Where is glucose reabsorbed in the body?
Most of the glucose entering the tubular system is reabsorbed along the nephron segments, primarily in the proximal tubule, such that urine is almost free of glucose. This is different in diabetes, where the filtered glucose exceeds the transport capacity of the tubular system for glucose and glucosuria occurs.
How is glucose absorbed from the gastrointestinal tract?
When the stomach digests food, the carbohydrate (sugars and starches) in the food breaks down into another type of sugar, called glucose. The stomach and small intestines absorb the glucose and then release it into the bloodstream. Which system is responsible for breaking down food into glucose?
What are common causes of high blood sugar levels?
What Causes Blood Sugar to Rise in Non-Diabetics?
- Non-Diabetic Hyperglycemia and Prediabetes. You are considered to have impaired glucose tolerance or prediabetes if you have a fasting glucose level between 100–125 mg/dL.
- Common Causes. ...
- Genetics. ...
- Lifestyle Risk Factors. ...
- A Word From Verywell. ...
Where does glucose enter the blood?
The glucose goes straight from the digestive system into the bloodstream after food is consumed and digested. But glucose can only enter cells if there is insulin in the bloodstream too. Without insulin, the cells would starve. After we eat, blood sugar concentrations rise.
See more

Where is glucose absorbed the most?
In the presence of high concentrations of glucose (more than 30 mM) in the lumen of the small intestine, arising after eating, active glucose transport is saturated and additional mechanisms may be involved in the absorption of glucose in the small intestine.
Where is glucose absorbed first?
the liverAbsorption: Going to the Blood Stream The first organ to receive glucose, fructose, and galactose is the liver. The liver takes them up and converts galactose to glucose, breaks fructose into even smaller carbon-containing units, and either stores glucose as glycogen or exports it back to the blood.
Is glucose absorbed in the stomach?
Following delivery to the stomach, the sugar empties into the duodenum (1), where it is absorbed into the blood (2). Before entering the general circulation, glucose passes through the liver, where it may be stored and released (3, 4).
Where is glucose absorbed in the small intestine?
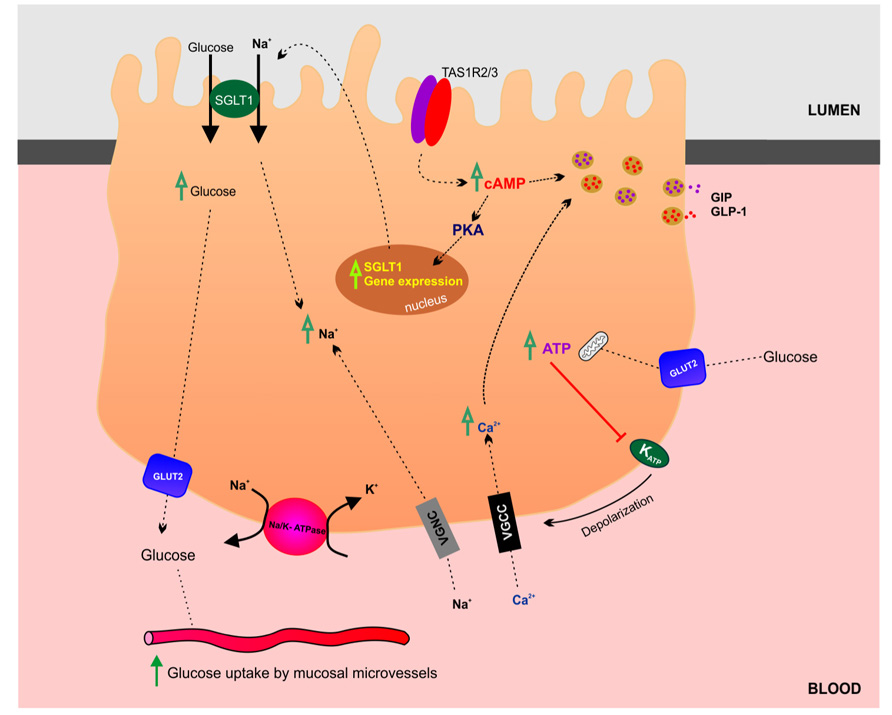
Glucose absorption takes place in small intestinal villus cells by SGLT1, which is driven by active sodium extrusion via the basolateral Na+/K+ ATPase.
