
Where will you find keratinocytes?
Keratinocytes are found in the outermost layer of the skin, called the epidermis. The epidermis is composed of 95% keratinocyte cells. The cells in the basal layer are sometimes called basal keratinocytes or basal cells.
Where are keratinized cells found in the body?
Keratinocyte cells are found in the deepest basal layer of the stratified epithelium that comprises the epidermis, and are sometimes referred to as basal cells or basal keratinocytes. It is known that 95% of the cells in the epidermis are keratinocytes. Squamous keratinocytes are also found in the mucosa of the mouth and esophagus, as well as the corneal, conjunctival and genital …
Where is cytoskeleton found in a house?
The last two types are found only occasionally in the epidermis and oral mucosa. The dendritic cells are of the same type as in the dermis and will be described later (see Dermal cells). Keratinocytes. Keratinocytes represent the most frequently found principal cells of the epidermis. From the lowermost basal layer to the uppermost shedding cells of stratum corneum they …
Where are heterocysts found?
Keratinocytes are the most prominent cell within the epidermis. Keratinocytes are ectodermally derived and can be distinguished from melanocytes and Langerhans cells in the epidermis by their larger size, intercellular bridges, and ample cytoplasm. Keratinocytes are present in all four layers of the epidermis.

Are keratinocytes found in the dermis or epidermis?
What layer of skin is keratinocytes found?
What is keratinocytes and its function?
Keratinocytes are maintained at various stages of differentiation in the epidermis and are responsible for forming tight junctions with the nerves of the skin. They also keep Langerhans cells of the epidermis and lymphocytes of the dermis in place.
Where are the oldest keratinocytes in your skin found?
Where are the youngest keratinocytes found?
What do keratinocytes produce?
What substance does keratinocytes produce?
What is the role of keratinocytes in wound healing?
Where are keratinocytes found?
It is known that 95% of the cells in the epidermis are keratinocytes. Squamous keratinocytes are also found in the mucosa of the mouth and esophagus , as well as the corneal, conjunctival and genital epithelia.
What are keratinocytes?
Keratinocytes are maintained at various stages of differentiation in the epidermis and are responsible for forming tight junctions with the nerves of the skin. They also keep Langerhans cells of the epidermis and lymphocytes of the dermis in place.
What is the role of keratinocytes in the immune system?
In addition to their physical role, keratinocytes serve a chemical immune role as immunomodulators, responsible for secreting inhibitory cytokines in the absence of injury and stimulating inflammation and activating Langerhans cells in response to injury.
What is the first line of defense for an organism?
The skin is the first line of defense and keratinocytes serve as a barrier between an organism and its environment. In addition to preventing toxins and pathogens from entering an organisms body, they prevent the loss of moisture, heat and other important constituents of the body.
How long does it take for keratinocytes to migrate?
Epidermal keratinocytes initially respond to an epidermal defect by migrating from the free edges of the wound within 24 hours. The keratinocyte migration in partial-thickness wounds also occurs from remaining skin appendages, including the hair follicle (Fig. 7.4 ). Epidermal stem cells from the hair follicle are now thought to originate from the hair bulge, which is believed to be the germinative portion of the hair. 18 A change in the activity of keratinocytes is required for re-epithelialization to occur. In the unwounded stable state, cuboid-shaped basal keratinocytes interact with each other by a desmosomal intercellular bridge, and are connected to their own basement membrane zone by hemidesmosomes. Approximately 12 hours after wounding, epidermal cells become somewhat flattened and elongated, develop pseudopod-like projections named lamellipodia, lose their cell–cell and cell–matrix attachments, retract their intracellular tonofilaments, and form actin filaments at the edge of the cell cytoplasm. While epidermal cells are migrating, their proliferative potential is inhibited. The migrating basal cells are thought to differ from normal basal cells and may express selective cell surface markers such as CD44, as well as some markers usually expressed by squamous cells. 18
What is the pigment produced by melanocytes?
