Antivirals
- Acyclovir (only nephrotoxic in intravenous form)
- Adefovir
- Cidofovir
- Foscarnet
- Indinavir
- Tenofovir
Which antibiotics are most associated with encephalopathy?
Results
- Aminoglycosides. ...
- Cephalosporins. ...
- Penicillins. ...
- Other beta-lactams: carbapenems. ...
- Tetracyclines. ...
- Trimethoprim/sulfonamides. ...
- Macrolides/azalides. ...
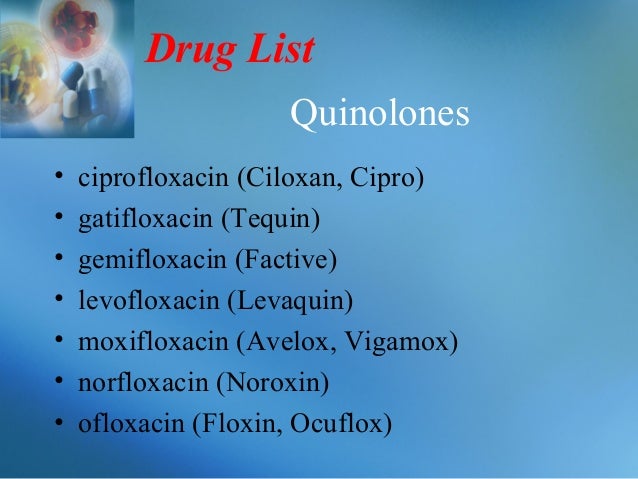
- Quinolones. ...
- Oxazolidinones. ...
- Streptogramins. ...
Is there any alternative for antibiotics?
- Bactroban
- Nitrofurazone
- Nystatin (mentioned above for denture stomatitis)
- Silvadene
- Sulfamylon
What antibiotics are used for oral infections?
Top 10 List of Generic Antibiotics
- amoxicillin
- doxycycline
- cephalexin
- ciprofloxacin
- clindamycin
- metronidazole
- azithromycin
- sulfamethoxazole and trimethoprim
- amoxicillin and clavulanate
- levofloxacin
What are the symptoms of antibiotics?
What are the signs and symptoms of an allergic reaction to an antibiotic?
- Mild symptoms include red, itchy, flaky, or swollen skin. You may have a flat, red area on your skin that is covered with small bumps. ...
- Severe symptoms include skin that blisters or peels, vision problems, and severe swelling or itching. ...
- Anaphylaxis symptoms include throat tightness, trouble breathing, tingling, dizziness, and wheezing. ...

Which antibiotics damage kidneys?
Aminoglycoside antibiotics are known for causing kidney injury—even at low doses. People with chronic kidney disease, dehydration, or those who have been taking these antibiotics for a long time are at particularly high risk. The most toxic aminoglycoside is neomycin, followed by gentamicin, tobramycin, and amikacin.
Which medications are nephrotoxic?
Drugs most often associated with this pathogenic mechanism of nephrotoxicity include antiplatelet agents (e.g., clopidogrel [Plavix], ticlopidine [Ticlid]), cyclosporine, mitomycin-C (Mutamycin), and quinine (Qualaquin).
Which antibiotic is least nephrotoxic?
In general, appropriately dosed vancomycin in noncritically ill patients for the treatment of less serious infections has minimal risk of nephrotoxicity (13).
Which antibiotic should be avoided in renal disease patients?
Table 3ClassDrugContraindicated or to be avoided if possible when:AntibioticsCefepimeGFR <30Phase-prophylactic psychotropic drugsLithiumGFR <60Antidiabetic drugsGlibenclamide, gimepirideGFR <60MetforminGFR <605 more rows•Sep 17, 2010
Does amoxicillin cause nephrotoxicity?
Conclusions: Although renal toxicity may occur with amoxicillin ingestions, it is rare and does not seem to be dose related.
Does amoxicillin affect kidney?
Amoxicillin (AMX) has been associated with acute kidney injury (AKI). Two distinct mechanisms have been described: acute interstitial nephritis and crystal nephropathy, the latter of which has been the primary focus of anecdotal reports.