How Is Glucose Absorbed From The Gastrointestinal Tract? How Are Blood Glucose Levels Maintained?
Almost 80 percent of these monosaccharides are glucose. Glucose is absorbed in small intestine by absorptive cells. The process of transport of glucose from intestinal lumen into the absorptive cell has two stages. In the first stage sodium ion from inside the cells are transported to interstitial fluid. This leads to low sodium concentration inside the cell. Then starts the second stage. As a result of low sodium inside the cells, sodium ions are transported from intestinal lumen by facilitated diffusion (diffusion with the help of transport protein). The transport protein that helps in this case, has a peculiarity. It transports sodium ion with glucose. Actually this protein drags glucose along with sodium ion from the lumen into the cell. Once into the cell, other transport proteins and enzymes cause facilitated diffusion of glucose through basal and lateral membranes of the cell into interstitial fluid and from there into the blood. Glucose absorption : Regulation of blood glucose level In a normal person the blood glucose level is narrowly controlled by following mechanisms: Liver acts as a blood glucose buffer system. When after a meal blood glucose rises and insulin is secreted, two thirds of the glucose absorbed from gut is stored in the liver in the form of glycogen. Then during succeeding hours, liver releases glucose back into blood to maintain a narrow range of blood glucose level. When blood glucose concentration rises too high, insulin is secreted; which decreases the level. Conversely when glucose level drops too low glucagon is secreted and restores Continue reading >>
What are the two ways in which glucose uptake can take place?
The two ways in which glucose uptake can take place are facilitated diffusion (a passive process) and secondary active transport (an active process which depends on the ion-gradient which is established through the hydrolysis of ATP, known as primary active transport).
How does the pancreas regulate glucose levels?
This is done by the pancreas, which releases hormones that regulate the usage and storage of glucose by cells. Type 1 diabetics are unable to make sufficient quantities of one of these hormones – insulin - and must therefore control their blood sugar levels by injecting insulin, as well as by carefully controlling their diet and exercise levels. Controlling rising blood sugar It is important that blood glucose level is kept within a narrow range due to its importance as an energy source for respiration - but also because of the effects it could have in causing the movement of water into and out of cells by osmosis Having eaten a meal containing sugars or starch (eg sweets, potatoes, bread, rice or pasta), the starch and large sugars are digested down into glucose and absorbed across the small intestine wall into the bloodstream. This triggers a rise in blood glucose concentration. The pancreas monitors and controls the concentration of glucose in the blood. In response to an increase in blood glucose level above the normal level, the pancreas produces a hormone called insulin which is released into the bloodstream. Insulin causes glucose to move from the blood into cells, where it is either used for respiration or stored in liver and muscle cells as glycogen. The effect of this is to lower the blood glucose concentration back to normal. The animation below shows how this works. You have an old or no version of Flash - you need to upgrade to view this content! Go to the WebWise Flash install guide Diabetes There are two main types of diabetes: Type 1 which usually develops during childhood Type 2 which is usually develops in later life This syllabus focuses on Type 1 diabetes - whic Continue reading >>
How does fructose enter the cell?
Fructose, chemically different from glucose and galactose, enters into the cells by facilitated diffusion, also called passive transport (no energy expenditure) thank to the transporter GLUT5 (acronym of GLucose Transporter type 5). All the three monosaccharides leave the cell through the transporter GLUT2 (acronym of GLucose Transporter type 2), ...
How do monosaccharides enter the bloodstream?
