What are the causes of anti-Kell hemolytic disease of the newborn?
Anti-Kell hemolytic disease of the newborn is most commonly caused by anti-K 1 antibodies, the second most common form of severe HDN. Over half of the cases of anti-K 1 related HDN are caused by multiple blood transfusions. Antibodies to the other Kell antigens are rare. Anti-Kell can cause severe anemia regardless of titer.
What is hemolytic disease of the fetus and newborn (HDFN)?
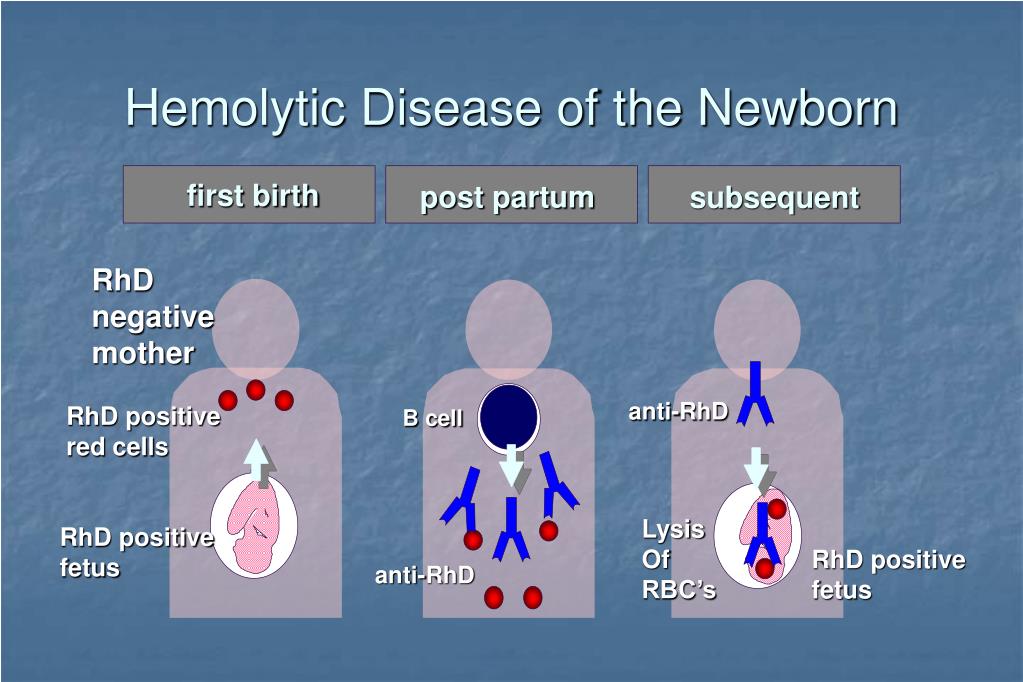
Hemolytic disease of the fetus and newborn (HDFN) is an immune-mediated red blood cell (RBC) disorder in which maternal antibodies attack fetal or newborn RBCs. [1][2] HDFN can cause significant morbidity and mortality, especially in limited healthcare resource settings.
Does anti-JKB cause severe hemolytic disease of the newborn?
Abstract Although anti-Jkb is a well-defined cause of severe acute or delayed hemolytic transfusion reactions, it is rarely associated with severe Hemolytic Disease of the Newborn (HDN), even with high antibody titer. To date, only 13 cases have been reported, so the possible reasons for that still remain unclear.
What is ABO hemolytic disease of the newborn?
