What is the function of angiotensin II in the kidney?
Angiotensin II serves at least three important functions in the kidney: autoregulation of GFR, reduction of salt excretion through direct and indirect actions on renal tubular cells, and growth modulation of renal cells expressing AT1 receptors. 7.12.3.4.1 Regulation of GFR
How does angiotensin II increase sodium reabsorption?
In the proximal convoluted tubule of the kidney, angiotensin II acts to increase Na-H exchange, increasing sodium reabsorption. Increased levels of Na in the body acts to increase the osmolarity of the blood, leading to a shift of fluid into the blood volume and extracellular space (ECF).
How do angiotensin II receptor blockers work?
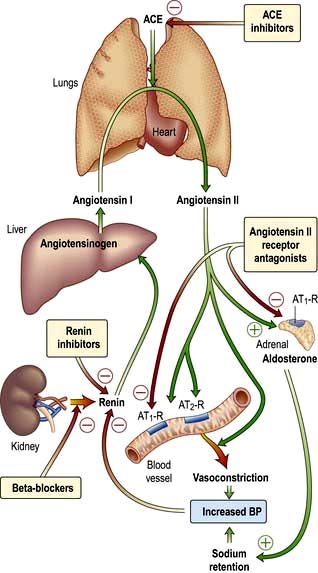
Angiotensin II receptor blockers (ARBs) decrease the effects of angiotensin. This protein causes blood vessels to become too narrow, leading to high blood pressure. ARBs also treat heart failure and kidney disease and lower the risk of heart attacks and strokes. The medicine relaxes blood vessels, so blood flows more freely.
Where is angiotensinogen produced in the body?
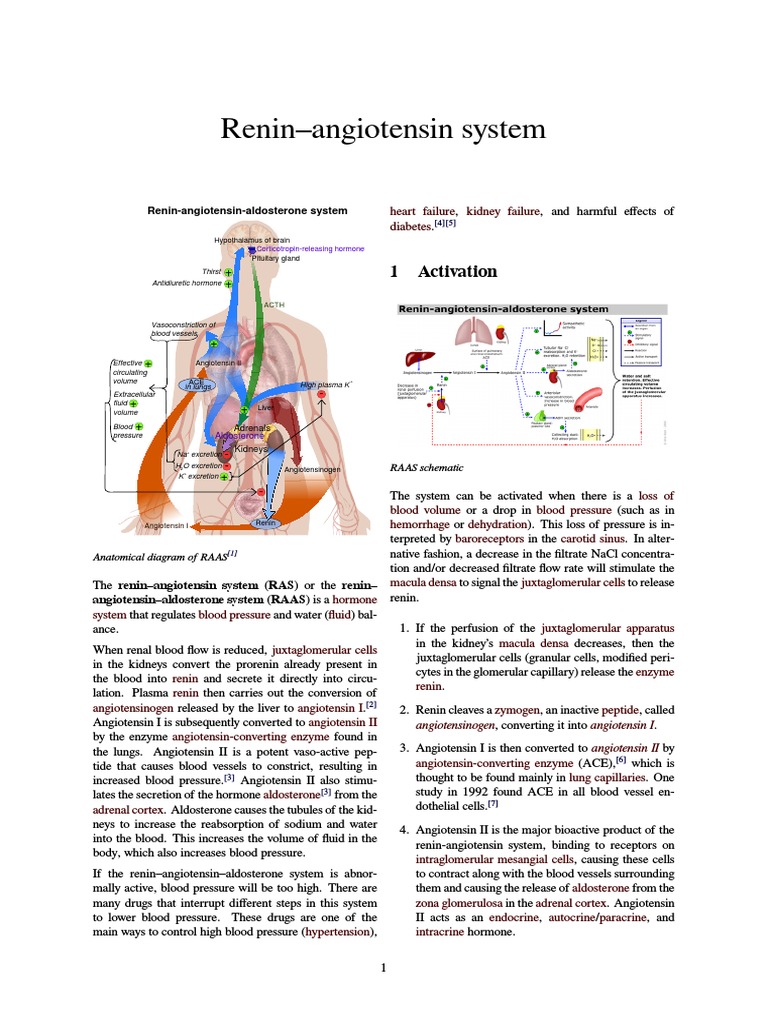
Angiotensinogen is produced in the liver and is found continuously circulating in the plasma. Renin then acts to cleave angiotensinogen into angiotensin I. Angiotensin I is physiologically inactive, but acts as a precursor for angiotensin II.