The passage of monosaccharides from the intestinal lumen to the inside of the cell, and, from this point into the bloodstream, does not occur by simple diffusion, that is freely following the only concentration gradient (from a region of higher concentration to one of lower), but is mediate by specific proteic transporters localized into the plasmatic membrane of enterocytes. The passage of both the glucose and the galactose, chemically very similar, is mediated by a transporter called SGLT1, acronym of Sodium-dependent GLucose coTransporter 1, which carries out the co-transport of one molecule of glucose/galactose together with two sodium ions (then energy will be spent for removing sodium from the cell and so keeping the gradient along which other sodium may enter again). Fructose, chemically different from glucose and galactose, enters into the cells by facilitated diffusion, also called passive transport (no energy expenditure) thank to the transporter GLUT5 (acronym of GLucose Transporter type 5). All the three monosaccharides leave the cell through the transporter GLUT2 (acronym of GLucose Transporter type 2), enter into the bloodstream (portal vein), reach the liver and then are distributed to different tissues. The absorption of electrolytes and solutes, in this case NaCl and monosaccharides, but the same is true e. g. for aminoacids, is accompanied by the movement of water, presumably by virtue of the osmotic gradient produced by absorption of the above-said molecules. It is thought that SGLT1 is one of the major enhancer of water absorption and, based on experimental data obtained from studies on Xenopus oocytes, it seems that the transport of two sodium ions and one molecule of glucose is accompanied by the passage of 260 molecules of water, that is about 3 l Continue reading >>
Where are glucose transporters located?
GLUT1 and GLUT3 are located in the plasma membrane of cells throughout the body , as they are responsible for maintaining a basal rate of glucose uptake.
Where do monosaccharides go?
All the three monosaccharides leave the cell through the transporter GLUT2 (acronym of GLucose Transporter type 2), enter into the bloodstream (portal vein), reach the liver and then are distributed to different tissues.
How Is Glucose Absorbed By The Body?
Active transport: The remaining glucose is absorbed by active transport with sodium ions. Step 1 = Sodium ions are actively transported out of the small intestine epithelial cells and into the blood streamby the sodium-potassiumpump. Thiscreatesa concentrationgradient, as there is now a higher concentration of sodium ions in the small intestinelumen than in the epithelial cells. Step 2 = This causes sodium ions to diffuse from the small intestine lumen into the cell down theirconcentrationgradient via asodium-glucose co-transporter protein, which brings glucose into the cell at the same time. This causes the glucose concentrationin the cell to increase. Step 3 = Glucose diffuses out of the cell and into the blood through a protein channel. This is facilitated diffusion. Continue reading >>
How does the body get glucose?
Your body can break down fats and even proteins to get the energy it needs. But it’s glucose, derived from the digestion of carbohydrates, that your body desires. Glucose is the main source of energy for every single cell, and it is the preferred energy type for brain cells. If you have diabetes, your body has problems handling glucose, which can be very dangerous for your health. Video of the Day All carbohydrates, with the exception of fiber, eventually wind up as glucose. However, the way they get there varies. Sugars, which are simple carbs, are very small molecules that convert into glucose quickly after combining with enzymes in your small intestine. Starches, which are complex carbohydrates, undergo numerous steps before glucose is formed. When you chew, your mouth secretes saliva, an enzyme that starts breaking down complex starch compounds. Saliva turns starches into a kind of simple carbohydrate. As the simple molecules approach your small intestine, the enzymes there kick in again to break them down further, converting them into glucose. Your intestinal tract is lined with numerous microvilli, which are tiny fingerlike protrusions that increase surface area for the maximum absorption of nutrients. These microvilli absorb glucose molecules and send them straight into your bloodstream. Once your brain senses that glucose is present, it sends signals to your pancreas to secrete the hormone insulin. Insulin is like a gatekeeper, opening up cell walls and allowing glucose to enter. Whatever glucose isn’t needed right away gets converted into glycogen, a polysaccharide that is stored in your liver and muscles as a backup source of energy. If you have diabetes, your body doesn’t regulate glucose levels well because it has a problem with insulin. With Type 1 di Continue reading >>
How do monosaccharides enter the bloodstream?