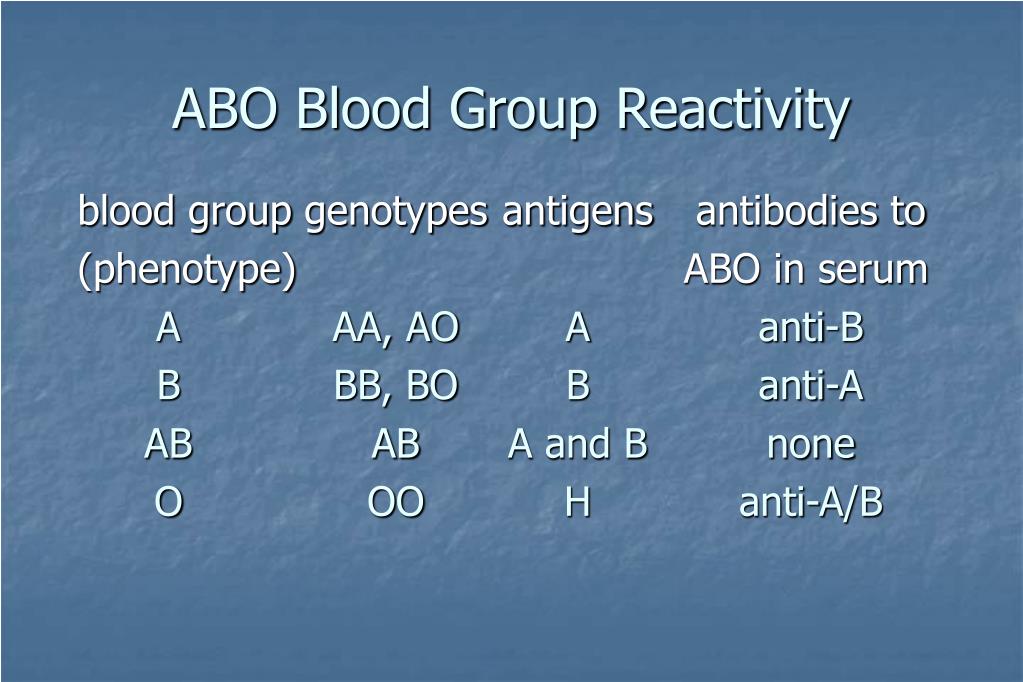
ABO hemolytic disease of the newborn can range from mild to severe, but generally, it is a mild disease. It can be caused by anti-A and anti-B antibodies. [15] Rhesus D hemolytic disease of the newborn (often called Rh disease) is the most common and only preventable form of severe HDN.
What causes hemolytic disease in newborns?
What is the term for a fetal hemolytic disease?
How much fetal blood is needed for alloimmunization?
Why is routine lab testing necessary for Rh negative women?
What is the interprofessional team for hemolytic disease?
When was hemolytic disease first described?
Can a rh negative fetus have an rh positive fetus?
See 4 more
About this website
What is the most frequently seen cause of hemolytic disease of the newborn?
HDN happens most often when an Rh negative mother has a baby with an Rh positive father. If the baby's Rh factor is positive, like his or her father's, this can be an issue if the baby's red blood cells cross to the Rh negative mother. This often happens at birth when the placenta breaks away.
What causes anti-c antibody?
Anti-c antibodies may occur due to exposures, such as feto- maternal hemorrhage, abruptio placentae, spontaneous or therapeutic abortion, cesarean delivery, ectopic pregnancy or transfusion. [10] They may cause acute or delayed hemo- lytic reactions.
What is anti M antibodies in pregnancy?
Anti-M is a common antibody detected in prenatal samples. Most often it is not clinically significant as it is predominantly an IgM antibody which does not cross the placental barrier. To distinguish IgM from IgG anti-M, some antibody identification methods exist that exclude IgM antibodies.
What is anti-c and anti-E?
Anti-c is an IgG antibody directed against the c antigen in the Rh blood group system. Anti-c is implicated in Hemolytic Transfusion Reactions and Hemolytic Disease of the Fetus and Newborn. Patients with Anti-c must receive c- blood. Anti-e is an antibody directed against the e antigen in the Rh blood group system.
Is Duffy IgG or IgM?
IgG subclassThe Duffy antibodies are predominantly of the IgG subclass whereas the IgM form is rare.
What is anti-N antibody?
Anti-N antibody. – Not previously vaccinated or infected. Interpretation* Not previously vaccinated or infected.
Does anti-N cause HDN?
CLINICAL: Anti-N is an uncommon antibody that does not cause hemolytic transfusion reactions or HDN. Selection of N-negative blood for transfusion is not necessary and the antibody can be ignored.
Can anti m cause HDN?
