What are the 3 hepatic veins?
The hepatic veins are large intraparenchymal veins which drain the liver into the inferior vena cava. They are usually three in number, named the right hepatic vein (RHV), middle hepatic vein (MHV) and left hepatic vein (LHV).
What does the hepatic vein contain?
The hepatic veins carry oxygen-depleted blood from the liver to the inferior vena cava. They also transport blood that has been drained from the colon, pancreas, small intestine, and the stomach, and cleaned by the liver. These veins originate from the core vein of the liver lobule, but they do not have any valves.
What happens when the hepatic artery is blocked?
Hepatic vein obstruction prevents blood from flowing out of the liver and back to the heart. This blockage can cause liver damage. Obstruction of this vein can be caused by a tumor or growth pressing on the vessel, or by a clot in the vessel (hepatic vein thrombosis).
What drains into the hepatic veins?
The hepatic veins are three large vessels that drain the venous blood from the liver into the inferior vena cava. The main hepatic veins are the right, intermediate and left hepatic veins....Hepatic veins.Drains fromCentral veins of the liverDrains toInferior vena cavaDrainage areaLiver1 more row•May 11, 2020
What does hepatic portal vein carry?
A blood vessel that carries blood to the liver from the intestines, spleen, pancreas, and gallbladder. Also called portal vein.
Does the hepatic vein carry oxygenated blood?
The liver receives a blood supply from two sources. The first is the hepatic artery which delivers oxygenated blood from the general circulation. The second is the hepatic portal vein delivering deoxygenated blood from the small intestine containing nutrients.
What is unique about hepatic portal vein?
Unlike most veins, the portal vein does not drain into the heart. Rather, it is part of a portal venous system that delivers venous blood into another capillary system, the hepatic sinusoids of the liver.
What is the difference between hepatic vein and renal vein?
The hepatic and renal veins drain into the inferior vena cava. The upper group of hepatic veins consists of three veins which extend to the posterior face of the liver to join the inferior cava. The left renal vein passes anterior to the aorta just below the origin of the superior mesenteric artery.
Where is the right hepatic vein located?
The right hepatic vein is the longest of the hepatic veins, formed anteriorly near the inferior border of the liver. It runs in the coronal plane through the right portal fissure, between the right medial and right lateral sectors of the liver.
What is the hepatic vein?
Hepatic vein (Vena hepatica) The hepatic veins are three large vessels that drain the venous blood from the liver into the inferior vena cava. The main hepatic veins are the right, intermediate and left hepatic veins. In addition, several smaller and somewhat inconsistent caudate lobe veins contribute to the venous drainage of the liver.
How many segments are there in the liver?
The course of the hepatic veins provides additional anatomical landmarks to further divide the four sectors of the liver (left lateral, left medial, right lateral, right medial) into eight segments, numbered by Roman numerals I-VIII.
Why are hepatic veins important?
Aside from their main function to drain the liver, the hepatic veins are important anatomical and surgical landmarks since they define the sectors and segments of the liver. This article will discuss the anatomy and function of the hepatic veins.
Which lobe drains the segment I of the liver?
The veins of the caudate lobe are highly inconsistent, varying in number from one to five. When present, they drain the segment I of the liver that corresponds to the caudate lobe. The veins of the caudate lobe terminate by draining directly into the inferior vena cava.
Where does the left hepatic vein end?
The left hepatic vein terminates by draining into the inferior vena cava, most often via a common trunk that forms with the intermediate hepatic vein.
Where does the vein end?
The vein terminates by draining into the inferior vena cava near the upper border of the caudate lobe of the liver, just below the central tendon of the diaphragm.
Where do the hepatic veins drain from?
There are usually three upper hepatic veins draining from the left, middle, and right parts of the liver.
What are the veins in the liver?
The hepatic veins are the veins of the liver, two of which are shown in this diagram. The hepatic veins are the veins that drain de-oxygenated blood from the liver into the inferior vena cava. There are usually three upper hepatic veins draining from the left, middle, and right parts of the liver. These are larger than the group ...
Where do the veins in the liver come from?
The lower group of from six to twenty smaller hepatic veins come from the right lobe and the caudate lobe, are in contact with the hepatic tissue, and are valveless. All the veins empty into the inferior vena cava at the back of the liver.
Which veins drain from the right, middle, and left regions of the liver?
The hepatic veins are divided into an upper and a lower group. The upper three drain the central veins from the right, middle, and left regions of the liver and are larger than the lower group of veins.
Can hepatic veins be connected to portal veins?
The syndrome can be fulminant, acute, chronic, or asymptomatic. The hepatic veins may be connected with the portal veins in a TIPS procedure.