What is the role of angiotensin II in the kidney?
Why is angiotensin important?
About this website

How does angiotensin 2 affect the kidneys?
In the kidney, angiotensin II exerts its effects to conserve salt and water through a combination of the hemodynamic control of renal blood flow and glomerular filtration rate and tubular epithelial cell sodium chloride and water transport mechanisms.
What part of the nephron does angiotensin II affect?
Angiotensin II constricts both the afferent (preglomerular) and efferent (postglomerular) arterioles but preferentially increases efferent resistance [2].
Where is angiotensin II produced in the kidney?
Thus, it is not surprising that angiotensin II can be produced locally within the kidneys because of the activity of a complete renin-angiotensin system (RAS) expressed along the nephron. In fact, the renal RAS can play an important role in disease.
What is the site of action of angiotensin II?
Angiotensin II acts on the adrenal cortex, causing it to release aldosterone, a hormone that causes the kidneys to retain sodium and lose potassium.
Where are angiotensin II receptors located?
Table 1.ReceptorLocationAT1Vessels, brain, heart, kidney, adrenal gland, and nervesAT2Adrenal gland, heart, brain, myometrium, fetus, and injured tissuesAT3Neuroblastoma cells in amphibiansAT4Brain, heart, vessels, lungs, prostate, adrenal gland, and kidney
What are the three actions of angiotensin II?
Angiotensin II (Ang II) raises blood pressure (BP) by a number of actions, the most important ones being vasoconstriction, sympathetic nervous stimulation, increased aldosterone biosynthesis and renal actions.
What is angiotensin II and what process does it facilitate?
Angiotensin II causes the muscular walls of small arteries (arterioles) to constrict (narrow), increasing blood pressure. Angiotensin II also triggers your adrenal glands to release aldosterone and your pituitary gland to release antidiuretic hormone (ADH, or vasopressin).
What is the role of angiotensin II in the body?
The overall effect of angiotensin II is to increase blood pressure, body water and sodium content. Angiotensin II has effects on: Blood vessels – it increases blood pressure by causing constriction (narrowing) of the blood vessels.
How does angiotensin 2 regulate GFR?
Angiotensin II (AngII) helps to prevent excessive decreases in GFR in different physiological and pathophysiological conditions by preferentially constricting the efferent arterioles, an action that can be mediated by either intrarenally formed or circulating AngII.
What receptors does angiotensin 2 bind to?
Abstract. Angiotensin II (Ang II) is the active peptide of the renin-angiotensin system (RAS). Ang II binds to AT1 and AT2 receptors to conduct signals.
What is the effect of angiotensin II on the GFR quizlet?
Angiotensin II constricts arterioles throughout the body. In the kidney it has a greater affect on the efferent arterioles than on the afferent arterioles so it tends to maintain the GFR despite the decrease in renal blood flow due to constriction of the afferent arteriole.
Which are actions of angiotensin II quizlet?
(The most prominent actions of angiotensin II are vasoconstriction (not dilation) and stimulation of aldosterone release. Both actions raise blood pressure. In addition, angiotensin II can act on the heart and blood vessels to cause remodeling and hypertrophy.
What does angiotensin II stimulate?
Angiotensin II is the main effector molecule of the RAS. It causes increases in blood pressure, influences renal tubuli to retain sodium and water, and stimulates aldosterone release from adrenal gland.
What is the effect of angiotensin II on the GFR quizlet?
Angiotensin II constricts arterioles throughout the body. In the kidney it has a greater affect on the efferent arterioles than on the afferent arterioles so it tends to maintain the GFR despite the decrease in renal blood flow due to constriction of the afferent arteriole.
How does angiotensin II affect water reabsorption?
Angiotensin II promotes expansion of the plasma volume by promoting renal sodium and water reabsorption.
How does angiotensin 2 regulate GFR?
Angiotensin II (AngII) helps to prevent excessive decreases in GFR in different physiological and pathophysiological conditions by preferentially constricting the efferent arterioles, an action that can be mediated by either intrarenally formed or circulating AngII.
Impact of angiotensin II on the kidney: does an angiotensin II ... - PubMed
The renin-angiotensin system (RAS) regulates blood pressure, volume, and electrolyte balance. Derangements of the RAS may contribute to hypertension and renal injury, particularly in patients with types 1 or 2 diabetes. Angiotensin-converting enzyme (ACE) inhibitors have been proven to be beneficial …
Angiotensin II and the maintenance of GFR and renal blood flow during ...