The passage of monosaccharides from the intestinal lumen to the inside of the cell, and, from this point into the bloodstream, does not occur by simple diffusion, that is freely following the only concentration gradient (from a region of higher concentration to one of lower), but is mediate by specific proteic transporters localized into the plasmatic membrane of enterocytes. The passage of both the glucose and the galactose, chemically very similar, is mediated by a transporter called SGLT1, acronym of Sodium-dependent GLucose coTransporter 1, which carries out the co-transport of one molecule of glucose/galactose together with two sodium ions (then energy will be spent for removing sodium from the cell and so keeping the gradient along which other sodium may enter again). Fructose, chemically different from glucose and galactose, enters into the cells by facilitated diffusion, also called passive transport (no energy expenditure) thank to the transporter GLUT5 (acronym of GLucose Transporter type 5). All the three monosaccharides leave the cell through the transporter GLUT2 (acronym of GLucose Transporter type 2), enter into the bloodstream (portal vein), reach the liver and then are distributed to different tissues. The absorption of electrolytes and solutes, in this case NaCl and monosaccharides, but the same is true e. g. for aminoacids, is accompanied by the movement of water, presumably by virtue of the osmotic gradient produced by absorption of the above-said molecules. It is thought that SGLT1 is one of the major enhancer of water absorption and, based on experimental data obtained from studies on Xenopus oocytes, it seems that the transport of two sodium ions and one molecule of glucose is accompanied by the passage of 260 molecules of water, that is about 3 l Continue reading >>
How does the small intestine absorb nutrients?
Absorption in the Small Intestine The absorption of nutrients occurs partially by diffusion through the wall of the small intestine. Learning Objectives Describe the role played by the small intestine in the absorption of nutrients Key Takeaways Digested food is able to pass into the blood vessels in the wall of the small intestine through the process of diffusion. The inner wall, or mucosa, of the small intestine is covered in wrinkles or folds called plicae circulares that project microscopic finger-like pieces of tissue called villi, which in turn have finger-like projections known as microvilli. The function of the plicae circulares, the villi, and the microvilli is to increase the amount of surface area available for the absorption of nutrients. Each villus transports nutrients to a network of capillaries and fine lymphatic vessels called lacteals close to its surface. villi: Tiny, finger-like projections that protrude from the epithelial lining of the intestinal wall. plicae circulares: These circular folds (known as the valves of Kerckring or the valvulae conniventes) are large, valvular flaps that project into the lumen of the bowel. diffusion: The act of diffusing or dispersing something, or the property of being diffused or dispersed; dispersion. Examples of nutrients absorbed by the small intestine include carbohydrates, lipids, proteins, iron, vitamins, and water. The Small Intestine The small intestine is the part of the gastrointestinal tract between the stomach and the large intestine where much of the digestion of food takes place. The primary function of the small intestine is the absorption of nutrients and minerals found in food. Digested nutrients pass into the blood vessels in the wall of the intestine through a process of diffusion. The inner wall, Continue reading >>
How does the pancreas regulate glucose levels?
This is done by the pancreas, which releases hormones that regulate the usage and storage of glucose by cells. Type 1 diabetics are unable to make sufficient quantities of one of these hormones – insulin - and must therefore control their blood sugar levels by injecting insulin, as well as by carefully controlling their diet and exercise levels. Controlling rising blood sugar It is important that blood glucose level is kept within a narrow range due to its importance as an energy source for respiration - but also because of the effects it could have in causing the movement of water into and out of cells by osmosis Having eaten a meal containing sugars or starch (eg sweets, potatoes, bread, rice or pasta), the starch and large sugars are digested down into glucose and absorbed across the small intestine wall into the bloodstream. This triggers a rise in blood glucose concentration. The pancreas monitors and controls the concentration of glucose in the blood. In response to an increase in blood glucose level above the normal level, the pancreas produces a hormone called insulin which is released into the bloodstream. Insulin causes glucose to move from the blood into cells, where it is either used for respiration or stored in liver and muscle cells as glycogen. The effect of this is to lower the blood glucose concentration back to normal. The animation below shows how this works. You have an old or no version of Flash - you need to upgrade to view this content! Go to the WebWise Flash install guide Diabetes There are two main types of diabetes: Type 1 which usually develops during childhood Type 2 which is usually develops in later life This syllabus focuses on Type 1 diabetes - whic Continue reading >>
How does the body use energy?