The pigment produced by the melanocytes is synthesised in a complex organelle called melanosome. Chemically, there are two basic types of melanin – namely eumelanin, which is brown-black and insoluble, and phenomelanin, which is yellow-red and soluble in dilute alkali. Produced melanin granules move from melanocytes to other cells where they assume a static array. In keratinocytes they form a supranuclear cap that acts as a shield against UV radiation. It has been shown that sun exposure stimulates the melanocytes to produce larger melanosomes making the distribution of these proteins resembling the pattern found in dark-skinned individuals.
What are the different types of cells in the epidermis?
There are at least five cell types in the adult epidermis: keratinocytes, Langerhans cells, melanocytes, Merkel cells and dendritic cells. The last two types are found only occasionally in the epidermis and oral mucosa. The dendritic cells are of the same type as in the dermis and will be described later (see Dermal cells).
Where are Merkel cells found?
They are mostly found in special regions such as the lips, oral cavity, hair follicles, the glabrous skin of the digits, or as a part of certain tactile discs. They are attached to adjacent keratinocytes by desmosomes (Figure 3 ). There are two prevailing hypotheses regarding the origin of the Merkel cells: the neural crest and cutaneous origin hypotheses. The tactile Merkel cells are opposed to small nerve plates connected by short, nonmyelinated axons to myelinated axons. These complex structures serve as tactile mechanoreceptors ( Figure 4 ). Epidermal Merkel cells seem to stimulate local proliferation and differentiation of keratinocytes.
Which enzyme is responsible for synthesis of pregnenolone?
Keratinocytes and sebocytes express not only StAR protein and CYP11A1 to promote pregnenolone synthesis, but also CYP17A1 (P450c17), which encodes the enzyme responsible for catalyzing 17-hydroxylation of pregnenolone and then a subsequent lyase reaction between C17 and C20 resulting in dehydroepiandrosterone (DHEA) (Thiboutot et al., 2003 ). Hair follicles also can potentially contribute to the local production of DHEA, as their steroid sulfatase activity can produce DHEA from circulating DHEA-sulfate, a product of systemic adrenal gland production ( Hoffmann et al., 2001 ). DHEA is then further converted to androstenedione in sebaceous glands by the type 1 isoform of 3β-hydroxysteroid dehydrogenase/Δ 5−4 isomerase (3β-HSD1) ( Fritsch et al., 2001; Chen et al., 2010 ).
Where is PTHRP expressed?
PTHrP is expressed in the basal layer through the granulosa layer of the skin, with epidermal expression detectable as early as day 14 of embryogenesis in the rat [183,184], although PTHrP expression in the epidermis may be limited to the hair follicles [185].
Where are keratinocytes found?
Keratinocytes (stained green) in the skin of a mouse. Keratinocytes are the primary type of cell found in the epidermis, the outermost layer of the skin. In humans, they constitute 90% of epidermal skin cells. Basal cells in the basal layer ( stratum basale) of the skin are sometimes referred to as basal keratinocytes.
What are keratinocytes associated with?
Within the epidermis keratinocytes are associated with other cell types such as melanocytes and Langerhans cells. Keratinocytes form tight junctions with the nerves of the skin and hold the Langerhans cells and intra-dermal lymphocytes in position within the epidermis. Keratinocytes also modulate the immune system: apart from the above-mentioned antimicrobial peptides and chemokines they are also potent producers of anti-inflammatory mediators such as IL-10 and TGF-β. When activated, they can stimulate cutaneous inflammation and Langerhans cell activation via TNFα and IL-1β secretion.
What are basal cells?
In humans, they constitute 90% of epidermal skin cells. Basal cells in the basal layer ( stratum basale) of the skin are sometimes referred to as basal keratinocytes.
What are the functions of keratinocytes?
The primary function of keratinocytes is the formation of a barrier against environmental damage by heat, UV radiation, water loss, pathogenic bacteria, fungi, parasites, and viruses . Pathogens invading the upper layers of the epidermis can cause keratinocytes to produce proinflammatory mediators, particularly chemokines such as CXCL10 and CCL2 ...
What are the proteins that make up the skin barrier?