The time course of the renal blood flow and GFR responses to narrowing of the renal artery in conscious dogs is reviewed. The initial response to this threat to renal perfusion is renal vasodilatation, but within minutes a secondary vasoconstriction mediated by angiotensin II begins to develop. Angi …
Angiotensin II - an overview | ScienceDirect Topics
M.J. McKinley, B.J. Oldfield, in Encyclopedia of Neuroscience, 2009 Intracellular Signaling. Angiotensin II acts on neuronal AT 1 receptors to stimulate firing of action potentials. While the intracellular signaling events to which AT 1 receptors are coupled have been studied in only a few brain sites, AT 1 receptor signaling occurs via G-protein (G q) coupled to the third intracellular loop.
Classical Renin-Angiotensin System in Kidney Physiology - PMC
Classical renin-angiotensin system (RAS). Through sequential cleavage of protein substrates by specific proteases, the multi-functional peptide hormone angiotensin II is generated by the “classical” RAS. The primary substrate for the RAS is angiotensinogen.While the liver is the primary source of angiotensinogen, it is also produced in other tissues including the kidney.
What nerves activate renin?
Renal injury will also activate renal afferent nerves to stimulate β-adrenergic output from the central nervous system that can stimulate renin release. Activation of the local RAS has also been shown in renal injury, indicated by upregulation of ACE and the infiltration of leukocytes expressing angiotensin II. 2.
Does angiotensin II activate fibroblasts?
Angiotensin II also activates renal fibroblasts to become myofibroblasts, stimulates the production of the profibrotic cytokine TGF-β, induces oxidative stress, stimulates chemokines and osteopontin that may cause local inflammation, and stimulates vascular and mesangial cell proliferation and hypertrophy.
Does angiotensin II cause hypertrophy?
It is known that angiotensin II can also induce subtle changes in the renal vasculature, glomeruli, and tubulointerstitial areas, 12 and measurements of arteriolar hypertrophy, intrarenal inflammation, and endothelial turnover were not performed.
Does angiotensin cause renal injury?
A variety of mechanisms has been suggested by which angiotensin II causes renal injury. Angiotensin II may cause pressure-induced renal injury via its ability to induce systemic and glomerular hypertension or cause ischemia-induced renal injury secondary to intrarenal vasoconstriction and decreased renal blood flow.
Where does angiotensin II affect vasoconstriction?
The effect of angiotensin II on vasoconstriction takes place in systemic arterioles. Here, angiotensin II binds to G protein-coupled receptors, leading to a secondary messenger cascade that results in potent arteriolar vasoconstriction. This acts to increase total peripheral resistance, causing an increase in blood pressure.
How long does angiotensin II last?
In the plasma, angiotensin II has a half-life of 1-2 minutes, at which point peptidases degrade it into angiotensin III and IV. Angiotensin III has been shown to have 100% of the aldosterone stimulating effect of angiotensin II, but 40% of the pressor effects, while angiotensin IV has further decreased the systemic effect.
How do ACE inhibitors work?
A common use for ACE inhibitors or ARBs is in the management of hypertension. In these cases, blocking or decreasing levels of angiotensin II will lead to a reduction in blood pressure. They achieve this goal by decreasing sodium and water reabsorption, leading to a reduction in blood volume, and decreasing arteriolar tone. In addition, these drugs are often used in the management of diabetes mellitus. Patients with diabetes mellitus often have renal manifestations such as proteinuria due to excess glucose damaging the glomerulus. Using ACE inhibitors or ARBs can decrease efferent arteriolar tone, leading to a reduction in pressure on the glomerulus. Thus, they are frequently used for prevention of worsening diabetic nephropathy.
How long does it take for aldosterone to work?
As a result, it enacts change by binding to nuclear receptors and altering gene transcription. Thus, the effects of aldosterone may take hours to days to begin, while the effects of angiotensin II are rapid. The effect of angiotensin II on vasoconstriction takes place in systemic ...
What are the three compounds that are found in the syringe of the kidney?
It is composed of three major compounds: renin, angiotensin II, and aldosterone. These three act to elevate arterial pressure in response to decreased renal blood pressure, decreased salt delivery to the distal convoluted tubule, and/or beta-agonism.
Which hormone stimulates the release of aldosterone?