All parts of the body (muscles, brain, heart, and liver) need energy to work. This energy comes from the food we eat. Our bodies digest the food we eat by mixing it with fluids (acids and enzymes) in the stomach. When the stomach digests food, the carbohydrate (sugars and starches) in the food breaks down into another type of sugar, called glucose. The stomach and small intestines absorb the glucose and then release it into the bloodstream. Once in the bloodstream, glucose can be used immediately for energy or stored in our bodies, to be used later. However, our bodies need insulin in order to use or store glucose for energy. Without insulin, glucose stays in the bloodstream, keeping blood sugar levels high. Insulin is a hormone made by beta cells in the pancreas. Beta cells are very sensitive to the amount of glucose in the bloodstream. Normally beta cells check the blood's glucose level every few seconds and sense when they need to speed up or slow down the amount of insulin they're making and releasing. When someone eats something high in carbohydrates, like a piece of bread, the glucose level in the blood rises and the beta cells trigger the pancreas to release more insulin into the bloodstream. When insulin is released from the pancreas, it travels through the bloodstream to the body's cells and tells the cell doors to open up to let the glucose in. Once inside, the cells convert glucose into energy to use right then or store it to use later. As glucose moves from the bloodstream into the cells, blood sugar levels start to drop. The beta cells in the pancreas can tell this is happening, so they slow down the amount of insulin they're making. At the same time, the pancreas slows down the amount of insulin that it's releasing into the bloodstream. When this happens, Continue reading >>
Is postprandial blood glucose a predictor of cardiovascular events?
Postprandial Blood Glucose Is a Stronger Predictor of Cardiovascular Events Than Fasting Blood Glucose in Type 2 Diabetes Mellitus, Particularly in Women: Lessons from the San Luigi Gonzaga Diabetes Study
How is glucose absorbed?
Almost 80 percent of these monosaccharides are glucose. Glucose is absorbed in small intestine by absorptive cells. The process of transport of glucose from intestinal lumen into the absorptive cell has two stages. In the first stage sodium ion from inside the cells are transported to interstitial fluid. This leads to low sodium concentration ...
What is the mechanism of absorbing glucose?
Jan 26, 2016. Glucose is absorbed by sodium glucose co-transport mechanism. Blood glucose levels are maintained by liver, insulin, glucagon and some other hormones.
What happens when blood glucose levels drop?
When blood glucose concentration rises too high, insulin is secreted; which decreases the level. Conversely when glucose level drops too low glucagon is secreted and restores it. These two are pancreatic hormones.
Where is glucose stored after a meal?
When after a meal blood glucose rises and insulin is secreted, two thirds of the glucose absorbed from gut is stored in the liver in the form of glycogen. Then during succeeding hours, liver releases glucose back into blood to maintain a narrow range of blood glucose level.
How is sodium ion transported from the intestinal lumen?
As a result of low sodium inside the cells, sodium ions are transported from intestinal lumen by facilitated diffusion (diffusion with the help of transport protein). The transport protein that helps in this case, has a peculiarity.
Where are carbohydrates absorbed?
After carbohydrates are eaten and digested, they are absorbed in the small intestine through a two-step transport system as follows:
What is the mechanism that allows glucose to be released into the blood?
Glucose is released from cells to the interstitial space by a mechanism believed to occur by facilitated diffusion through the glucose transporter-GLUT2 located in the lateral and basement membranes of cells and from there into the blood.
How are blood glucose levels regulated?
The levels of glucose in the blood are controlled by the following mechanisms:
What is the role of sodium dependent glucose transporter (SGLUT1) in the intestine?
The role of the sodium- dependent glucose transporter (SGLUT1) in the intestine is as we mentioned that it transports glucose and galactose to the cells lining the intestinal wall. As for its role in the kidneys, this protein plays a role in maintaining normal blood sugar levels, as it transports glucose to the kidney cells. Specialized, which ensures that sugar returns to the blood and is not released into the urine.
What is the most important form of sugar?
Glucose is a monosaccharide and is one of the most important forms of sugar the body uses for energy. All carbohydrates, including other sugars, are converted into glucose during the digestion of food.
What happens when the stomach digests food?
When the stomach digests food, the carbohydrate (sugars and starches) in the food breaks down into another type of sugar, called glucose. The stomach and small intestines absorb the glucose and then release it into the bloodstream.
What hormones are secreted from the adrenal glands?