Anti-M is capable of causing HDN as well as prolonged anemia (red cell aplasia) due to its ability to destroy the erythroid precursor cells. Newborns with anemia should be evaluated for all the possible causes to establish a diagnosis and its efficient management.
Is anti c clinically significant?
Anti-c is clinically the most important Rh antigen after anti-D and often causes severe HDN [4]. Properly formulated protocols to screen pregnant women for irregular antibodies need to be imposed to prevent perinatal mortality and morbidity [5].
What causes antibodies in blood during pregnancy?
How are these antibodies made during pregnancy? A few of your baby's blood cells may 'leak' into your blood during pregnancy. This usually happens when the baby is born. If your baby's blood group is different from your own, your immune system may produce antibodies.
How common is hemolytic disease?
HDN is relatively uncommon in the United States due to advances in early detection and treatment, limiting it to approximately 4,000 cases a year. It is more likely to happen during a mother's second or subsequent pregnancy. There are two causes, Rh incompatibility and ABO incompatibility.
What are hemolytic diseases?
Hemolytic anemia is a disorder in which red blood cells are destroyed faster than they can be made. The destruction of red blood cells is called hemolysis. Red blood cells carry oxygen to all parts of your body. If you have a lower than normal amount of red blood cells, you have anemia.
26 HEMOLYTIC DISEASE OF THE NEW BORN (HDNB) - National Institute of ...
MODULE Hemolytic Disease of the New Born (HDNB) Hematology and Blood Bank Technique 244 HEMATOLOGY AND BLOOD BANK TECHNIQUE Notes Tests on cord blood: (a) ABO & Rh Group (b) Direct Coomb’s test (c) Hemoglobin (d) Bilirubin Tests on maternal blood
Hemolytic Diseases Of The Newborn - PubMed
Hemolytic disease of the fetus and newborn (HDFN) is an immune-mediated red blood cell (RBC) disorder in which maternal antibodies attack fetal or newborn RBCs. HDFN can cause significant morbidity and mortality, especially in limited healthcare resource settings. Effects of HDFN range from mild ane …
Hemolytic Disease of the Newborn (HDN) - Lucile Packard Children's Hospital
Hemolytic disease of the newborn (HDN) is a blood problem in newborns. It occurs when your baby's red blood cells break down at a fast rate. It’s also called erythroblastosis fetalis.
Hemolytic Disease of the Newborn: A Review of Current Trends and ...
Hemolytic disease of the newborn (HDN), also known as Erythroblastosis fetalis, is a hemolytic condition that predominantly affects rhesus-positive fetuses and infants born to rhesus-negative mothers.The pathophysiology of HDN begins with maternal antibodies attacking fetal red blood cells following alloimmunization due to rhesus or ABO incompatibility between the maternal and fetal blood.
Hemolytic Disease of the Newborn - Children's Hospital of Philadelphia
When the mother's antibodies attack the red blood cells, they are broken down and destroyed (hemolysis). This makes the baby anemic. Anemia is dangerous because it limits the ability of the blood to carry oxygen to the baby's organs and tissues.
Who is affected by hemolytic disease of the newborn?
Babies affected by HDN are usually in a mother's second or higher pregnancy, after she has become sensitized with a first baby. HDN due to Rh incompatibility is about three times more likely in Caucasian babies than African-American babies.
What is hemolytic disease of the newborn (HDN)?
Hemolytic disease of the newborn is also called erythroblastosis fetalis. This condition occurs when there is an incompatibility between the blood types of the mother and baby.
What happens to the baby when the mother's antibodies cross the placenta?
As the antibodies destroy the red blood cells, the baby can become sick. This is called erythroblastosis fetalis during pregnancy. In the newborn, the condition is called hemolytic disease of the newborn.
How to detect a Rh negative mother?
Because of the advances in prenatal care, nearly all women with Rh negative blood are identified in early pregnancy by blood testing . If a mother is Rh negative and has not been sensitized, she is usually given a drug called Rh immunoglobulin (RhIg), also known as RhoGAM. This is a specially developed blood product that can prevent an Rh negative mother's antibodies from being able to react to Rh positive cells. Many women are given RhoGAM around the 28th week of pregnancy. After the baby is born, a woman should receive a second dose of the drug within 72 hours, if her baby is Rh positive. If her baby is Rh negative, she does not need another dose.