What are the most common nephrotoxic drugs?
The most common drugs that cause DIKD include antibiotics, anti-rejection medications, antiviral agents, non-steroidal anti-inflammatory agents, anti-ulcer agents and chemotherapy. Most studies have defined nephrotoxicity as 0.5 mg/dL or 50% rise in Scr over 24–72 h time frame and a minimum 24–48 h of drug exposure.
Is ciprofloxacin nephrotoxic?
Nephrotoxic reactions to ciprofloxacin appear to be unusual but potentially serious. It has previously been reported that fluoroquinolones could cause acute renal failure (ARF) after the ingestion of large quantities, but it is now recognized that therapeutic doses of fluoroquinolones can also cause renal injury.
Is ciprofloxacin safe in kidney disease?
In SK patients, renal tubular biomarkers, especially NAG, allow monitoring of tubular injury and impose caution in prescribing ciprofloxacin treatment, mainly to patients at risk. Ciprofloxacin is relatively safe regarding its nephrotoxicity, while caution is required in vulnerable patients.
Is Augmentin safe in renal failure?
Augmentin (Amoxicillin and Clavulanate) can be taken in patient with chronic kidney disease (CKD) and an estimated glomerular filtration rate (eGFR) of 39 milliliters per minute per 1.73 meters squared. The dose is often reduced in patients with an eGFR of 39.
Is azithromycin safe in kidney disease?
Azithromycin is excreted in bile and then faeces. Unlike clarithromycin, very little unchanged azithromycin appears in the urine, and there are no biologically active metabolites. Thus, azithromycin dosing modification is not needed in patients with kidney disease.
Is levofloxacin safe in CKD?
Since levofloxacin is excreted mainly by the kidneys, the dose of Levofloxacin Tablets should be adjusted in patients with renal impairment.
Is Ibuprofen a nephrotoxic drug?
Mechanisms of Ibuprofen- and APAP-Related Kidney Injury Ibuprofen produces nephrotoxicity in three ways. One is the direct toxicity to the kidney. The second is secondary renal damage caused by the deposition of antigen-antibody complexes (Ag-Ab complexes) formed by ibuprofen on the glomeruli.
Are NSAIDs nephrotoxic?
Non-steroidal anti-inflammatory drugs (NSAIDs) are commonly used medications associated with nephrotoxicity, especially when used chronically. Factors such as advanced age and comorbidities, which in themselves already lead to a decrease in glomerular filtration rate, increase the risk of NSAID-related nephrotoxicity.
Is omeprazole nephrotoxic?
Recent clinical data point to a subtle nephrotoxic effect of omeprazole, but the cellular and molecular mechanisms are unknown. Now, we have observed that omeprazole directly induces cell death in cultured tubular renal cells in vivo e in vitro through the generation of oxidative stress-induced cell death.
Is aspirin a nephrotoxic drug?
Aspirin is defined as a nephrotoxic drug while the renal safety of edaravone is controversial. We aimed to evaluate whether edaravone will increase the nephrotoxicity of aspirin in patients with ischaemic stroke.
What are the risk factors for antimicrobial induced AKI?
General risk factors for antimicrobial-induced AKI include pre-existing chronic kidney disease, and concomitant use of medication with nephrotoxic potential. Prevention and early recognition of AKI represent the standard approach to mitigate AKI and avoid morbidity.
What causes acute kidney injury?
Medication-induced nephrotoxicity remains one of the most common causes of acute kidney injury (AKI) among hospitalized patients. Within the extensive group of medications associated with AKI, antibiotics and other antimicrobials are well recognized triggers of structural and functional renal impairment. Clinical manifestations range ...
Can antibiotics cause nephrotoxicity?
Nephrotoxicity of Antimicrobials and Antibiotics. Medication-induced nephrotoxicity remains one of the most common causes of acute kidney injury (AKI) among hospitalized patients. Within the extensive group of medications associated with AKI, antibiotics and other antimicrobials are well recognized triggers of structural ...