Where do hepatic veins carry blood?
The hepatic veins carry oxygen-depleted blood from the liver to the inferior vena cava. They also transport blood that has been drained from the colon, pancreas, small intestine, and the stomach, and cleaned by the liver. These veins originate from the core vein of the liver lobule, but they do not have any valves.
Where do the veins in the upper group originate?
The upper group usually consists of three large veins that originate from the backside of the liver and drain the right, middle, and left lobes of the liver.
What is the liver's role in the heart?
In that respect, the liver performs the role of a filtering organ for blood that is on its way back to the heart. Any impediment in the outflow of blood from the hepatic veins may result in a serious condition known as Budd-Chiari syndrome, which can cause liver damage. Last medically reviewed on January 20, 2018.
Where do the lobule veins come from?
These veins originate from the core vein of the liver lobule, but they do not have any valves. They can be segregated into the lower group and the upper group veins.
Where does oxygen depleted blood go?
The oxygen-depleted blood from these veins empty into the inferior vena cava. From here, the blood is delivered back to the heart, where the re-oxygenation process of the blood takes place. In that respect, the liver performs the role of a filtering organ for blood that is on its way back to the heart.
Where is the hepatic portal vein located?
Generally, the hepatic portal vein is about 8 centimeters (3 inches) long in adults, and is located in the upper right quadrant of the abdomen, which originates behind the neck of the pancreas and is part of the hepatic portal system.
What is the hepatic portal vein?
This vein is part of the hepatic portal system that receives all of the blood draining from the abdominal digestive tract, as well as from the pancreas, gallbladder, and spleen. ‘Hepatic’ means of or relating to the liver, therefore the hepatic portal vein is a blood vessel that sends nutrient-rich blood from the gastrointestinal tract ...
What is the confluence of the splenic and mesenteric veins?
While there may be some variations between individuals, the hepatic portal vein is usually formed by the convergence of the superior mesenteric vein and the splenic vein, referred to as the splenic-mesenteric confluence. In some individuals, the hepatic portal vein also directly joins with the inferior mesenteric vein.
What is the role of the hepatic portal system in the body?
Additionally, the hepatic portal system plays a key role in cleansing the blood of the bacteria and toxins that are picked up by the blood while it is being perfused through the intestines.
Which veins are responsible for lipid metabolism?
The left and right gastric veins, which form an arc along the lesser curvature of the stomach, also empty into the hepatic portal vein. Broadly, the hepatocytes that process the blood play a large role in protein synthesis, carbohydrate metabolism, lipid metabolism, and detoxification.
Which veins are associated with the intestinal veins?
Other than the previously mentioned hepatic and related veins, the principal associated intestinal veins are the inferior mesenteric vein, superior mesenteric vein, and the splenic vein (which converges with the pancreatic veins before it meets the inferior mesenteric vein, and ultimately meets the superior mesenteric vein). The left and right gastric veins, which form an arc along the lesser curvature of the stomach, also empty into the hepatic portal vein. Broadly, the hepatocytes that process the blood play a large role in protein synthesis, carbohydrate metabolism, lipid metabolism, and detoxification.Solidify your knowledge about the hepatic portal vein
Where does the portal vein go before the liver?
However, before reaching the liver, the portal vein bisects into the left and right, with each side further dividing from venous branches into portal venules. These portal venule branches run alongside hepatic arterioles in the spaces between the liver lobules, and these two vessels, along with a common bile duct, form the hepatic portal triad.
Where is the left hepatic vein located?
It drains segments 2, 3, 4a and 4b. It is always located anterior to the left portal vein. The vertical plane of the left hepatic vein separates the segments 4a and 4b from segments 2 and 3.
What is the middle hepatic vein?
Middle hepatic vein. The middle hepatic vein (MHV) runs at the middle hepatic fissure and drains segments 4a, 4b, 5 and 8. The vertical plane of the middle hepatic vein separates the segments 5 and 8 (posterolateral to this plane) from segments 4a and 4b (anteromedial to this plane).
What are the three veins in the liver?
Three large intrahepatic veins drain the liver parenchyma, into the inferior vena cava (IVC), and are named the right hepatic vein , middle hepatic vein and left hepatic vein. The veins are important landmarks, running in between and defining the segments of the liver.
Which vein drains segments 5 and 7?
The right hepatic vein ( RHV) runs in the right hepatic fissure and drains segments 5, 6, 7 and 8. The vertical plane of the right hepatic vein separates the segments 6 and 7 (posterior to the plane) from segments 5 and 8 (anterior to this plane).
Which veins drain into the inferior vena cava?
