for schizophrenia?
The old Victorian asylums like this one at Moorhaven on the edge of Dartmoor provided many people with schizophrenia with a sanctuary from the pressures of the world. (Image: Guy Wareham)
When was schizophrenia first described?
In fact the oldest recorded description of an illness like schizophrenia dates back to the Ebers Papyrus of 1550BC from Egypt. 1. Descriptions of episodes of madness involving hearing voices, seeing visions and erratic and unruly behaviour start to appear in the literature from the 17th century.
Where in the Bible does it talk about schizophrenia?
Schizophrenia has been around for a long time. References to people who are clearly insane appear in classical writings and the bible, for instance in Mark 5 we hear of the Gerasene Demoniac who, “All day and all night among the tombs and in the mountains he would howl and gash himself with stones”. In fact the oldest recorded description of an illness like schizophrenia dates back to the Ebers Papyrus of 1550BC from Egypt. 1
What was the Nazi plan to eradicate schizophrenia?
Faced with the seemingly intractable problem of an incurable condition that led to disturbed behaviour, in the 1930s the Nazi regime in Germany embarked on an ambitious programme to eradicate schizophrenia from the race by the use of euthanasia.
What is schizophrenia characterized by?
Schizophrenia is a psychotic disorder characterized by hallucinations, delusions, and disturbances in thought, perception, and behavior. Traditionally, schizophrenia may involve positive symptoms, such as hallucinations, delusions, formal thought disorders, and negative symptoms, such as paucity of speech, anhedonia, and lack of motivation. This activity outlines the evaluation of schizophrenia and explains the role of the interprofessional team in improving care for patients with this condition.
What is the best treatment for psychosis?
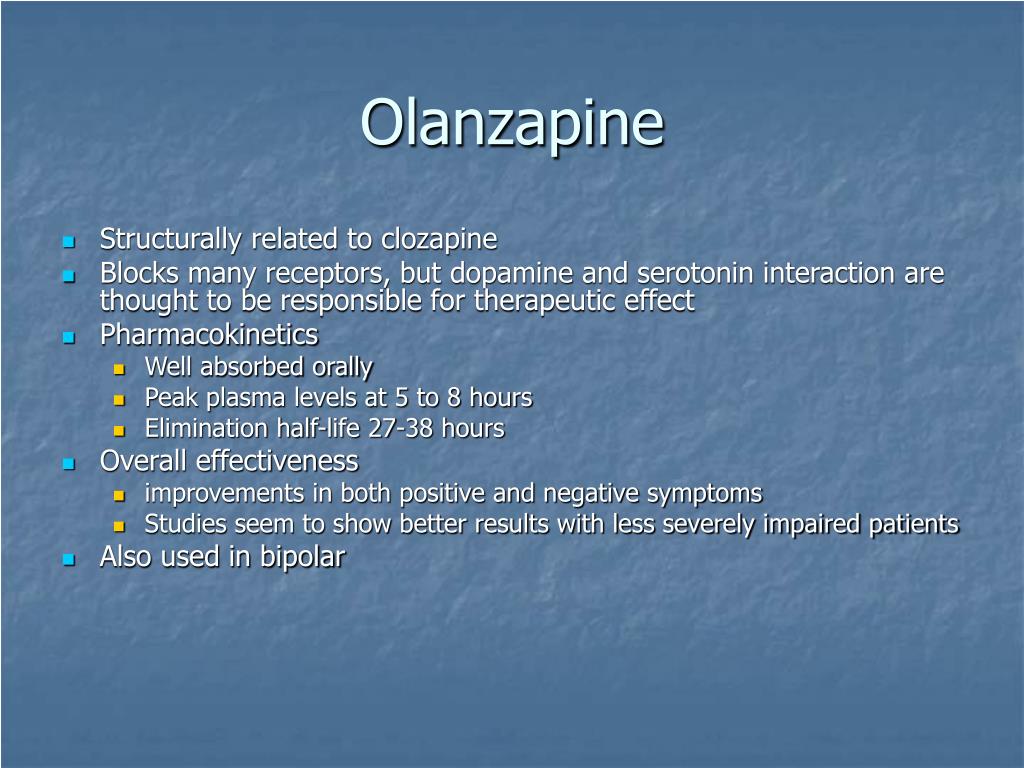
For the initial treatment of acute psychosis, it is recommended to start an oral second-generation antipsychotic (SGA) such as aripiprazole, olanzapine, risperidone, quetiapine, asenapine, lurasidone, sertindole, ziprasidone, brexpiprazole, molindone, iloperidone, etc. Sometimes, if clinically needed, alongside a benzodiazepine such as diazepam, clonazepam, or lorazepam to control behavioral disturbances and non-acute anxiety. First-generation antipsychotics (FGA) like trifluoperazine, fluphenazine, haloperidol, pimozide, sulpiride, flupentixol, chlorpromazine, etc., are not commonly used as the first line but can be used.