A number of structural proteins ( filaggrin, keratin ), enzymes ( proteases ), lipids, and antimicrobial peptides ( defensins) contribute to maintain the important barrier function of the skin. Keratinization is part of the physical barrier formation ( cornification ), in which the keratinocytes produce more and more keratin ...
What is the process of keratinization?
Keratinization is part of the physical barrier formation ( cornification ), in which the keratinocytes produce more and more keratin and undergo terminal differentiation. The fully cornified keratinocytes that form the outermost layer are constantly shed off and replaced by new cells.
Where do epidermal stem cells reside?
Epidermal stem cells reside in the lower part of the epidermis (stratum basale) and are attached to the basement membrane through hemidesmosomes. Epidermal stem cells divide in a random manner yielding either more stem cells or transit amplifying cells.
What are the three types of keratinocytes?
There are three types of keratonocyte clones-holoclone, meroclone, and paraclone ( Figure 7.4) [45]. Holoclone can give rise to meroclone and paraclone but reverse does not happen.
What are the factors that contribute to the development of keratinocyte carcinoma?
Agents playing a significant role in the pathogenesis of keratinocyte carcinoma include ultraviolet light, x-ray exposure, and chemical carcinogens. Fair skin, immunosuppression, and human papillomavirus are associated with increased risk of keratinocyte carcinoma.
What is KC skin cancer?
Keratinocyte carcinoma (KC) (also referred to as nonmelanoma skin cancer (NMSC)) is by far the most common form of human cancer. A personal history of KC is well established to be associated with increased risk of recurrent KC (American Cancer Society, 2007 ). Based on shared risk factors and susceptibility profiles it is not surprising ...
Is KC a cancer?
Keratinocyte carcinoma (KC) (also referred to as nonmelanoma skin cancer (NMSC)) is by far the most common form of human cancer. A personal history of KC is well established to be associated with increased risk of recurrent KC (American Cancer Society, 2007 ). Based on shared risk factors and susceptibility profiles it is not surprising that a personal history of KC is also associated with a markedly increased risk of malignant melanoma, another form of cutaneous carcinoma that is far more lethal but less common than KC. More surprising is that a substantial body of epidemiologic evidence now indicates that a personal history of KC is consistently associated with an overall elevated risk of noncutaneous malignancies. In the later sections, after providing background on the occurrence of KC in populations and factors associated with KC risk, this evidence is characterized and evaluated. Evidence is also summarized from studies that have examined KC in relation to increased risk of fatal outcomes such as survival after a diagnosis with a noncutaneous malignancy, cancer-specific mortality, and all-cause mortality.
What are TA cells?
TA cells differentiate and give rise to spinous, granular and stratum corneum layers. After several rounds of cell divisions, these TA cells may become senescent TA cells, which may not differentiate into cells of spinous, granular and stratum corneum layers.
What is the youngest layer of the epidermis?
The youngest keratinocyte layer of the epidermis is separated from the underlying dermis by the basement membrane. The basement membrane is composed of collagen and other molecules produced by epidermal keratinocytes in combination with fibronectin produced by dermal fibroblasts. Because there are no blood vessels in the epidermis, the nutrients required to sustain the keratinocytes must exit the circulation in the dermal blood vessels and diffuse across the basement membrane. Leukocytes that access the epidermis, including the T cell and LC populations, also extravasate from the dermal blood vessels. These migrating cells secrete enzymes that dissolve small regions of the basement membrane, allowing passage of the leukocytes into the epidermis.
What is the basement membrane of the epidermis?
The basement membrane is a protective layer composed of collagen, laminin, heparan sulfate, and glycosaminoglycan produced by epidermal keratinocytes in combination with fibronectin produced by dermal fibroblasts. As mentioned previously, there are no blood vessels in the epidermis. Thus, nutrients required to sustain the keratinocytes must exit the circulation in the dermal blood vessels and diffuse across the basement membrane. Similarly, leukocytes that access the epidermis, including the T cell and DC populations, must migrate from the dermal vessels and force their way through the basement membrane before entering the epidermis. Activated leukocytes secrete enzymes that dissolve components of the basement membrane, allowing rapid passage of the migrating cells into the epidermis.