Which antibiotics are nephrotoxic?
T he potentially nephrotoxic antibiotics in current clinical use are neomycin, kanamycin, paromomycin, bacitracin, the polymyxins (polymyxin B, and colistin), and amphotericin B. 1-3 Nephrotoxicity was reported with early lots of streptomycin, but the drug now commercially available does not appear to have this property.
What is a tetracycline?
Tetracyclines.— A primary renal toxic effect of undegraded
What medications can cause kidney problems?
And so, make sure to only take medication prescribed by your healthcare provider and respect the recommended dose. 1. Antibiotics. Including: ciprofloxacin, met hicillin, vancomycin , aminoglycosides, cephalosporins, amphotericin B, bacitracin, and sulfonamides.
What are the drugs that are used to treat HIV?
Antiviral Drugs. Including: acyclovir (Zovirax), used to treat herpes infection, and indinavir, ritonavir, and tenofovir, all used to treat HIV. 6. High Blood Pressure Drugs. Including: captopril (Capoten), lisinopril, ramipril, and angiotensin receptor blockers like candesartan and valsartan.
Can drugs cause kidney failure?
In part, drugs can cause kidney inflammation, which can lead to fibrosis and renal scarring, and thus, kidney failure.
Where does nephrotoxicity occur?
Nephrotoxicity occurs once the aminoglycoside is freely filtered by the glomerular filtration barrier and is reabsorbed in the S1 and S2 segments of the proximal renal tubule. The aminoglycoside enters the cytosol and accumulates in organelles such as the mitochondria, Golgi complex, and the nucleus.
What are the side effects of nephrotoxicity?
Side effects including nephrotoxicity and drug interactions are fairly common given the high concentration achieved in the kidney. Drugs cause approximately 20%-40% of acute kidney injury (AKI), perhaps as high as 60% of AKI in the elderly population. 1 Aminoglycosides and beta-lactams are considered the most common antimicrobials causing AKI ...
What causes acute kidney injury?
Medication-induced nephrotoxicity remains one of the most common causes of acute kidney injury (AKI) among hospitalized patients. Within the extensive group of medications associated with AKI, antibiotics and other antimicrobials are well recognized triggers of structural and functional renal impairment. Clinical manifestations range ...
What is acyclovir in urine?
Acyclovir is a potent inhibitor agent for the replication of the herpes virus group. Acyclovir inhibits the viral DNA polymerase, once the drug has been converted into an active triphosphate form - acyclovir triphosphate (Acyclo-GTP). Sixty to ninety percent of acyclovir is eliminated in the urine with no prior hepatic metabolism. Acyclovir clearance is greater than creatinine clearance indicating active tubular secretion as part of the excretory process. Similar to indinavir, acyclovir has low urine solubility promoting drug crystallization in kidney tubules. Crystal formation occurs within 24-48 hours of acyclovir administration with an estimated prevalence of 12%-48% described by 3 large series. 19, 20 Needle shape crystals may be identified under polarizing light microscopy, in combination with hematuria and pyuria. Direct tubular cytotoxicity to the tubular cells with subsequent interstitial nephritis has been described, in the absence of crystalluria. Specific risk factors for crystal formation include rapid intravenous infusion and higher doses (>1500 mg/m 2 ).
What are the risk factors for antimicrobial-induced AKI?
General risk factors for antimicrobial-induced AKI include pre-existing chronic kidney disease, and concomitant use of medication with nephrotoxic potential. Prevention and early recognition of AKI represent the standard approach to mitigate AKI and avoid morbidity. Previous article. in issue.
How does renal tubular toxicity occur?
Renal tubular toxicity might be explained by increased intracellular drug concentration, following influx through the family of organic anion transporters, or decreased excretion by the multidrug resistance-associated protein transporters in the proximal tubule. 2, 3 Genetic polymorphisms in these transporters predispose to renal injury after exposure to certain antimicrobials. If the exposure endures, programmed cell death or apoptosis harmonious with immune-mediated injury destroys cells by the mitogen-activated protein kinase pathway, promoting ATN. 4 In addition, mitochondrial injury through phosphorylation by several antimicrobials leads to oxidative stress, with ensuing anaerobic metabolism, lactic acidosis, and triglyceride accumulation. The presence of reactive oxygen species further disrupts the mitochondrial DNA.
