What causes elevated parathyroid hormone levels?
- A noncancerous growth (adenoma) on a gland is the most common cause.
- Enlargement (hyperplasia) of two or more parathyroid glands accounts for most other cases.
- A cancerous tumor is a very rare cause of primary hyperparathyroidism.
What causes elevated parathyroid levels?
High parathyroid hormone (PTH) levels are primarily caused by hyperparathyroidism, which happens when your parathyroid glands are overactive and release too much PTH. In the United States, about 100,000 people develop hyperparathyroidism each year.
What type of hormone do the parathyroid glands produce?
- Bones: Parathyroid hormone stimulates the release of small amounts of calcium from your bones into your bloodstream.
- Kidneys: Parathyroid hormone enables the production of active vitamin D (calcitriol) in your kidneys. ...
- Small intestine: Parathyroid hormone signals your small intestine to absorb more calcium from the food you eat.
What are the signs of parathyroid problems?
Parathyroid Disease Symptoms. A lump in the neck. Difficulty speaking or swallowing. Muscle weakness. Sudden increase in blood calcium levels (hypercalcemia) Fatigue, drowsiness. Urinating more than usual, which may cause you to be dehydrated and very thirsty. Bone pain and broken bones. Kidney stones.

Where do parathyroid hormones come from?
Parathyroid hormone comes from four parathyroid glands in the neck, just behind the thyroid. These glands receive feedback from blood calcium levels to determine when they need to secrete the hormone.
How is parathyroid hormone released?
Parathyroid hormone (PTH) levels are mainly controlled by a feedback loop of calcium levels in your blood to your parathyroid glands. In other words, low calcium levels in your blood stimulate parathyroid hormone release, whereas high calcium levels in your blood prevent your glands from releasing parathyroid hormone.
What gland releases parathyroid hormone?
Function of the parathyroid glands Parathyroid glands produce parathyroid hormone, which plays a key role in the regulation of calcium levels in the blood. Precise calcium levels are important in the human body, since small changes can cause muscle and nerve problems.
When is parathyroid released?
If calcium blood levels are too low, your parathyroid glands will release PTH into the blood. This causes calcium levels to rise. If calcium blood levels are too high, these glands will stop making PTH. PTH levels that are too high or too low can cause serious health problems.
What triggers the release of parathyroid hormone quizlet?
PTH is released when blood calcium levels fall below its set point and it causes bone to release calcium and stimulates formation of vitamin D hormone (calcitriol) in the kidneys, which promotes calcium absorption from the GI tract.
Is parathyroid hormone regulated by the pituitary gland?
The parathyroid gland and adrenal medulla are not controlled by the pituitary but play important roles in calcium metabolism and the adrenergic (sympathetic nervous system) function respectively.
What are the 4 parathyroid glands?
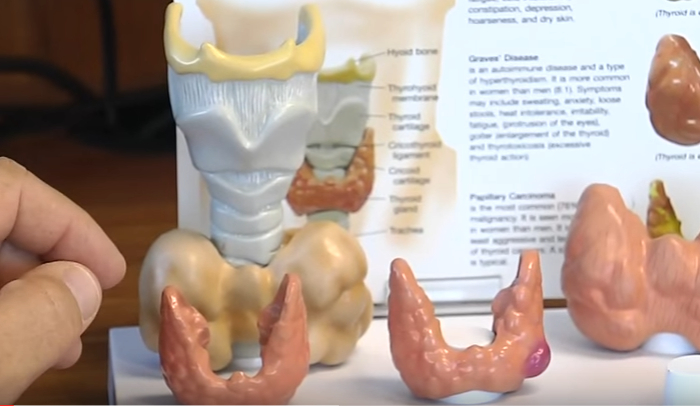
What are Parathyroid Glands? Parathyroid glands are four small glands of the endocrine system which regulate the calcium in our bodies. Parathyroid glands are located in the neck behind the thyroid where they continuously monitor and regulate blood calcium levels.