What is the term for a baby's organs that are unable to handle anemia?
Hydrops fetalis. This occurs as the baby's organs are unable to handle the anemia. The heart begins to fail and large amounts of fluid build up in the baby's tissues and organs. A fetus with hydrops is at great risk of being stillborn.
How long does it take for a baby to turn yellow?
The baby may not look yellow immediately after birth, but jaundice can develop quickly, usually within 24 to 36 hours.
Why do we collect blood from the umbilical cord during pregnancy?
Sampling of some of the blood from the fetal umbilical cord during pregnancy to check for antibodies, bilirubin, and anemia in the fetus.
What is the medical term for hemolytic disease of the newborn?
Pediatrics, Immunohaematology. Complications. heart failure, splenomegaly. Hemolytic disease of the newborn, also known as hemolytic disease of the fetus and newborn, HDN, HDFN, or erythroblastosis foetalis, is an alloimmune condition that develops in a fetus at or around birth, when the IgG molecules (one of the five main types of antibodies) ...
How to tell if a newborn has hemolytic disease?
Signs of hemolytic disease of the newborn include a positive direct Coombs test (also called direct agglutination test), elevated cord bilirubin levels, and hemolytic anemia. It is possible for a newborn with this disease to have neutropenia and neonatal alloimmune thrombocytopenia as well. Hemolysis leads to elevated bilirubin levels. After delivery bilirubin is no longer cleared (via the placenta) from the neonate's blood and the symptoms of jaundice (yellowish skin and yellow discoloration of the whites of the eyes, or icterus) increase within 24 hours after birth. Like other forms of severe neonatal jaundice, there is the possibility of the neonate developing acute or chronic kernicterus, however the risk of kernicterus in HDN is higher because of the rapid and massive destruction of blood cells. It is important to note that isoimmunization is a risk factor for neurotoxicity and lowers the level at which kernicterus can occur. Untreated profound anemia can cause high-output heart failure, with pallor, enlarged liver and/or spleen, generalized swelling, and respiratory distress.
What is IVIG used for?
IVIG - IVIG has been used to successfully treat many cases of HDN. It has been used not only on anti-D, but on anti-E as well.< IVIG can be used to reduce the need for exchange transfusion and to shorten the length of phototherapy. The AAP recommends "In isoimmune hemolytic disease, administration of intravenousγ-globulin (0.5-1 g/kg over 2 hours) is recommended if the TSB (total serum bilirubin) is rising despite intensive phototherapy or the TSB level is within 2 to 3 mg/dL (34–51 μmol/L) of the exchange level. If necessary, this dose can be repeated in 12 hours (evidence quality B: benefits exceed harms). Intravenous γ-globulin has been shown to reduce the need for exchange transfusions in Rh and ABO hemolytic disease."
What is hemolytic disease?
Hemolytic disease of the newborn, also known as hemolytic disease of the fetus and newborn, HDN, HDFN, or erythroblastosis foetalis, is an alloimmune condition that develops in a fetus at or around birth, when the IgG molecules ...
What is the most common form of HDN?
Rhesus D hemolytic disease of the new born (often called Rh disease) is the most common and only preventable form of severe HDN. Since the introduction of Rho-D immunoglobulin, ( Rhogam, at 1968, which prevents the production of maternal Rho-D antibodies, the incidence of anti-D HDN has decreased dramatically.
What are the complications of HDN?
Complications of HDN could include kernicterus, hepatosplenomegaly, inspissated (thickened or dried) bile syndrome and/or greenish staining of the teeth, hemolytic anemia and damage to the liver due to excess bilirubin. Conditions that may cause similar symptoms in the newborn period include: acquired hemolytic anemia, congenital toxoplasma, congenital syphilis infection, congenital obstruction of the bile duct, and cytomegalovirus (CMV) infection.
What is the third sensitization model?