Caudate lobe veins. The highly variable caudate lobe veins ( or a single vessel) drain directly into the inferior vena cava. These veins are occasionally referred to as the Spigelian veins and may become prominent in the setting of hepatic venous obstruction, as in Budd-Chiari syndrome.
Is the right hepatic vein a dominant vein?
The right hepatic vein is a single dominant vein in ~70% (range 60-78%) of individuals. There may be an early bifurcation, early trifurcation or even multiple right hepatic veins entering the IVC. Hence this may make it difficult to accurately deduce segmental anatomy of the liver.
Why does hepatic vein obstruction cause liver damage?
Causes. Hepatic vein obstruction prevents blood from flowing out of the liver and back to the heart. This blockage can cause liver damage. Obstruction of this vein can be caused by a tumor or growth pressing on the vessel, or by a clot in the vessel (hepatic vein thrombosis).
How does blood clotting happen?
Blood clotting normally occurs when there is damage to a blood vessel. Platelets immediately begin to adhere to the cut edges of the vessel and release chemicals to attract even more platelets. A platelet plug is formed, and the external bleeding stops. Next, small molecules, called clotting factors, cause strands of blood-borne materials, called fibrin, to stick together and seal the inside of the wound. Eventually, the cut blood vessel heals and the blood clot dissolves after a few days.
Which organ processes nutrients in the blood and filters out toxic substances?
The liver processes the nutrients in this blood and filters out toxic substances. The hepatic veins then carry the blood away from the liver and into the inferior vena cava, which leads to the right atrium, one of the four chambers of the heart.
What happens when a cut blood vessel heals?
Eventually, the cut blood vessel heals and the blood clot dissolves after a few days. Blood clots (fibrin clots) are the clumps that result when blood coagulates.
How is the hepatic vein shape determined?
The shape of the hepatic vein spectral Doppler waveform is primarily determined by pressure changes in the right atrium, or more exactly the blood flow resulting from the resultant pressure gradients.
What is the p wave on a hepatic vein?
Radiographic features. The normal periodic hepatic vein waveform is typically described in four parts: coinciding with the "p wave" on the electrocardiogram, contraction elevates pressure within the right atrium creating a gradient for late diastolic filling of the right ventricle.
What does a change in the hepatic venous waveform mean?
Alterations in the normal hepatic venous Doppler waveform often indicate cardiac dysfunction , although it may also reflect disease of the hepatic parenchyma and/or vasculature. The consequent hemodynamic perturbations may manifest as:
What is the term for a spectral waveform that is transmitted by cardiac motion?
Some prefer the term "periodic" since the term "triphasic" already has a specific application in arterial spectral Doppler waveforms and since "periodic" suggests that the waveform is transmitted by cardiac motion rather than systolic flow.
Where does the C wave occur?
Sometimes a c wave occurs as a second small inflection above the baseline, right after the a wave, reflecting the effect of the tricuspid valve bulging into the right atrium.
Where are short gastric varices found?
Short gastric or left gastric varices are found below the left lobe of the liver (Fig. 22.13). In patients with spontaneous splenorenal shunts, a direct communication, often “U-shaped,” will be observed between the splenic and left renal veins (Fig. 22.14). The left renal vein is typically dilated and flow will be reversed in the main PV. Spontaneous portocaval shunts are less common, but if large are associated with focal dilatation of the IVC at the level of the shunt as well as hepatic encephalopathy, since a large amount of blood draining from the bowel will be shunted into the systemic circulation without detoxification by the liver. Surgical shunts appear similar to spontaneous shunts on DUS examination. Although these are the most readily ultrasound-detected variceal patterns, varices can occur virtually anywhere in the retroperitoneum or abdomen (Figs. 22.15 and 22.16).
How many patients with GE varices will bleed?
It is estimated that approximately one-third of patients with GE varices will present with significant variceal bleeding. 24, 31, 32 Risk factors for hemorrhage include large varices, a portosystemic gradient greater than 12 to 15 mm Hg, a coronary vein greater than 7 mm in diameter, ascites, acute alcohol binge, and exercise. 3, 4, 15, 33 Medical management of significant bleeding from GE varices includes endoscopic sclerotherapy, variceal band ligation, vasoconstrictors (vasopressin, nitroglycerin, somatostatin, and octreotide), and balloon tamponade. Bleeding is controlled by a combination of endoscopic and pharmacologic treatment in up to 80% to 90% of cases. 24, 32, 34, 35, 36 However, approximately 70% of patients will rebleed, 35, 36, 37 and the mortality rate in such patients is extremely high (30% to 40%) despite aggressive medical management including prophylactic treatment with β-blockers. 35, 36, 37, 38
What is portal hypertension?