What 4 glands are in your neck?
The parathyroid glands are small pea-sized glands located in the neck just behind the butterfly-shaped thyroid gland. Most people have four parathyroid glands, with two parathyroid glands lying behind each 'wing' of the thyroid gland.
Is the parathyroid part of the thyroid?
Parathyroid Glands: Essentials Parathyroid hormone regulates the body's calcium levels. There are four parathyroid glands, and they are each about the size of a grain of rice. Though they're located near each other, the parathyroid glands are not related to the thyroid gland.
What does parathyroid hormone do to calcium?
Parathyroid hormone is directly involved in the bones, kidneys, and small intestine. In the bones, PTH stimulates the release of calcium in an indirect process through osteoclasts which ultimately leads to resorption of the bones.
What does parathyroid hormone do to bone?
The aim of this review is to focus on the roles of PTH in bone remodeling. PTH plays a central role in regulating calcium-phosphate metabolism and its production increases in response to low serum calcium levels. A continue hypersecretion of PTH, as occurs in primary hyperparathyroidism, leads to bone resorption.
What stimulation controls parathyroid release?
What type of stimulation controls parathyroid release? The parathyroid is stimulated by the actual level of calcium in the blood rather than by neural or hormonal stimulus.
What causes calcitriol to be released?
Renal production of calcitriol is stimulated in response to PTH, low calcium and low phosphate 4.
What stimulates the secretion of parathyroid hormone from the parathyroid gland quizlet?
What stimulates the secretion of parathyroid hormone from the parathyroid gland? Parathyroid hormone is produced in response to a low blood calcium level.
What stimulates the release of calcitriol?
Parathyroid hormone stimulates calcitriol production in the kidney by increasing the synthesis of 1-α hydroxylase. Calcitriol has several important functions in the body. It maintains serum calcium levels by increasing calcium absorption in the gastrointestinal tract.
How is the secretion of parathyroid hormone determined?
Secretion of parathyroid hormone is determined chiefly by serum ionized calcium concentration through negative feedback. Parathyroid cells express calcium-sensing receptors on the cell surface. PTH is secreted when [Ca 2+] is decreased (calcitonin is secreted when serum calcium levels are elevated). The G-protein-coupled calcium receptors bind extracellular calcium and may be found on the surface on a wide variety of cells distributed in the brain, heart, skin, stomach, C cells, and other tissues. In the parathyroid gland, high concentrations of extracellular calcium result in activation of the Gq G-protein coupled cascade through the action of phospholipase C. This hydrolyzes phosphatidylinositol 4,5-bisphosphate (PIP2) to liberate intracellular messengers IP3 and diacylglycerol (DAG). Ultimately, these two messengers result in a release of calcium from intracellular stores into the cytoplasmic space. Hence a high extracellular calcium concentration leads to an increase in the cytoplasmic calcium concentration. In contrast to the mechanism that most secretory cells use, this high cytoplasmic calcium concentration inhibits the fusion of vesicles containing granules of preformed PTH with the membrane of the parathyroid cell, and thus inhibits release of PTH.
What is the function of the parathyroid glands?
Parathyroid hormone ( PTH ), also called parathormone or parathyrin, is a hormone secreted by the parathyroid glands that regulates the serum calcium concentration through its effects on bone, kidney, and intestine. PTH influences bone remodeling, which is an ongoing process in which bone tissue is alternately ...
How does PTH work?
PTH is secreted in response to low blood serum calcium (Ca 2+) levels . PTH indirectly stimulates osteo clast activity within the bone matrix ( osteon ), in an effort to release more ionic calcium (Ca 2+) into the blood to elevate a low serum calcium level. The bones act as a (metaphorical) " bank of calcium" from which the body can make ...
What is the function of PTH in the body?
PTH is "a key that unlocks the bank vault" to remove the calcium.
What is the main determinant of the amount of calcium excreted into the urine per day?