What are the main hypotheses for schizophrenia?
There are three main hypotheses regarding the development of schizophrenia. The neurochemical abnormality hypothesis argues that an imbalance of dopamine, serotonin, glutamate, and GABA results in the psychiatric manifestations of the disease. It postulates that four main dopaminergic pathways are involved in the development of schizophrenia. This dopamine hypothesis attributes the positive symptoms of the illness to excessive activation of D2 receptors via the mesolimbic pathway, while low levels of dopamine in the nigrostriatal pathway are theorized to cause motor symptoms through their effect on the extrapyramidal system. Low mesocortical dopamine levels resulting from the mesocortical pathway are thought to elicit the negative symptoms of the disease. Other symptoms such as amenorrhea and decreased libido may be caused by elevated prolactin levels due to decreased availability of tuberoinfundibular dopamine as a result of blockage of the tuberoinfundibular pathway. Evidence showing exacerbation of positive and negative symptoms in schizophrenia by NMDA receptor antagonists insinuates the potential role of glutaminergic hypoactivity while serotonergic hyperactivity has also been shown to play a role in schizophrenia development. [5]
What is the genetic basis for schizophrenia?
Several studies postulate that the development of schizophrenia results from abnormalities in multiple neurotransmitters, such as dopaminergic, serotonergic, and alpha-adrenergic hyperactivity or glutaminergic and GABA hypoactivity. Genetics also plays a fundamental role - there is a 46% concordance rate in monozygotic twins and a 40% risk of developing schizophrenia if both parents are affected. The gene neuregulin (NGR1), which is involved in glutamate signaling and brain development, has been implicated, alongside dysbindin (DTNBP1), which helps glutamate release, and catecholamine O-methyl transferase (COMT) polymorphism, which regulates dopamine function.
How much does urban residence increase the risk of developing schizophrenia?
Urban residence - increases the risk of developing schizophrenia by 2 to 4%
What is hallucinatory voice?
Hallucinatory voices providing a running commentary of the patient
What is disconnect hypothesis?
Conversely, the disconnect hypothesis focuses on the neuroanatomical changes seen in PET and fMRI scans. There is a reduction in grey matter volume in schizophrenia, present not only in the temporal lobe but in the parietal lobes as well. Differences in the frontal lobes and hippocampus are also seen, potentially contributing to a range of cognitive and memory impairments associated with the disease.
What did Kraepelin mean by early dementia?
By calling his syndrome 'early dementia', he meant to differentiate it from dementias that occur later in life such as Alzheimer's disease (senility). Correctly, Kraepelin believed that dementia praecox was primarily a disease of the brain. However, he was mistaken in believing that this disorder was a form of dementia.
What is schizophrenia caused by?
Conditions like schizophrenia were not differentiated from other forms of mental illness or mental retardation, much of which was thought of as being supernatural in origin, caused by evil spirits, demon possession, punishment for sin, or similar spiritualist phenomena.
What was Gregory Bateson's theory of schizophrenia?
This theory proposed that schizophrenia was caused by particular forms of bad parenting, specifically where parents explicitly said one thing and then contradicted that thing with implicit unconscious messages of opposite content.
What is Kurt Schneider's contribution to schizophrenia?
The next major contribution to the progress of understanding schizophrenia came when Kurt Schneider listed his 'first rank' features of the disease in 1959. This important work effectively differentiated schizophrenia from other psychoses and served as the inspiration for the two diagnostic manuals widely used to define modern schizophrenia, the International Classification of Diseases (ICD, currently in its 10th edition) and the DSM. The definition and diagnostic criteria for schizophrenia codified in these manuals continue to evolve today, based primarily on new research findings that further illuminate the illness.
Who was the first to describe schizophrenia as a negative or positive?
Although Bleuler was the first to describe symptoms as "positive" or "negative", both Kraepelin and Bleuler recognized that schizophrenia symptoms tended to cluster into distinct categories. They created a typology of schizophrenic subtypes that continues to be used today. Modern schizophrenic categories recognized by the DSM (Diagnostic and Statistical Manual of Mental Disorders; the repository of mental health diagnoses, currently in its fourth, text-revised edition) include paranoid, disorganized, catatonic, residual, and undifferentiated subtypes, each based on a particular distinct symptom cluster.