In the case of prolonged low glucose , adrenaline , growth hormone, and cortisol are secreted from the adrenal hormones, which leads to the restoration of the normal blood sugar level.
How is glucose absorbed into the bloodstream?
Glucose is a product of carbohydrate digestion, the absorption of which into the blood stream involves two main stages: 1) Diffusion into the blood: When carbohydrates are first broken down, there's a higher concentration of glucose in the small intestine than in the blood, creating a concentration gradient, so glucose moves across the epithelial cells of the small intestine and into the blood by diffusion. When the concentration of glucose in the small intestine lumen is the same as in the blood, diffusion stops. 2) Active transport: The remaining glucose is absorbed by active transport with sodium ions. Step 1 = Sodium ions are actively transported out of the small intestine epithelial cells and into the blood stream by the sodium-potassium pump. This creates a concentration gradient, as there is now a higher concentration of sodium ions in the small intestine lumen than in the epithelial cells. Step 2 = This causes sodium ions to diffuse from the small intestine lumen into the cell down their concentration gradient via a sodium-glucose co-transporter protein, which brings glucose into the cell at the same time. This causes the glucose concentration in the cell to increase. Step 3 = Glucose diffuses out of the cell and into the blood through a protein channel. This is facilitated diffusion.
What is the step 2 of the glucose transporter?
Step 2 = This causes sodium ions to diffuse from the small intestine lumen into the cell down their concentration gradient via a sodium-glucose co-transporter protein, which brings glucose into the cell at the same time.
Which step is the sodium ion transported out of the small intestine?
Step 1 = Sodium ions are actively transported out of the small intestine epithelial cells and into the blood stream by the sodium-potassium pump.
What is the step 3 of diffusion?
This causes the glucose concentration in the cell to increase. Step 3 = Glucose diffuses out of the cell and into the blood through a protein channel. This is facilitated diffusion.
Where Does Glucose Reabsorption Occur?
In order to ensure that valuable molecules like glucose and amino acids aren't excreted together with the waste products, the kidney must reabsorb them, a process that takes place in the proximal tubule. Blood flows into the kidney through the renal artery, which branches and subdivides into smaller vessels to supply blood to the nephrons. The nephrons are the functional units of the kidney that carry out the actual filtration and reabsorption; there are hundreds of thousands of them in adult human kidneys. The blood flows through a ball of capillaries called the glomerulus; here the blood pressure causes water, dissolved salts and small molecules like waste products, amino acids and glucose to leak through the capillaries' walls into a structure called Bowman's capsule. This initial step removes waste products from the blood while preventing the loss of cells like red blood cells or proteins, but it also removes valuable molecules like glucose from the bloodstream. Hence the next step in the process: reabsorption. Reabsorption takes place in the proximal tubule of the nephron, a tube leading out of Bowman's capsule. The cells that line the proximal tubule recapture valuable molecules including, of course, glucose. The mechanism by which they do so is different for different molecules and solutes. For glucose there are two processes involved: the process whereby glucose is reabsorbed across the apical membrane of the cell, meaning the membrane of the cell that faces out onto the proximal tubule, and then the mechan Continue reading >>
How does glucose reabsorb in the kidney?
Renal glucose reabsorption is the part of kidney (renal) physiology that deals with the retrieval of filtered glucose, preventing it from disappearing from the body through the urine. If glucose is not reabsorbed by the kidney, it appears in the urine, in a condition known as glucosuria. This is associated with diabetes mellitus. [1] Firstly, the glucose in the proximal tubule is co-transported with sodium ions into the proximal convoluted tubule walls via the SGLT2 cotransporter. Some (typically smaller) amino acids are also transported in this way. Once in the tubule wall, the glucose and amino acids diffuse directly into the blood capillaries along a concentration gradient. This blood is flowing, so the gradient is maintained. Lastly, sodium/potassium ion active transport pumps remove sodium from the tubule wall and the sodium is put back into the blood. This maintains a sodium concentration gradient in the proximal tubule lining, so the first step continues to happen. Gliflozins such as canagliflozin inhibit renal glucose reabsorption, [2] and are used in diabetes mellitus to lower blood glucose. Overview table Characteristics of glucose reabsorption Characteristic Proximal tubule Loop of Henle Distal convoluted tubule Collecting duct system S1 S2 S3 Reabsorption (%) 98 [3] Beyond the distal convoluted tubule: 2% [3] Reabsorption (mmol/day) Concentration Apical transport proteins SGLT2 [3] SGLT1 [3] Basolateral transport proteins GLUT2 [3] GLUT1 [3] Other reabsorption features Continue reading >>
What is excretion in the kidney?