The main determinant of the amount of calcium excreted into the urine per day is the plasma ionized calcium concentration itself . The plasma parathyroid hormone (PTH) concentration only increases or decreases the amount of calcium excreted at any specified plasma ionized calcium concentration.
What hormone is used to treat osteoporotic women?
In osteoporotic women, administration of an exogenous parathyroid hormone analogue ( teriparatide, by daily injection) superimposed on estrogen therapy produced increases in bone mass and reduced vertebral and nonvertebral fractures by 45 to 65%.
What is the difference between hyperparathyroidism and hypoparathyroidism?
Primary hyperparathyroidism is due to autonomous, abnormal hypersecretion of PTH from the parathyroid gland, while secondary hyperparathyroidism is an appropriately high PTH level seen as a physiological response to hypocalcaemia. A low level of PTH in the blood is known as hypoparathyroidism and is most commonly due to damage to or removal of parathyroid glands during thyroid surgery.
What is parathyroid hormone?
The parathyroid glands are located in the neck, just behind the butterfly-shaped thyroid gland.
How is parathyroid hormone controlled?
Parathyroid hormone is mainly controlled by the negative feedback of calcium levels in the blood to the parathyroid glands . Low calcium levels in the blood stimulate parathyroid hormone secretion, whereas high calcium levels in the blood prevent the release of parathyroid hormone.
What happens if I have too much parathyroid hormone?
A primary problem in the parathyroid glands, producing too much parathyroid hormone causes raised calcium levels in the blood ( hypercalcaemia) and this is referred to as primary hyperparathyroidism. There is a similar but much rarer condition called tertiary hyperparathyroidism that causes hypercalcaemia due to excess parathyroid hormone production on the back drop of all four glands being overactive. Secondary hyperparathyroidism occurs in response to low blood calcium levels and is caused by other mechanisms, for example, kidney disease and vitamin D deficiency.
What hormones increase bone formation?
Bones – parathyroid hormone stimulates the release of calcium from large calcium stores in the bones into the bloodstream. This increases bone destruction and decreases the formation of new bone. Kidneys – parathyroid hormone reduces loss of calcium in urine.
What causes hyperparathyroidism?
Secondary hyperparathyroidism occurs in response to low blood calcium levels and is caused by other mechanisms, for example, kidney disease and vitamin D deficiency. Mild primary hyperparathyroidism often causes few if any symptoms and is frequently diagnosed by finding a high calcium concentration on a routine blood test.
Does parathyroid hormone affect the kidneys?
Parathyroid hormone also stimulates the production of active vitamin D in the kidneys. Intestine – parathyroid hormone indirectly increases calcium absorption from food in the intestine, via its effects on vitamin D metabolism.
Can parathyroidism cause low calcium levels?
It can result in low levels of calcium in the blood ( hypocalcaemia ). It is usually treated medically with oral calcium and vitamin D analogues but the availability of parathyroid hormone replacement therapy may change the approach to treatment for some patients. Last reviewed: Feb 2018. Prev.
What hormones are involved in the secretion of parathyroid hormone?
Parathyroid hormone (PTH) secretion is regulated by a complex interplay of circulating minerals and hormones that include extracellular calcium (via the calcium-sensing receptor, CaSR), plasma phosphate, 1,25-dihydroxyvitamin D (1,25 (OH)2D), and fibroblast growth factor 23 (FGF23) . The most common causes of secondary hyperparathyroidism are renal disease and vitamin D deficiency. Although less common, other conditions that cause secondary hyperparathyroidism include disorders of calcium balance (deficiency, malabsorption, and excess excretion), disorders associated with FGF23 excess, persistent parathyroid disease after renal transplant, specific disorders of acid–base balance, and ingestion of certain medications.
What is the relationship between parathyroid hormone and calcitonin?