How much of aminoglycosides are eliminated in the kidney?
Aminoglycosides are well recognized nephrotoxins, causing a dose-dependent reduction in approximately 50% of kidney function (AKI) in 10%-20% of patients. 26 After administration, approximately 5%-10% of the dose will remain in the renal cortex. Aminoglycosides are 99% eliminated by the urine without prior metabolism.
What are the drugs that block angiotensin receptors?
Including: captopril (Capoten), lisinopril, ramipril, and angiotensin receptor blockers like candesartan and valsartan.
What are the drugs that are used to treat HIV?
Antiviral Drugs. Including: acyclovir (Zovirax), used to treat herpes infection, and indinavir, ritonavir, and tenofovir, all used to treat HIV. 6. High Blood Pressure Drugs. Including: captopril (Capoten), lisinopril, ramipril, and angiotensin receptor blockers like candesartan and valsartan.
What are the risks of kidney failure?
Acute kidney failure can lead to unpleasant problems including ( 6 ): Shortness of breath, caused by fluid buildup in the lungs. Chest pain, caused by inflammation of the lining that covers your heart (pericardium). Muscle weakness, caused by electrolyte imbalance.
What causes kidney damage?
Drugs are one of the most common causes of kidney damage. Over the last 30 years, instances of drug-induced acute kidney injury have been on the rise ( 2 ).
Can nephrotoxic drugs cause kidney damage?
Nephrotoxic Drugs That Cause Kidney Damage. Before taking any of these drugs, be aware that they are known to cause severe (and sometimes deadly) kidney damage ( 3, 4, 5 ). If you already have kidney problems, these drugs can be deadly even in small doses. And so, make sure to only take medication prescribed by your healthcare provider ...
What are the side effects of antibiotics?
More common side effects include: Nausea and vomiting. Diarrhoea. Loss of appetite. Photosensitivity.
What is interstitial nephritis?
Acute interstitial nephritis- inflammation and swelling in the kidney.
What is NAC used for?
NAC is used in hospitals to protect the kidneys from contrast dye which is known to cause nephrotoxicity and has the strongest evidence for prevention of acute kidney injury in humans.
What is the role of oxidative stress in kidney disease?
In every case of impaired kidney function, either acute or chronic, oxidative stress plays a key role in kidney damage. Reports have shown that reactive oxygen species and reactive nitrogen species are elevated in antibiotic nephrotoxicity and are responsible for a large amount of the damage caused by antibiotics.
What is the best vitamin for kidneys?
Vitamin E. Vitamin E is a potent fat-soluble antioxidant. Animal and human studies have demonstrated a beneficial effect of vitamin E in prevention of kidney damage induced by drugs including antibiotics.
How have antibiotics saved lives?
Antibiotics have not only saved peoples’ lives, but they have also played a pivotal role in achieving major advances in medicine and surgery. They have successfully prevented or treated infections that can occur in patients who are receiving chemotherapy treatments; who have chronic diseases; or who have had complex surgeries such as organ transplants, joint replacements, or cardiac surgery.
What is the inflammation of the filtering units of the kidney?
Acute glomerulonephritis – inflammation of the filtering units of the kidney.
What is the diagnosis of nephrotoxicity?
Thus the diagnosis of nephrotoxicity must rely on evidence of exposure to a sufficient quantity of a toxic chemical, clinical or analytic laboratory findings that confirm or strongly suggest toxicosis, and clinical or necropsy findings of compatible illness. These same principles should be applied to the diagnosis of emerging toxicities, such as melamine-cyanuric acid intoxication, associated with pet foods, and the recently recognized Fanconi syndrome in dogs that have consumed dog treats.