When was schizophrenia first described?
The first, formal description of schizophrenia as a mental illness was made in 1887 by Dr. Emile Kraepelin.
Does schizophrenia have a diathesis?
A diathesis is a vulnerability. Diathesis-stress models of schizophrenia basically propose that people have predispositions and vulnerabilities ...
What are the side effects of schizophrenia?
Schizophrenia medications can cause a variety of other adverse effects, including the following: 1 Antipsychotic medications with anticholinergic effects have been shown to worsen narrow-angle glaucoma, and patients should be appropriately monitored.49Chlorpromazine is most commonly associated with opaque deposits in the cornea and lens.2Because of the risk of cataracts, eye examinations are recommended for patients treated with quetiapine.50Those using thioridazine at doses exceeding 800 mg daily are at risk of developing retinitis pigmentosa.2 2 Low-potency FGAs and clozapine have been associated with urinary hesitancy and retention.2The incidence of urinary incontinence among patients taking clozapine can be as high as 44% and can be persistent in 25% of patients.2,51 3 FGAs and risperidone have a greater tendency to cause sexual dysfunction compared with SGAs.2,52 4 Treatment with antipsychotics can cause transient leukopenia.2,53 5 The three antipsychotics with the greatest risk for hematological complications are clozapine, chlorpromazine, and olanzapine.54Clozapine is associated with an especially high risk for the development of neutropenia or agranulocytosis.54 6 On rare occasions, dermatological allergic reactions have occurred at approximately eight weeks after the initiation of antipsychotic therapy.2 7 Both FGAs and SGAS can cause photosensitivity, leading to severe sunburn.2 8 Clozapine has been reported to cause sialorrhea in approximately 54% of patients with schizophrenia.2The mechanism of this effect is unknown.2
How many nonadherence rates are there in schizophrenia?
Not only do nonpharmacological therapies fill in gaps in pharmacological treatments; they can help to ensure that patients remain adherent to their medications.18Nonadherence rates in schizophrenia range from 37% to 74%, depending on the report.19Individuals with mental disorders tend to be less adherent for several reasons. They may deny their illness; they may experience adverse effects that dissuade them from taking more medication; they may not perceive their need for medication; or they may have grandiose symptoms or paranoia.2
What are the factors that contribute to schizophrenia?
Environmental and social factors may also play a role in the development of schizophrenia, especially in individuals who are vulnerable to the disorder.1Environmental stressors linked to schizophrenia include childhood trauma, minority ethnicity, residence in an urban area, and social isolation.1In addition, social stressors, such as discrimination or economic adversity, may predispose individuals toward delusional or paranoid thinking.1
What neurotransmitter is involved in schizophrenia?
Another theory for the symptoms of schizophrenia involves the activity of glutamate, the major excitatory neurotransmitter in the brain. This theory arose in response to the finding that phenylciclidine and ketamine, two noncompetitive NMDA/glutamate antagonists, induce schizophrenia-like symptoms.6This, in turn, suggested that NMDA receptors are inactive in the normal regulation of mesocortical dopamine neurons, and pointed to a possible explanation for why patients with schizophrenia exhibit negative, affective, and cognitive symptoms.7
What is the serotonin hypothesis?
The serotonin hypothesis for the development of schizophrenia emerged as a result of the discovery that lysergic acid diethylamide (LSD) enhanced the effects of serotonin in the brain. 1Subsequent research led to the development of drug compounds that blocked both dopamine and serotonin receptors, in contrast to older medications, which affected only dopamine receptors. The newer compounds were found to be effective in alleviating both the positive and negative symptoms of schizophrenia.1
How to diagnose schizophrenia?
A diagnosis of schizophrenia is reached through an assessment of patient-specific signs and symptoms, as described in the Diagnostic and Statistical Manual of Mental Disorders,Fifth Edition (DSM-5).12The DSM-5states that “the diagnostic criteria [for schizophrenia] include the persistence of two or more of the following active-phase symptoms, each lasting for a significant portion of at least a one-month period: delusions, hallucinations, disorganized speech, grossly disorganized or catatonic behavior, and negative symptoms.”12At least one of the qualifying symptoms must be delusions, hallucinations, or disorganized speech.12
How many patients report favorable treatment outcomes for schizophrenia?
The prognosis for patients with schizophrenia is generally unpredictable.2Only 20% of patients report favorable treatment outcomes.12The remaining patients experience numerous psychotic episodes, chronic symptoms, and a poor response to antipsychotics.2