Figure 30.2. Relationship between parathyroid hormone (PTH) and calcitonin (CT) secretion and ionized calcium concentration. PTH and CT secretion are normalized to percent of maximum. The dashed line shows half-maximal secretion, which occurs at ∼1.2 mM Ca 2+. This is referred to as the set point. PTH secretion increases to defend calcium homeostasis. Conversely, as calcium levels rise, PTH secretion is inhibited, while release of CT increases.
How does calcium affect PTH secretion?
A reduction in serum calcium reduces extracellular calcium transflux and thus stimulates PTH secretion by reducing parathyroid cell calcium. A molecule that is antagonistic to the CaR receptor pathway, therefore, should be associated with an increase in PTH secretion. In mouse models of postmenopausal osteoporosis, CaR antagonists increase PTH secretion and BMD [82].
How is PTH secretion regulated?
PTH secretion is tightly regulated by changes of extracellular calcium12 through a negative-feedback mechanism that is primarily mediated by the calcium-sensing receptor (CaSR), a family C G protein–coupled receptor (GPCR) on parathyroid cells. Reductions of serum ionized calcium stimulate PTH secretion, whereas increases ...
How does PTH affect the kidney?
Pi released from bone complexes Ca 2+ and thus prevents the free plasma [Ca 2+] from rising as much as it would in the absence of the increased Pi. PTH causes the kidney to retain more of the filtered Ca 2+ and dispose of the Pi. Thus there is a hyperphosphaturia and more of the Ca 2+ that is resorbed from bone is retained in the blood. Because PTH can raise the filtered load of Ca 2+, the effect of PTH can be either a hypocalciuria or hypercalciuria, depending on the balance of PTH effects on bone resorption and kidney reabsorption of Ca2+. Further, PTH stimulates the kidney 1α hydroxylase to increase production of 1,25 (OH) 2 D, which stimulates Ca 2+ and Pi absorption from the intestine. The net effect of PTH secreted in response to hypocalcemia is generally not hypophosphatemia because it increases Pi input into the plasma at the same time that it increases Pi output from the plasma.
What is the regulation of PTH secretion?
The regulation of PTH secretion by calcium is an example of unusually precise cellular control. A decrease of a few per cent in serum calcium concentration (experimentally induced) elicits a nearly instantaneous response in PTH secretion, with the hormone concentration rising twofold or more.
What is the cause of secondary hyperparathyroidism?
Secondary hyperparathyroidism is found when PTH is elevated as an adaptive response to depressed serum calcium, decreased 1,25-dihydroxyvitamin D [1,25 (OH)2D] or 25-hydroxyvitamin D [25 (OH)D] concentrations (in the context of vitamin D deficiency or renal failure), poor calcium intake, excessive renal calcium losses or hyperphosphatemia (especially in the context of renal failure). With prolonged secondary hyperparathyroidism, the parathyroid glands can respond by enlarging and starting to autonomously produce PTH, a condition known as tertiary hyperparathyroidism.
What hormone is secreted by the parathyroid gland?
The parathyroid gland secretes parathyroid hormone (PTH), a polypeptide, in response to low calcium levels detected in the blood. PTH facilitates the synthesis of active vitamin D, calcitriol (1,25-dihydroxycholecalciferol, or vitamin D3) in the kidneys.
How is parathyroid hormone synthesized?
Parathyroid hormone is a polypeptide that is synthesized and cleaved into an active form within the parathyroid gland. The initial structure formed is a pre-pro-PTH, a 115 amino acid polypeptide that is cleaved to form pro-PTH comprised of 90 amino acids. It is then cleaved a second time, again at the amino-terminal portion, to form active parathyroid hormone comprised of 84 amino acids. This is the primary hormone that is stored, secreted, and functions in the body. The process of synthesis, cleavage, and storage is estimated to take less than an hour. Active PTH secretion can occur as quickly as a few seconds when low serum calcium is detected. The mechanism of secretion is via exocytosis, a process where the hormone is released through a membrane vesicle carried to the cell membrane, releasing the hormone after the vesicle fuses with the outer membrane. The serum half-life of activated PTH is a few minutes and is removed from the serum quickly by the kidney and liver. [5][6]
Why do I have hypoparathyroidism?