What is the purpose of laboratory testing for nephrotoxicity?
Laboratory testing often is required to establish the adverse effects of toxicity. Obviously increased serum urea nitrogen and creatinine concentrations, along with urinalysis, are used clinically to indicate renal injury. Urine specific gravity, cellular casts, and presence of crystals can aid in the diagnosis of acute nephrotoxicity. Calcium abnormalities are common with EG and with CCF toxicosis. Values within the normal range for all these tests would be interpreted as arguing against a diagnosis of nephrotoxicity. Such findings may not exclude exposure to a subtoxic dose of a nephrotoxic chemical.
What causes renal failure?
Renal failure is common, but only a small percent of cases of renal insufficiency are caused by chemical toxicants. The kidney constitutes only 1% of body weight in most mammals but receives about 25% of normal cardiac output. This high cardiac output exposes the kidney to many substances foreign to the body, including food additives, drugs, and other foreign chemicals (i.e., xenobiotics). These chemicals often reach relatively high concentrations in the renal ultrafiltrate. Kidneys also possess unique transporters that concentrate toxicants in this organ. In many instances a high concentration of xenobiotics is associated with nephrotoxicity, but other factors may also play a role.
What are the two tenets of toxicology?
Two tenets of toxicology are exposure and dose response . Pets must first be exposed to a toxicant for it to cause a toxicosis. Further, they must be exposed to a potentially toxic dose and have the adverse effect previously demonstrated for that toxicant before a clinician can reach a conclusive diagnosis of a toxicosis.
Which organs are responsible for the metabolism of endogenous and exogenous chemicals?
The kidneys also conduct substantial metabolism of endogenous and exogenous chemicals. Bioactivation of some chemicals can lead to nephrotoxicity, although metabolism of most chemicals leads to detoxification.
Can xenobiotics cause nephrotoxicity?
Animals may be predis posed to nephrotoxicity. Young and geriatric animals generally are believed to be more susceptible to the nephrotoxic effects of xenobiotics. Young animals may not have fully developed detoxifying enzyme systems, and these systems may be diminished in geriatric animals. Malnutrition, dehydration, shock, preexisting renal conditions, and concurrent exposure to multiple nephrotoxins are some of the factors that may influence the potential for nephrotoxicity.
Which antibiotics block neuromuscular transmission?
Since the original observations were made with streptomycin in patients with tuberculosis, many other aminoglycoside antibiotics have been implicated in neuromuscular and autonomic transmission blockade [5]. They include amikacin [6], tobramycin [7], neomycin [8], gentamicin [9], and kanamicin [9]. These neuromuscular blocking effects of aminoglycosides have implications in neurological conditions such as myasthenia gravis or Lambert Eaton myasthenic syndrome, where these antibiotics can worsen neuromuscular weakness and thus are contraindicated in these patients.
How does neurotoxicity occur in renally impaired patients?
Pathogenesis of neurotoxicity in renally impaired patients appears to be mediated by rise in serum concentrations, increased permeability of the blood-brain barrier secondary to blood urea increase, carbamylation, glycation or other chemical protein modification, as well as build up of toxic organic acids within the cerebrospinal fluid [30]. Increased circulating unbound antibiotic also contributes to the vulnerability of renally compromised patients to CNS toxicity [31, 32]. As with other beta-lactams, the basic mechanism for this neurotoxicity includes decreased gamma-aminobutyric acid (GABA) release from nerve terminals, increased excitatory amino acid release, as well as cytokine release [33, 34]. Other postulated mechanisms for cephalosporin neurotoxicity also include induction of endotoxins and, possibly, glutaminergic mechanisms. Laboratory studies also show that cephalosporins with high affinity for GABA-A receptors and those with high penetrance through the blood-brain barrier are more neurotoxic [34].
What are the risk factors for neurotoxicity?