Where do keratinocytes form?
Keratinocytes form in the deep, basal cell layer of the skin and gradually migrate upward, becoming squamous cells before reaching the surface of the skin over the course of a month. For this reason, non-melanoma skin cancers such as basal cell carcinoma and squamous cell carcinoma are sometimes called keratinocyte cancers.
What type of cell is keratinocyte?
When to See a Doctor. Keratinocytes are the most common type of skin cells. They make keratin, a protein that provides strength to skin, hair, and nails. Keratinocytes form in the deep, basal cell layer of the skin and gradually migrate upward, becoming squamous cells before reaching the surface of the skin over the course of a month. ...
How do you know if you have basal cell cancer?
Although a general warning sign of skin cancer is a sore that won't heal or that repeatedly bleeds and scabs over, basal cell cancer may also appear as: 3 1 A pearly white or waxy bump, often with visible blood vessels, on your face, ears or neck. The bump may bleed and develop a crust. In darker skinned people, this type of cancer may be brown or black. 2 A flat, scaly, brown or flesh-colored patch on your back or chest. Over time, these patches can grow quite large. 3 More rarely, a white, waxy scar. This type of basal cell carcinoma is easy to overlook, but it may be a sign of a particularly invasive and disfiguring cancer called morpheaform basal cell carcinoma.
What is the most common type of skin cell?
Keratinocytes are the most common type of skin cells. They make keratin, a protein that provides strength to skin, hair, and nails. Keratinocytes form in the deep, basal cell layer of the skin and gradually migrate upward, becoming squamous cells before reaching the surface of the skin over the course of a month.
What is the protein that makes up the skin?
They make keratin, a protein that provides strength to skin, hair, and nails. Keratinocytes form in the deep, basal cell layer of the skin and gradually migrate upward, becoming squamous cells before reaching the surface of the skin over the course of a month.
What is basal cell carcinoma?
Basal cell carcinoma is a type of skin cancer. Basal cell carcinoma begins in the basal cells—a type of cell within the skin that produces new skin cells as old ones die off. Most basal cell carcinomas are thought to be caused by long-term exposure to ultraviolet (UV) radiation from sunlight. Avoiding the sun and using sunscreen may help protect ...
Where are basal cells located?
Basal cells are found at the bottom of the epidermis—the outermost layer of skin. Basal cells produce new skin cells. As new skin cells are produced, they push older cells toward the skin's surface, where the old cells die and are sloughed off. The process of creating new skin cells is controlled by a basal cell's DNA.
Where are keratinocytes found?
Keratinocytes are found in the outermost layer of the skin, called the epidermis. The epidermis is composed of 95% keratinocyte cells. The cells in the basal layer are sometimes called basal keratinocytes or basal cells. The epidermis is about 0.2 mm thick. Inside the epidermis, keratinocytes are arranged in four different layers — ...
What is the function of keratinocytes?
The key function of keratinocytes is to develop a barricade against environmental changes such as UV radiation, heat, pathogens (fungi, viruses, bacteria, parasites), and water loss and also play a significant role in signal transduction inside the extracellular matrix. YouTube. Subscribe. Watch later.
What are the different types of melanins?
Melanins are classified as: 1 Eumelanin—that gives the black or brown color to skin and hair of humans; 2 Pheomelanin—that gives yellow to reddish brown color, majorly found in the female skin; 3 Neuromelanin—that produces brown or black color in a specific region of the brain; 4 and both pheomelanin and eumelanin.
Where are basal cells found?
Basal cells. Basal cells are small round-shaped cells found in the basal cell layer. Skin cells are first produced in this region by continuous division, giving rise to new skin cells. These new cells continuously force the older cells toward the uppermost layer of the skin, where they are finally shed. The basal layer is otherwise called the ...
How are skin cells produced?
Skin cells are first produced in this region by continuous division, giving rise to new skin cells . These new cells continuously force the older cells toward the uppermost layer of the skin, where they are finally shed. The basal layer is otherwise called the stratum germinativum, as the cells produce new cells continuously.