Hypoparathyroidism doesn't occur with the same frequency as an overactive gland and can also vary in duration. Hypoparathyroidism can be chronic, or it can resolve transiently. Most commonly, a person becomes hypo-parathyroid when their parathyroid gland is removed with elective surgery, or it is damaged iatrogenically during a thyroid resection procedure due to the close anatomical proximity. The next most common cause of the underproduction of PTH is associated with autoimmune disorders causing the destruction or damaging the glands individually or collectively. This can be found in Autoimmune polyendocrine syndrome type I. Autoimmune polyendocrine syndrome type I is due to mutation of the autoimmune regulatory (AIRE) gene and is characterized by the triad chronic mucocutaneous candidiasis, hypoparathyroidism, and Addison disease. Another cause of hypoparathyroidism is due to failure of embryological formation of the parathyroid glands. DiGeorge syndrome is a condition due to chromosomal 22q11 deletion and is characterized by the failure of the formation of the 3rd and 4th pharyngeal pouches, which are responsible for the embryological formation of the thymus and parathyroid gland. Manifestations of DiGeorge syndrome are chronic infections (due to lack of mature T lymphocyte proliferation in an absent thymus), hypoparathyroidism, cleft lip/palate, congenital cardiac defects (i.e., persistent truncus arteriosus, tetralogy of Fallot, or ventricular septal defect), and craniofacial abnormalities. [12][13]
What is the function of the parathyroid gland?
In the blood, the sensitive process of calcium and phosphate homeostasis is maintained primarily by an appropriately functioning parathyroid gland. The parathyroid gland is comprised of 4 small glands located posteriorly to the thyroid in the middle aspect of the anterior neck. The parathyroid gland secretes parathyroid hormone (PTH), a polypeptide, in response to low calcium levels detected in the blood. PTH facilitates the synthesis of active vitamin D, calcitriol (1,25-dihydroxycholecalciferol, or vitamin D3) in the kidneys. In conjunction with calcitriol, PTH regulates calcium and phosphate. PTH effects are present in the bones, kidneys, and small intestines. As serum calcium levels drop, the secretion of PTH by the parathyroid gland increases. Increased calcium levels in the serum serve as a negative-feedback loop signaling the parathyroid glands to stop the release of PTH. The mechanism of PTH in the body is intricate, and the clinical ramifications of irregularities are significant. The understanding of PTH is of paramount relevance and importance.[1][2][3][4]
Why is my parathyroid gland not producing enough PTH?
If hypocalcemia and low levels of PTH characterize the clinical scenario, then the concern is that the parathyroid glands are not producing enough PTH. Hypoparathyroidism can be caused by a variety of different conditions and can manifest in various ways. The underproduction of PTH can be chronic or transient, depending on the etiology. More common causes of hypoparathyroidism are the autoimmune destruction of the gland, damage during thyroid resections, or severe illnesses. Each of those conditions would need to be investigated further.
How long does it take for parathyroid hormone to cleave?
The process of synthesis, cleavage, and storage is estimated to take less than an hour.
Which organ system is directly involved in the release of calcium?
Organ Systems Involved. Parathyroid hormone is directly involved in the bones, kidneys, and small intestine. Effects of PTH in the Bones. In the bones, PTH stimulates the release of calcium in an indirect process through osteoclasts which ultimately lead to resorption of the bones.
What if the parathyroid hormone is too high?
Too much Parathyroid hormone causes higher calcium levels in the blood which leads to a disease known as hyperparathyroidism.
Which hormones are present next to the thyroid gland and have no concerned function?