Excretion is the removal from the body of the waste products of metabolic activities 11.3.2 Draw and label a diagram of the kidney 11.3.3 Annotate a diagram of a glomerulus and associated nephron to show the function of each part The nephron is the functional unit of the kidney and includes: Afferent arteriole: Brings blood to the nephron to be filtered Efferent arteriole: Removes blood from nephron (minus filtered components) Glomerulus: Capillary tuft where filtration occurs Bowman's Capsule: First part of nephron where filtrate is collected Proximal Convoluted Tubule: Where selective reabsorption occurs Loop of Henle: Important for establishing a salt gradient in the medulla Distal Convoluted Tubule: Final site of selective reabsorption Collecting Duct: Feeds into ureter and is where osmoregulation occurs Vasa Recta: Blood network that reabsorbs components from the filtrate 11.3.4 Explain the process of ultrafiltration, including blood pressure, fenestrated blood capillaries and basement membrane Ultrafiltration occurs when hydrostatic pressure forces blood through a semi-permeable membrane, separating blood cells and large proteins from the remainder of the serum Ultrafiltration occurs between the glomerulus and the Bowman's capsule and requires two things to form the filtrate: The glomerulus increases blood pressure by forming narrow branches (which also increases surface area for filtration) This pressure is maintained by a narrow efferent arteriole (relative to the afferent arteriole), which restricts the outflow of blood, keeping pressure high The net pressure gradient in the glomerulus forces blood into the capsule space The basement membrane is a fine mesh that restricts the passage of blood cells and proteins - it is the sole filtration barrier Blood can exi Continue reading >>
How do molecules get reabsorbed?
Once inside the lumen of the nephron, small molecules, such as ions, glucose and amino acids, get reabsorbed from the filtrate: Specialized proteins called transporters are located on the membranes of the various cells of the nephron. These transporters grab the small molecules from the filtrate as it flows by them. Each transporter grabs only one or two types of molecules. For example, glucose is reabsorbed by a transporter that also grabs sodium. Transporters are concentrated in different parts of the nephron. For example, most of the Na transporters are located in the proximal tubule, while fewer ones are spread out through other segments. Some transporters require energy, usually in the form of adenosine triphosphate (active transport), while others don't (passive transport). Water gets reabsorbed passively by osmosis in response to the buildup of reabsorbed Na in spaces between the cells that form the walls of the nephron. Other molecules get reabsorbed passively when they are caught up in the flow of water (solvent drag). Reabsorption of most substances is related to the reabsorption of Na, either directly, via sharing a transporter, or indirectly via solvent drag, which is set up by the reabsorption of Na. This content is not compatible on this device. The reabsorption process is similar to the "fish pond" game that you see in some amusement parks or state fairs. In these games, there is a stream that contains different colored plastic fish with magnets. The children playing the game each have a fishing pole with an attached magnet to catch the fish as they move by. Different colored fish have different prize values associated with them, so some children will be selective and try to grab the colored fish with the highest prize value. Now suppose our nephron is t Continue reading >>
How does the kidney help with glucose homeostasis?
The enormous capacity of the proximal tubular cells to reabsorb the filtered glucose load entirely, utilizing the sodium-glucose co-transporter system (primarily SGLT-2), became the focus of attention. Original studies conducted in experimental animals with the nonspecific SGLT inhibitor phlorizin showed that hyperglycemia after pancreatectomy decreased as a result of forced glycosuria. Subsequently, several compounds with more selective SGLT-2 inhibition properties (second-generation) were developed. Some agents made it into pre-clinical and clinical trials and a few have already been approved for commercial use in the treatment of type 2 diabetes. In general, a 6-month period of therapy with SGLT-2 inhibitors is followed by a mean urinary glucose excretion rate of ~80 g/day accompanied by a decline in fasting and postprandial glucose with average decreases in HgA1C ~1.0%. Concomitant body weight loss and a mild but consistent drop in blood pressure also have been reported. In contrast, transient polyuria, thirst with dehydration and occasional hypotension have been described early in the treatment. In addition, a significant increase in the occurrence of uro-genital infections, particularly in women has been documented with the use of SGLT-2 inhibitors. Although long-term cardiovascular, renal and bone/mineral effects are unknown SGLT-2 inhibitors, if used with caution and in the proper patient provide a unique insulin-independent therapeutic option in th Continue reading >>
Where is sodium reabsorbed in the kidney?