The third sensitization model can occur in women of blood type O. The immune response to A and B antigens , which are widespread in the environment, usually leads to the production of IgM or IgG anti-A and anti-B antibodies early in life. Women of blood type O are more prone than women of types A and B to making IgG anti-A and anti-B antibodies, and these IgG antibodies are able to cross the placenta. For unknown reasons, the incidence of maternal antibodies against type A and B antigens of the IgG type that could potentially cause hemolytic disease of the newborn is greater than the observed incidence of "ABO disease." About 15% of pregnancies involve a type O mother and a type A or type B child; only 3% of these pregnancies result in hemolytic disease due to A/B/O incompatibility. In contrast to antibodies to A and B antigens, production of Rhesus antibodies upon exposure to environmental antigens seems to vary significantly across individuals. In cases where there is ABO incompatibility and Rh incompatibility, the risk of alloimmunization is decreased because fetal red blood cells are removed from maternal circulation due to anti-ABO antibodies before they can trigger an anti-Rh response.
What is the mechanism of hemolytic disease?
Hemolytic disease of the fetus and newborn (HDN) is a condition where the passage of maternal antibodies results in the hemolysis of fetal/neonatal red cells. The antibodies can be naturally occurring such as anti-A, and anti-B, or immune antibodies developed following a sensitizing event.
How many babies born to a negative mother are kell 1 positive?
Therefore, about 4.5% of babies born to a Kell 1 negative mother are Kell 1 positive. The disease results when maternal antibodies to Kell 1 are transferred to the fetus across the placental barrier, breaching immune privilege.
What is HDN in medical terms?
Medical condition. HDN due to anti-Kell alloimmunization. Specialty. Obstetrics, maternal–fetal medicine, neonatology. Hemolytic disease of the newborn (anti-Kell1) is the second most common cause of severe hemolytic disease of the newborn (HDN) after Rh disease. Anti-Kell 1 is becoming relatively more important as prevention ...
Why is anti-Kell 1 important?
Anti-Kell 1 is becoming relatively more important as prevention of Rh disease is also becoming more effective. Hemolytic disease of the newborn (anti-Kell 1) is caused by a mismatch between the Kell antigens of the mother and fetus. About 91% of the population are Kell 1 negative and about 9% are Kell 1 positive.
What causes isoimmunization?
The most common causes of isoimmunization are blood transfusion, and fetal-maternal hemorrhage. The hemolytic process can result in anemia, hyperbilirubinemia, neonatal thrombocytopenia, and neonatal neutropenia.
What tests are done for HDN?
Testing for HDN involves blood work from both mother and father, and may also include assessment with amniocentesis and Middle Cerebral Artery scans.
What is the test for RhD?
This test can help with knowledge for the current baby, as well as aid in the decision about future pregnancies. With RhD, the test is called the RhD genotype. With RhCE, and Kell antigen it is called an antigen phenotype.
What are antibody titers used for?
Antibody titers can be used to monitor the risk of HDFN in pregnancies affected by alloimmunization. 1#N#ACOG Practice Bulletin No. 192: Management of Alloimmunization During Pregnancy. Obstet Gynecol. 2018; 131 (3): e82-e90.#N#In alloimmunized mothers who have not had a previous HDFN-affected pregnancy, the titer of maternal antibodies against the antigen in question can be used to determine whether intervention may be necessary. 1#N#ACOG Practice Bulletin No. 192: Management of Alloimmunization During Pregnancy. Obstet Gynecol. 2018; 131 (3): e82-e90.#N#A critical antibody titer indicates significant risk for HDFN and hydrops fetalis and requires fetal monitoring with ultrasound. 1#N#ACOG Practice Bulletin No. 192: Management of Alloimmunization During Pregnancy. Obstet Gynecol. 2018; 131 (3): e82-e90.#N#, 3#N#Royal College of Obstetricians & Gynaecologists. The Management of Women with Red Cell Antibodies during Pregnancy. Green-top Guideline No. 65. May 28, 2014. [Accessed: Nov 2019]
What is the chance of a fetus being RhD positive?