What is the basal layer of the skin?
The basal layer is otherwise called the stratum germinativum, as the cells produce new cells continuously. These cells are composed of basophilic cytoplasm and a chromatin-rich nucleus in an elliptical shape.
What are basal cells called?
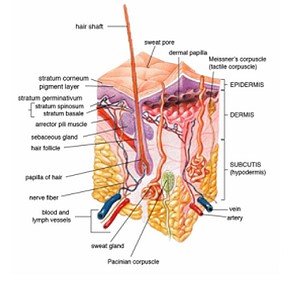
The cells in the basal layer are sometimes called basal keratinocytes or basal cells. The epidermis is about 0.2 mm thick. Inside the epidermis, keratinocytes are arranged in four different layers — the stratum basale, stratum spinosum, stratum granulosum, and stratum corneum. The stratum basale is the basal layer of the epidermis ...
Definition and Location
- Keratinocytes represent the major cell type of the epidermis, the outermost of the layers of the skin, making up about 90 percent of the cells there. They originate in the deepest layer of the epidermis, the stratum basale and move up to the final barrier layer of the skin, the stratum corneum. There, keratinocytes are found as nucleus-free, flat, ...
Differentiation of Keratinocytes
- Keratinocytes proliferate in the basal layer of the epidermis and start differentiating on their way to the surface, undergoing gradual differentiation. During this process, they profoundly change their morphology and start to produce keratin, cytokines, growth factors, interleukins and complement factors. Keratinocyte differentiation is regulated by several factors as well as by ep…
Function
- Keratinocytes are highly specialized. They play an essential role in protection, as they form a tight barrier that prevents foreign substances from entering the body, while minimizing the loss of moisture, heat, and other constituents. These cells have also a structural role, forming tight bonds with the other cells in the epidermis and maintaining them in their locations. In addition, keratino…
Applications
- Keratinocyte Cell Culture Cultivation of human keratinocytes in monolayer culture was first described by Rheinwald and Green more than 30 years ago. Since then, numerous advances have been made in...
- Characterization At each stage of differentiation, keratinocytes express specific keratins, but also other markers such as involucrin, loricrin, transglutaminase, filaggrin, and caspase 14.
- Keratinocyte Cell Culture Cultivation of human keratinocytes in monolayer culture was first described by Rheinwald and Green more than 30 years ago. Since then, numerous advances have been made in...
- Characterization At each stage of differentiation, keratinocytes express specific keratins, but also other markers such as involucrin, loricrin, transglutaminase, filaggrin, and caspase 14.
- Research Applications Keratinocytes can be used in many applications, such as studies on epidermal development and differentiation, studies on drug uptake, pharmaceutical testing, cosmetic and toxi...
Interactions with Other Cells in The Skin
- Keratinocytes and Fibroblasts The cross-talk between keratinocytes and fibroblasts is essential for maintaining the skin homeostasis and for ensuring a balanced wound-healing process (Wojtowicz, 20...
- Keratinocytes and Melanocytes The interaction of keratinocytes and melanocytes is also crucial for the homeostasis of the epidermis. Melanocytes produce melanin, which absorbs …
- Keratinocytes and Fibroblasts The cross-talk between keratinocytes and fibroblasts is essential for maintaining the skin homeostasis and for ensuring a balanced wound-healing process (Wojtowicz, 20...
- Keratinocytes and Melanocytes The interaction of keratinocytes and melanocytes is also crucial for the homeostasis of the epidermis. Melanocytes produce melanin, which absorbs UV waves and prevents...
- Keratinocytes and other cells Keratinocytes have immunomodulatory functions that interact with lymphocytes and Langerhans cells in the skin.
Role in Wound Healing and Inflammation
- Keratinocytes in Wound Healing Keratinocytes are responsible for restoring the epidermis following injuries (Pastar et al., 2014). This process, called re-epithelialization, is necessary for a succ...