Tubular Reabsorption of Sodium, Chloride and Fluids 99% of the glomerular filtrate volume (primary urine, 120 ml/min), 99% of the filtrated sodium and 99% of the filtered Chloride are reabsorbed in the renal tubules of the nephron. The reabsorption is energy consuming process; the needed energy rises linearly with the NaCl-Reabsorption. The most common drive for the reabsorption is the basolateral located Na-K-ATPase (sodium-potassium pump), which transports three sodium atoms out of the cell and two potassium atoms into the cell, the energy derives from the hydrolysis of one ATP molecule. Proximal Tubule and Descending Part of the Henle Loop In the proximal tubule, two thirds of the primary urine volume with electrolytes are reabsorbed. Electrolyte reabsorption leads to the water reabsorption with help of the leaky intercellular spaces of the proximal tubule epithelium. The solvent drag enables the paracellular absorption of water and chloride due to electrolyte concentrations between the tubule lumen and the renal interstitium. The drive of the sodium transport is accomplished through the basolateral sodium-potassium-pump. On the luminal side of the proximal tubule epithelium, sodium enters the cell via symporter membrane proteins (Co-transport with glucose, galactose, phosphate, sulfate or amino acids) or antiporter membrane proteins (Co-transport with protons). The reabsorption of HCO3 is linked to the sodium reabsorption and proton secretion with help of a luminal and intracellular carbonic anhydrase. The chloride reabsorption is not so clearly identified. Beside the solvent drag, there are additional minor transcellular transport pathways for chloride in the luminal and basolateral membrane. Th Continue reading >>
Where is urine produced?
Urine is produced in microscopic structures in the kidney called nephrons . There are approximately 1 million nephrons in each kidney. The glomerulus filters blood and produces glomerular filtrate. This filtrate contains water, glucose [glucose: A simple sugar made by the body from food, which is used by cells to make energy in respiration.], salts and urea [urea: A nitrogenous waste product resulting from the breakdown of proteins. It is excreted in urine.]. Large molecules such as protein [protein: Organic compound made up of amino acid molecules. One of the three main food groups, proteins are needed by the body for cell growth and repair.] are too large to fit through the blood capillary [capillaries: Extremely narrow tubes, which carry blood around a body's tissues.] walls. The Bowman's capsule collects the filtrate and it enters the tubules. All glucose is reabsorbed immediately into the blood capillaries. As the rest of the filtrate travels through the tubules, water and salts needed by the body are reabsorbed into the blood capillaries. The loop of Henl helps maintain the correct water balance in the body by filtering out salts. The waste, consisting of excess water, excess salts and urea, is urine. The collecting duct collects the urine, which is then transported in the ureter to the bladder. The bladder stores urine until the body is ready to expel it through the urethra. This process can be summarised in three important steps: Filtration - where lots of water, ions [ion: The charged particle formed when an atom, or a group of atoms, lose or gain electrons. Ion charge helps determine a substance's acidity or alkalinity.], urea [urea: A nitrogenous waste product resulting from the breakdown of proteins. It is excreted in urine.] and sugar are squeezed from the Continue reading >>
What cells transport glucose from the intestine to the bloodstream?
Once digestion creates a pool of glucose in intestine, absorptive cells lining in small intestine begin to transport the glucose from intestine to bloodstream.
Where does the transporter molecule move?
The transporter molecule within the enterocyte moves to the cell membrane closest to the intestine and first binds sodium, which changes the shape of the transporter so it can now also grab a single glucose molecule from within intestine