If the father is homozygous for the D antigen, then all of his offspring will be RhD positive; if heterozygous, there is a 50% chance that the fetus will be RhD positive. 1. ACOG Practice Bulletin No. 192: Management of Alloimmunization During Pregnancy. Obstet Gynecol. 2018; 131 (3): e82-e90.
What is the ABO/RH screen?
ABO/Rh typing and an antibody screen are recommended for all pregnant women to assess the risk of HDFN development, identify alloantibodies, and determine the need for anti-D immune globulin prophylaxis. 1#N#ACOG Practice Bulletin No. 192: Management of Alloimmunization During Pregnancy. Obstet Gynecol. 2018; 131 (3): e82-e90.
What is HDFN in pregnancy?
HDFN occurs when fetal red blood cells (RBCs) are destroyed by maternal alloantibodies that have crossed into the fetal circulation, leading to hemolysis and anemia. 1. ACOG Practice Bulletin No. 192: Management of Alloimmunization During Pregnancy.
What is the medical term for hemolytic disease of the fetus and newborn?
Hemolytic disease of the fetus and newborn (HDFN), also known as hemolytic disease of the newborn (HDN) or alloimmune HDFN, is a potentially severe alloimmune condition that may, on rare occasions, result in stillbirth or neonatal death. 1. ACOG Practice Bulletin No. 192: Management of Alloimmunization During Pregnancy.
Why is chorionic villus biopsy discouraged?
Therefore, the use of chorionic villus biopsy is discouraged in testing for hemolytic disease of the fetus and newborn (HDFN) because it is more likely to cause fetomaternal hemorrhage and worsen alloimmunization than other techniques (eg, amniocentesis). 1.
When should I screen for anti-D antibodies?
Obstet Gynecol. 2017; 130 (2): e57-e70. Antibody screening is also recommended before anti-D immune globulin treatment at 28 weeks of gestation, postpartum , and in association with any pregnancy event that may result in fetomaternal hemorrhage to confirm that RhD sensitization has not occurred. 1.
What antigens are used in routine antenatal screening?
We consider routine antenatal antibody screening as an essential strategy to be carried out in every pregnant woman, irrespective of her Rh(D) phenotype, in order to detect red cell alloimmunization to other clinically significant blood group antigens such as Kidd, Duffy or Kell.
How to sensitize against Kidd antigens?
The most common route of sensitization against Kidd antigens is via blood transfusion. Antibodies are usually IgG able to cross the placenta, bind complement and produce rapid either intravascular and/or extravascular hemolysis. In those fetal RBC-maternal blood contact cases, the sensitization is rare but possible.
What causes fetomaternal incompatibility?
The vast majority of cases of fetomaternal incompatibility are due to ABO sensitization, although most of severe HDN are produced by anti-RhD. The proportion of cases that has been caused by Kell, Duffy, Kidd and other systems is just around 3 % [5–11]. Kidd antigens can be detected from the 7th week of gestation and are well developed at birth. When alloimmunization occurs it can potentially lead to a HDN which usually has a mild clinical course and a good outcome.
How many cases of anti-JKB related HDN?
There are only thirteen cases of anti-Jkb related HDN reported in medical literature (Table 2) [12–23]. Most of them (76.92 %) were mild and the newborn required either phototherapy (4 cases: 30.76 %) or no treatment at all. Only Merlob’s case needed red blood cell transfusion. Despite of these data, 2 cases (15.38 %) had a fatal outcome. One of them developed hidrops fetalis and intrauterine death [21], and the second one died of acute renal failure 4 days after birth in spite of intensive treatment with exchange transfusion and phototherapy for 3 days [17].
Is anti-JKB titer low during pregnancy?
Follow-up was continued and anti-Jkb titer remained low during whole pregnancy. No data of anemia were noted in the fetus, thus no intrauterine transfusion was required. At August 10th of current year, our patient delivered a female infant after 40 weeks gestation. Her weight was 3.15 kg. The baby had no complications at birth and she was a normal full-term infant, without jaundice or data of hemolysis.
Is anti-JKB a cause of HDN?