As previously mentioned, these include extremes of age, impaired renal function, history of central nervous system disease, and/or damage to the blood-brain barrier (Figure 1). Other important factors to consider are body size (volume of distribution), as well as co-administration with other medications with neurotoxic and/or nephrotoxic effects, as well as any epileptogenic potential [41]. Apart from altered mental status induced by the antibiotic itself, the nephrotoxicity sometimes induced by antibiotics may itself be responsible for the encephalopathy. Early diagnosis is therefore essential in minimizing neurotoxic adverse effects. Thus avoidance of neurotoxic agents in patients with the above-mentioned risk factors is critical in preventing neurotoxicity.
What are the symptoms of cephalosporin?
Their myriad of neurological symptoms included lethargy, confusion, agitation, global aphasia, chorea-athetosis, seizures, myoclonus and coma, which were slowly progressive in evolution. EEGs of all patients demonstrated diffuse slowing with triphasic waves suggestive of toxic-metabolic encephalopathy (without any epileptiform features) [17]. Mortality was high in all cases.
Can ciprofloxacin cause neurotoxicity?
Neurotoxic manifestations associated with quinolones include seizures, confusion/encephalopathy, myoclonus and toxic psychosis (Table 2). Complex partial status epilepticus or NCSE documented by EEG have been reported with ciprofloxacin-induced neurotoxicity in patients presenting with altered mental status or confusion [62]. One case report described generalized myoclonus with delirium with ciprofloxacin [63]. That being said, EEG manifestation of fluoroquinolone-associated delirium, range from normal EEGs to diffuse slowing [64, 65]. Interestingly, CNS penetration of fluoroquinolones does not always correlate with the potential for epileptogenicity [66]. In contrast to ciprofloxacin, ofloxacin has an increased CNS permeability of 50% of the serum concentration, though interestingly less cases of neurotoxicity have been reported for ofloxacin than for ciprofloxacin [67].
Is cefazolin neurotoxic?
Neurotoxicity has been reported with first generation cephalosporins such as cefazolin, second generation such as cefuroxime, third generation such as ceftazidime and fourth generation such as cefepime and can range from encephalopathy to non-convulsive status epilepticus [13] (Table 1). This is particularly true in the setting of renal impairment though cases also exist in those with normal creatinine clearance. Previous CNS disease has also been suggested as decreasing the threshold of nervous system toxicity with use of third and fourth generation cephalosporins [14]. In addition to pre-existing CNS conditions, reduced creatinine clearance, impaired renal function and excess dosage of medication have been described as independent risk factors for neurotoxic effects [15]. The typical time period for encephalopathy induced by cephalosporin use is a latency of 1 to 10 days following start of medication, and resolution in 2 to 7 days following discontinuation [16].
Does metronidazole cause neurotoxicity?
Metronidazole can have cerebellar toxicity that manifests clinically with varying degrees of limb and gait ataxia and dysarthria (Table 2). Symptoms are accompanied by characteristic T2 high signal lesions on brain MRI in the cerebellum and brainstem. Neurotoxicity was seen after prolonged use of metronidazole with clinical symptoms resolving within 3–7 days of discontinuation of the medication, while follow-up MRIs also show resolution of cerebellar lesions [111]. While the precise mechanism for neurotoxicity is not entirely clear, one hypothesis is that it occurs via axonal swelling secondary to metronidazole-induced vasogenic oedema [112]. Peripheral neuropathy is another recognized potentially neurotoxic effect with use of metronidazole. One report describes a 53-year-old who developed encephalopathy, dysarthria, ataxia and a length-dependent peripheral neuropathy in the context of prolonged metronidazole therapy (a cumulative dose of 146 g over 88 days). Multiple skin biopsies confirmed evidence of a small fibre sensory neuropathy [113]. In another case reporting the rapid development of peripheral neuropathy related to metronidazole with electrophysiologic studies demonstrating prolonged distal motor latencies, mildly decreased compound muscle action potential and decreased sensory nerve action potentials involving the posterior tibial and peroneal nerves to varying degrees were noted [114]. Optic neuropathy, as well as autonomic neuropathy, have also been described in association with metronidazole use [115, 116]. Other neurological adverse effects ascribed to metronidazole include dizziness, headache and confusion [117].