Parathyroids also manage the amount of calcium in the bones and determine their strongness. However, these glands are present next to the thyroid gland and have no concerned function. Bones – The parathyroid hormone (PTH) stimulates the release of calcium from stores of calcium present in the bones into the bloodstreams.
What hormone controls calcium levels in the blood?
Parathyroid hormone controls and regulates the levels of calcium in the blood and raise their levels when they are too low. This gland performs its function through its actions on the bones, intestine, and the kidneys. There are two main types of Parathyroid hormone : Parathormone. Calcitonin.
What happens when your parathyroid is low?
It is treated medically with vitamin D analogues and oral calcium supplements. When the calcium level falls down people get tingling sensation or cramps in the hand muscles.
Why is calcium high in hyperparathyroidism?
It is of three types. In primary and tertiary hyperparathyroidism, the level of calcium is high due to excessive secretion of parathyroid hormone. In secondary hyperparathyroidism, the level of calcium is low due to other factors like kidney disease.
Does PTH increase calcium absorption?
Intestine – PTH increases the calcium absorption in the intestine by food through its impacts and effects on the metabolism of vitamin D. Kidneys – PTH minimizes the calcium loss in the urine and also stimulates active vitamin D formation in the kidneys.
What is the role of parathyroid?
The parathyroid plays a vital role in regulating and balancing both calcium and phosphorus in your bones and blood.
Why do we need to see parathyroid cells?
Having images showing specific accumulation of parathyroid cells allows healthcare providers to see where the cancer cells are clustering. This information not only shows if the cancer is spreading, but it can also identify which of the four parathyroid glands are affected by cancer.
Why does hypoparathyroidism occur?
Hypoparathyroidism occurs when the parathyroid isn't acting to maintain levels of blood calcium. This affects the body's muscles and nerves, among other things. Hypoparathyroidism can occur if the parathyroid glands are malfunctioning or if the kidneys and bones are not correctly registering the presence of PTH.
What hormone is used to control calcium in the blood?
In order to manage the amount of these minerals, the parathyroid uses the parathyroid hormone (PTH). If there is an imbalance of calcium in the bloodstream, the parathyroid will either stop or increase the parathyroid hormone production.
How many parathyroid glands are there in the neck?
The parathyroid consists of four individual glands in the neck. These glands vary in size from one person to another. However, a healthy parathyroid gland will be somewhere between the size of a grain of rice and a pea.
What happens when the parathyroid gland detects too much calcium?
If the parathyroid detects too much calcium, it will stop producing the hormone. When the calcium levels get too low, the parathyroid will release PTH. Parathyroid hormone release triggers the body to release some of the calcium our body has stored in our bones. The bones will release this calcium into the bloodstream.
How to tell if someone has parathyroidism?
When determining if someone has a parathyroid disorder, a healthcare provider will request a series of lab tests. Most often, they will be looking for the presence of PTH and calcium levels in your blood. 5
Where are the parathyroid glands located?
Click image to enlarge. The parathyroid glands are two pairs of small, oval-shaped glands. They are located next to the two thyroid gland lobes in the neck. Each gland is usually about the size of a pea.
Which organs are responsible for absorbing calcium from the intestines?
Conservation of calcium by the kidneys. Stimulates cells in the kidney to transforms weaker forms of vitamin D into the form that is strongest at absorbing calcium from the intestines.
Where is the parathyroid gland located?
These glands, located behind the thyroid at the bottom of your neck , are about the size of a grain of rice. The parathyroid glands produce parathyroid hormone. This hormone helps maintain an appropriate balance of calcium in the bloodstream and in tissues that depend on calcium for proper functioning. Two types of hyperparathyroidism exist.
What is the role of the parathyroid glands in the body?
The parathyroid glands, which lie behind the thyroid, manufacture the parathyroid hormone, which plays a role in regulating your body's levels of the minerals calcium and phosphorus. Hyperparathyroidism is when your parathyroid glands create too much parathyroid hormone in the bloodstream.
How does the parathyroid gland regulate calcium?