Although anti-Jkb is a well-defined cause of severe acute or delayed hemolytic transfusion reactions, it is rarely associated with severe Hemolytic Disease of the Newborn (HDN), even with high antibody titer. To date, only 13 cases have been reported, so the possible reasons for that still remain unclear. Most of HDN due to anti-Jkb are mild-to-moderate, and usually have a good prognosis. A 41-years-old woman, who had a positive antibody screening test in her 13th week of pregnancy, was sent to the blood bank for study before an amniocentesis. Antibody identification and red blood cell (RBC) phenotyping of the patient and his husband were performed, plus arrays study in the amniotic fluid. An anti-Jkb was identified in the patient’s serum with a titer of 1:1, and her RBC phenotype was O Rh(D) positive, C(+), c(+), E(−), e(+), K(−), Jka(+), Jkb(−). The RBC genotype of the fetus was B Rh(D) positive, Jka(+), Jkb(+). Antibody titer remained stable and the pregnancy was uneventful. At birth, there was no need of phototherapy or exchange transfusion for the newborn and her Jk(b+) typing result was confirmed in a cord blood sample. Although most of HDN cases due to anti-Jkb have a good outcome, monitoring antibody titer should be done to prevent fatal complications. Furthermore, antenatal antibody screening should be performed in every pregnant woman irrespective of her Rh(D) antigen status in order to detect red cell alloimmunization to other clinically significant blood group antigens.
What causes hemolytic disease in newborns?
As mentioned, there are two mechanisms causing hemolytic disease of the fetus and newborn. First, the fetomaternal pair can have inherent ABO incompatibility , which occurs in 15 to 25% of pregnancies.[8] Only about 1% of those pairs, those with high IgG titers, will develop HDFN due to ABO incompatibility.[8] In ABO incompatibility, naturally occurring antigens against A or B blood types are present in mothers with O blood type. If the mother's fetus has an A or B (or AB) blood type, these maternal anti-A and/or anti-B antibodies, respectively, will attack the foreign blood type of the fetus. The anti-A and anti-B antibodies are IgG, which can cross the placenta and affect the developing fetus.[9] Compared with FMH, ABO incompatibility generally causes a less severe form of HDFN. Postulated theories for this include fetal RBCs express less ABO blood group antigens than adult levels and that ABO blood group antigens are expressed by many tissues, which reduces the chance that antibodies specifically target the antigens on fetal RBCs. [4]
What is the term for a fetal hemolytic disease?
Hemolytic disease of the fetus and newborn (HDFN) is an immune-mediated red blood cell (RBC) disorder in which maternal antibodies attack fetal or newborn RBCs. [1][2] HDFN can cause significant morbidity and mortality, especially in limited healthcare resource settings. Effects of HDFN range from mild anemia to hydrops fetalis in the fetus and hyperbilirubinemia and kernicterus in the newborn. [1][3] Through early detection, management, and prevention of this disease, the incidence, and prevalence of HDFN has exponentially decreased in the past 50 years. [1]
How much fetal blood is needed for alloimmunization?
As little as 0.1 mL of fetal blood entering maternal circulation is sufficient to cause alloimmunization.[7] In fact, 15 to 50% of gestations have sufficient fetomaternal hemorrhage to cause alloimmunization, and only 1 to 2% of all Rh alloimmunization is caused by antepartum FMH.[7] As such, it is important to consider HDFN at all stages of the pregnancy where FMH may occur.
Why is routine lab testing necessary for Rh negative women?
Patient education regarding routine lab testing and Rh-D immunoprophylaxis in Rh-negative women are necessary to ensure possible FMH events are reported and appropriately treated in pregnant women. Additionally, parents of newborns can be educated on signs and symptoms to be aware of in hyperbilirubinemia to assist the interprofessional team in the early identification of possible HDFN cases.
What is the interprofessional team for hemolytic disease?