Ultrasound Evaluation of the Portal and Hepatic Veins. Portal hypertension (PHT) is an extremely common medical problem worldwide. In Western countries, PHT most commonly occurs secondary to underlying liver cirrhosis, either viral or alcohol induced.
Can cirrhosis cause PHT?
While cirrhosis is the most common cause of PHT in the United States, it should be remembered that cirrhosis can be present in the absence of PHT, and PHT can occur without cirrhosis. FIGURE 22.1. Normal portal vein.
Is cirrhosis a risk factor for HCC?
Patients with cirrhosis are at increased risk for developing HCC. The incidence of HCC in patients with cirrhosis is estimated at 3% per year, and patients with cirrhosis due to hepatitis B, hepatitis C, and hemochromatosis seem to have the highest risk for developing HCC.
Is it safe to have an ultrasound of the liver?
Furthermore, there are no known risks associated with ultrasound examination of the liver. Ultrasound is also an excellent means of evaluating patients for portal vein (PV) thrombosis and Budd-Chiari syndrome (BCS), which may precipitate acute deterioration of liver function in patients with cirrhosis and HCC.
Is PHT a viral disease?
In Western countries, PHT most commonly occurs secondary to underlying liver cirrhosis, either viral or alcohol induced. Morbidity is primarily related to bleeding from gastroesophageal (GE) varices and liver failure. However, these patients are also at increased risk for developing hepatocellular carcinoma (HCC).
What is the mean ref needed for a right hepatic vein?
Normally the right hepatic vein measures <6 mm and, in these patients, its mean is ~9 mm ref needed .
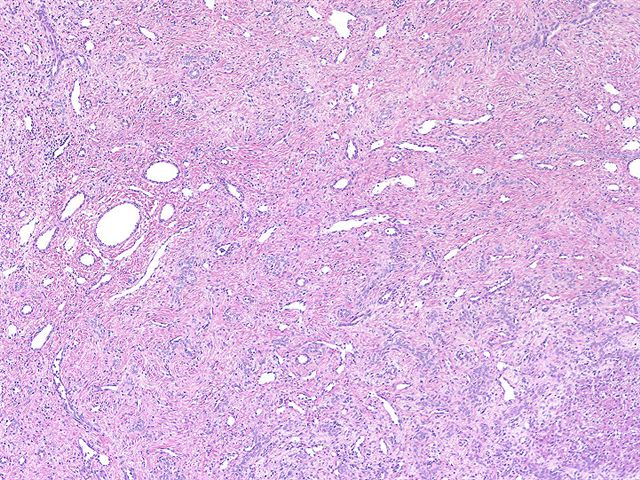
What is a congested liver?
Passive hepatic congestion, also known as congested liver in cardiac disease, describes the stasis of blood in the hepatic parenchyma, due to impaired hepatic venous drainage, which leads to the dilation of central hepatic veins and hepatomegaly .
What causes hepatic parenchyma to die?
Elevated hepatic venous pressure and a decrease in hepatic venous flow cause hypoxia in hepatic parenchyma, and eventual diffuse hepatocyte death and fibrosis. This results in a micronodular cirrhosis, which is indistinguishable from cirrhosis produced by other causes 2.
What is passive hepatic congestion?
Passive hepatic congestion is a well-studied result of acute or chronic right-sided heart failure.
Is hepatic congestion a form of heart disease?
All forms of heart disease (congenital or acquired) are linked to passive hepatic congestion.

Overview
- Structure & Location
The hepatic veins arise from the core vein central liver lobule—a subsection of the liver—and drain blood to the IVC. These veins vary in size between 6 and 15 millimeters (mm) in diameter, and they’re named after the corresponding part of the liver that they cover. These include:1 1. Righ… - Anatomical Variations
Variations to the anatomy of the hepatic veins are not uncommon and occur in approximately 30% of the population.1 In most cases, the right hepaticvein will be what’s affected. Doctors have observed early bifurcation (splitting into two) or trifurcation (splitting into three) of this vein—wit…
Structure
Clinical significance
Additional images
The hepatic veins are the veins that drain de-oxygenated blood from the liver into the inferior vena cava. There are usually three upper hepatic veins draining from the left, middle, and right parts of the liver. These are larger than the group of lower hepatic veins that can number from six to twenty. All of the hepatic veins drain into the inferior vena cava.
External links
The hepatic veins are divided into an upper and a lower group. The upper three drain the central veins from the right, middle, and left regions of the liver and are larger than the lower group of veins.
The lower group of from six to twenty smaller hepatic veins come from the right lobe and the caudate lobe, are in contact with the hepatic tissue, and are valveless. All the veins empty into th…