Angiotensin II also acts on the adrenal cortex, specifically the zona glomerulosa. Here, it stimulates the release of aldosterone. Aldosterone is a steroid hormone that causes an increase in sodium reabsorption and potassium excretion at the distal tubule and collecting duct of the nephron.
What is the role of the renin-angiotensin-aldosterone system in the?
The renin–angiotensin–aldosterone system (RAAS) is a critical regulator of blood volume and systemic vascular resistance. While the baroreceptor reflex responds in a short-term manner to decreased arterial pressure, the RAAS is responsible for more chronic alterations.
What is the function of angiotensin II?
Angiotensin II serves at least three important functions in the kidney: autoregulation of GFR, reduction of salt excretion through direct and indirect actions on renal tubular cells, and growth modulation of renal cells expressing AT1 receptors.
What is the effect of angiotensin II on the proximal tubule?
The effect of angiotensin II on the proximal tubule appears to be partly due to the activation of the sodium–hydrogen (Na + –H +) antiporter in the luminal membrane ( Cogan et al. 1991; Quan and Baum 1999 ).
How does angiotensin II affect GFR?
1990 ). Although both afferent and efferent arterioles are constricted by angiotensin II, the efferent arteriole has a greater increase in resistance due to a smaller basal diameter ( Denton et al. 1992 ), which may be partly due to different mechanisms of constriction because calcium channel blockers abolish the afferent response while having little or no effect on the increase in efferent tone ( Carmines et al. 1992 ). The net effect is elevation of the hydraulic pressure in the glomerular capillary ( PGC ), which tends to maintain the GFR even under conditions of renal hypoperfusion. In contrast, at higher concentrations, angiotensin II can lower GFR by lowering the surface area available for filtration and by sensitizing the afferent arteriole to the constricting signal of the tubuloglomerular feedback ( Ichikawi and Harris 1991; Myers et al. 1975 ). Hence, the net effect of angiotensin II on GFR varies, depending upon the underlying condition.
How long to grow H295R cells?
Grow H295R/TR SF-1 cells in 24-well plates in basal conditions or under stimulation with forskolin (10 μg/mL) or angiotensin II (10 nM) for 4 days.
How does angiotensin II increase plasma volume?
Angiotensin II promotes expansion of the plasma volume by promoting renal sodium and water reabsorption. Angiotensin II mediates this by directly stimulating sodium reabsorption in the early proximal tubule (Cogan 1990a; Ichikawi and Harris 1991; Quan and Baum 1997) and by increasing the secretion of aldosterone from the adrenal cortex ( Kifor et al. 1991 ), which in turn promotes sodium reabsorption in the cortical collecting tubule.
What is Ang II?
Ang II is the major bioactive product of the renin–angiotensin system (RAS) and has been implicated in a variety of cardiovascular diseases. These include vascular hypertrophy and hyperplasia, atherosclerosis, hypertension, and heart failure ( Heeneman et al. 2007; Higuchi et al. 2007; Kazi and Deswal 2008 ). Most of the physiological and pathophysiological effects of Ang II in the cardiovascular system have been attributed to the AT 1 receptor, a GPCR that has been shown to activate multiple signaling pathways ( Higuchi et al. 2007 ). Second messengers involved in AT 1 signaling include IP 3, DAG, ROS, RhoA, and PKC. The AT 1 receptor has also been shown to transactivate epidermal growth factor receptors (EGFRs) that lead to the activation of the Raf/ERK and PI3K/Akt pathways, a process implicated in vascular hypertrophy. The RhoA/ROK pathway and NAD (P)H oxidase activation downstream of AT 1 receptors both have also been implicated in the cell growth response to Ang II. Finally, prolonged Ang II elevations increase sensitivity of VSMC to other vasoconstrictors, and thus increase vascular resistance ( Maeso et al. 1996 ).
Which receptors regulate salt and water homeostasis?
Angiotensin Receptors . Angiotensin II is a vasoconstrictor with proliferative effects involved in the regulation of salt and water homeostasis and pathological remodeling of the heart and vessels usually through AT1 -subtype receptors [115].
What is the role of angiotensin II in the kidney?
Several lines of evidence suggest strongly that angiotensin plays an important role in the maintenance of renal vascular resistance and arterial pressure in several physiological and pathophysiological states ...
Why is angiotensin important?
Several lines of evidence suggest strongly that angiotensin plays an important role in the maintenance of renal vascular resistance and arterial pressure in several physiological and pathophysiological states with increased activity of the renin-angiotensin system.