- Keratinocytes in Inflammation When the epidermal barrier is breached or when pathogens enter the skin, an inflammatory response is triggered. Keratinocytes actively participate in thi…
- Keratinocytes in Wound Healing Keratinocytes are responsible for restoring the epidermis following injuries (Pastar et al., 2014). This process, called re-epithelialization, is necessary for a succ...
- Keratinocytes in Inflammation When the epidermal barrier is breached or when pathogens enter the skin, an inflammatory response is triggered. Keratinocytes actively participate in this process, as...
Keratinocytes by Promocell
- The in vitroculture of human skin cells is an essential research tool widely used for assaying dermal toxicity, pharmacological testing, and tissue repair. We offer a comprehensive portfolio of primary human dermal cells including keratinocytes, melanocytes, fibroblasts and hair follicle cells to support these research applications. Primary Normal Human Epidermal Keratinocytes ar…
Overview
Keratinocytes are the primary type of cell found in the epidermis, the outermost layer of the skin. In humans, they constitute 90% of epidermal skin cells. Basal cells in the basal layer (stratum basale) of the skin are sometimes referred to as basal keratinocytes. Keratinocytes form a barrier against environmental damage by heat, UV radiation, water loss, pathogenic bacteria, fungi, parasites, and viruses. A number of structural proteins, enzymes, lipids, and antimicrobial peptidescontribute to …
Cell differentiation
Epidermal stem cells reside in the lower part of the epidermis (stratum basale) and are attached to the basement membrane through hemidesmosomes. Epidermal stem cells divide in a random manner yielding either more stem cells or transit amplifying cells. Some of the transit amplifying cells continue to proliferate then commit to differentiate and migrate towards the surface of the epidermis. Those stem cellsand their differentiated progeny are organized into columns named …
Function
The primary function of keratinocytes is the formation of a barrier against environmental damage by heat, UV radiation, water loss, pathogenic bacteria, fungi, parasites, and viruses.
Pathogens invading the upper layers of the epidermis can cause keratinocytes to produce proinflammatory mediators, particularly chemokines such as CXCL10 and CCL2 (MCP-1) which attract monocytes, natural killer cells, T-lymphocytes, and dendritic cellsto the site of pathogen inv…
Structure
A number of structural proteins (filaggrin, keratin), enzymes (proteases), lipids, and antimicrobial peptides (defensins) contribute to maintain the important barrier function of the skin. Keratinization is part of the physical barrier formation (cornification), in which the keratinocytes produce more and more keratin and undergo terminal differentiation. The fully cornified keratinocytes that form the outermost layer are constantly shed off and replaced by new cells.
Interaction with other cells
Within the epidermis keratinocytes are associated with other cell types such as melanocytes and Langerhans cells. Keratinocytes form tight junctions with the nerves of the skin and hold the Langerhans cells and intra-dermal lymphocytes in position within the epidermis. Keratinocytes also modulate the immune system: apart from the above-mentioned antimicrobial peptides and chemokines they are also potent producers of anti-inflammatory mediators such as IL-10 and TGF-β. …
Role in wound healing
Wounds to the skin will be repaired in part by the migration of keratinocytes to fill in the gap created by the wound. The first set of keratinocytes to participate in that repair come from the bulge region of the hair follicle and will only survive transiently. Within the healed epidermis they will be replaced by keratinocytes originating from the epidermis.
At the opposite, epidermal keratinocytes, can contribute to de novo hair follicle formation during …
Sunburn cells
A sunburn cell is a keratinocyte with a pyknotic nucleus and eosinophilic cytoplasm that appears after exposure to UVC or UVB radiation or UVA in the presence of psoralens. It shows premature and abnormal keratinization, and has been described as an example of apoptosis.
Aging
With age, tissue homeostasis declines partly because stem/progenitor cells fail to self-renew or differentiate. DNA damage caused by exposure of stem/progenitor cells to reactive oxygen species (ROS) may play a key role in epidermal stem cell aging. Mitochondrial superoxide dismutase (SOD2) ordinarily protects against ROS. Loss of SOD2 in mouse epidermal cells was observed to cause cellular senescencethat irreversibly arrested proliferation in a fraction of keratinocytes. In older …