The parathyroid glands maintain proper levels of both calcium and phosphorus in your body by turning the secretion of parathyroid hormone (PTH) off or on , much like a thermostat controls a heating system to maintain a constant air temperature. Vitamin D also is involved in regulating the amount of calcium in your blood.
Why is my parathyroid gland not getting enough calcium?
Your body may not get enough calcium from your diet, often because your digestive system doesn't absorb the calcium from it.
Why is hyperparathyroidism common?
Primary hyperparathyroidism occurs because of some problem with one or more of the four parathyroid glands: A noncancerous growth (adenoma) on a gland is the most common cause. Enlargement (hyperplasia) of two or more parathyroid glands accounts for most other cases.
What minerals are involved in hyperparathyroidism?
Phosphorus, another mineral, works along with calcium in these areas. Hyperparathyroidism may occur because of a problem with the parathyroid glands (primary hyperparathyroidism) or because of another disease that affects the glands' function (secondary hyperparathyroidism).
What are the two types of hyperparathyroidism?
Two types of hyperparathyroidism exist. In primary hyperparathyroidism, an enlargement of one or more of the parathyroid glands causes overproduction of the hormone. This causes high calcium levels in the blood, which can cause a variety of health problems. Surgery is the most common treatment for primary hyperparathyroidism.

Overview
Function
Parathyroid hormone regulates serum calcium through its effects on bone, kidney, and the intestine:
In bone, PTH enhances the release of calcium from the large reservoir contained in the bones. Bone resorption is the normal destruction of bone by osteoclasts, which are indirectly stimulated by PTH. Stimulation is indirect since osteoclast…
Structure
hPTH-(1-84) crystallizes as a slightly bent, long, helical dimer. The extended helical conformation of hPTH-(1-84) is the likely bioactive conformation. The N-terminal fragment 1-34 of parathyroid hormone (PTH) has been crystallized and the structure has been refined to 0.9 Å resolution.
Regulation of PTH secretion
Secretion of parathyroid hormone is determined chiefly by serum ionized calcium concentration through negative feedback. Parathyroid cells express calcium-sensing receptors on the cell surface. PTH is secreted when [Ca ] is decreased (calcitonin is secreted when serum calcium levels are elevated). The G-protein-coupled calcium receptors bind extracellular calcium and may be found on the surface on a wide variety of cells distributed in the brain, heart, skin, stomach, C c…
Disorders
Hyperparathyroidism, the presence of excessive amounts of parathyroid hormone in the blood, occurs in two very distinct sets of circumstances. Primary hyperparathyroidism is due to autonomous, abnormal hypersecretion of PTH from the parathyroid gland, while secondary hyperparathyroidism is an appropriately high PTH level seen as a physiological response to hypocalcemia. A low level of PTH in the blood is known as hypoparathyroidism and is most com…
Measurement
PTH can be measured in the blood in several different forms: intact PTH; N-terminal PTH; mid-molecule PTH, and C-terminal PTH, and different tests are used in different clinical situations. The level may be stated in pg/dL or pmol/L (sometimes abbreviated mmol/L); multiply by 0.1060 to convert from pg/dL to pmol/L.
A US source states the average PTH level to be 8–51 pg/mL. In the UK the biological reference ra…
See also
• Disorders of calcium metabolism
• Parathyroid hormone family
• Parathyroid hormone-related protein
• Preotact
Further reading
• Drüeke TB, Massy ZA (2003). "Advanced oxidation protein products, parathyroid hormone and vascular calcification in uremia". Blood Purification. 20 (5): 494–7. doi:10.1159/000065203. PMID 12207101. S2CID 46752152.
• Parfitt AM (Oct 2002). "Parathyroid hormone and periosteal bone expansion". Journal of Bone and Mineral Research. 17 (10): 1741–3. doi:10.1359/jbmr.2002.17.10.1741. PMID 12369776. S2CID 37111637.