Enhancing interprofessional team outcomes for patients with hemolytic disease of the fetus and newborn requires close collaboration between both OB/GYN and pediatric providers, nurses, pharmacists, and blood bank personnel. With HDFN, there are two patients to consider at all times - the mother and the fetus/newborn. When HDFN is identified in utero, the delivery team should be well versed and prepared ahead of time to identify signs and symptoms of HDFN as these infants may need timely transfusions at birth. Pharmacists and providers must identify if and when Rh-D immunoprophylaxis is indicated to prevent future HDFN cases throughout the pregnancy. Through the development of Rh-D immunoprophylaxis and newborn work-up protocols, the incidence of HDFN has dramatically dropped in the past 50 years. Still, it will take continued interprofessional collaboration to ensure the incidence of HDFN remains low.
When was hemolytic disease first described?
Hemolytic disease of the fetus and newborn was first described by Dr. Louis K. Diamond in 1932 when he wrote about erythroblastosis fetalis in the newborn based on peripheral smears.[6] Rhesus D-negative (RhD) immunoprophylaxis was first introduced in 1968, which dropped the incidence of HDFN from 1% of all newborns worldwide (with 50% mortality) to 0.5%.[1] The incidence of HDFN decreased even further to 0.1% with the administration of antepartum RhD immunoprophylaxis.[2] However, despite adequate RhD immunoprophylaxis, an estimated 1 to 3 in 1000 Rh-negative women still develop alloimmunization today. Thus it is important to stay vigilant for the development of HDFN. [1]
Can a rh negative fetus have an rh positive fetus?
For example, an Rh-negative woman can have an Rh-positive fetus due to her partner being Rh- positive. Antibodies that develop due to FMH put subsequent pregnancies at risk for HDFN as the first antibodies to develop are of IgM type, which cannot cross the placenta. In subsequent encounters with the Rh-D antigen, maternal antibodies rapidly develop IgG antibodies, which do cross the placenta. [11]
Overview
Pathophysiology
Antibodies are produced when the body is exposed to an antigen foreign to the make-up of the body. If a mother is exposed to a foreign antigen and produces IgG (as opposed to IgM which does not cross the placenta), the IgG will target the antigen, if present in the fetus, and may affect it in utero and persist after delivery. The three most common models in which a woman becomes sensitized toward (i.e., produces IgG antibodies against) a particular antigen are hemorrhage, blo…
Signs and symptoms
Signs of hemolytic disease of the newborn include a positive direct Coombs test (also called direct agglutination test), elevated cord bilirubin levels, and hemolytic anemia. It is possible for a newborn with this disease to have neutropenia and neonatal alloimmune thrombocytopenia as well. Hemolysis leads to elevated bilirubin levels. After delivery, bilirubin is no longer cleared (via the placenta) from the neonate's blood and the symptoms of jaundice (yellowish skin and yellow discol…
Diagnosis
The diagnosis of HDN is based on history and laboratory findings:
Blood tests done on the newborn baby
• Biochemistry tests for jaundice including total and direct bilirubin levels.
• Complete blood count (CBC) which may show a decreased hemoglobin and hematocrit due to red blood cell destruction
Prevention
In cases of Rho(D) incompatibility, Rho(D) immunoglobulin is given to prevent sensitization. However, there is no comparable immunotherapy available for other blood group incompatibilities.
Early pregnancy
• IVIG – IVIG stands for Intravenous Immunoglobulin. It is used in cases of previous loss, high maternal titers, known aggressive antibodies, and in cases where religion prevents blood transfu…
After birth testing
• Coombs – in certain instances (when there is concern for blood group incompatibility between mother and baby for example), after birth a baby will have a direct Coombs test run to confirm the antibodies attached to the infant's red blood cells. This test is run on the infant's cord blood.
In some cases, the direct Coombs will be negative but severe, even fatal HDN can occur. An indirect Coombs needs to be run in cases of anti-C, anti-c, and anti-M. Infants with Anti-M are al…
Treatment
After birth, treatment depends on the severity of the condition, but could include temperature stabilization and monitoring, phototherapy, transfusion with compatible packed red blood, exchange transfusion, sodium bicarbonate for correction of acidosis and/or assisted ventilation.
• Phototherapy – Exposure to ultraviolet light (phototherapy) is recommended when the cord bilirubin is 3 or higher. Some doctors use it at lower levels while awaiting lab results. This conver…
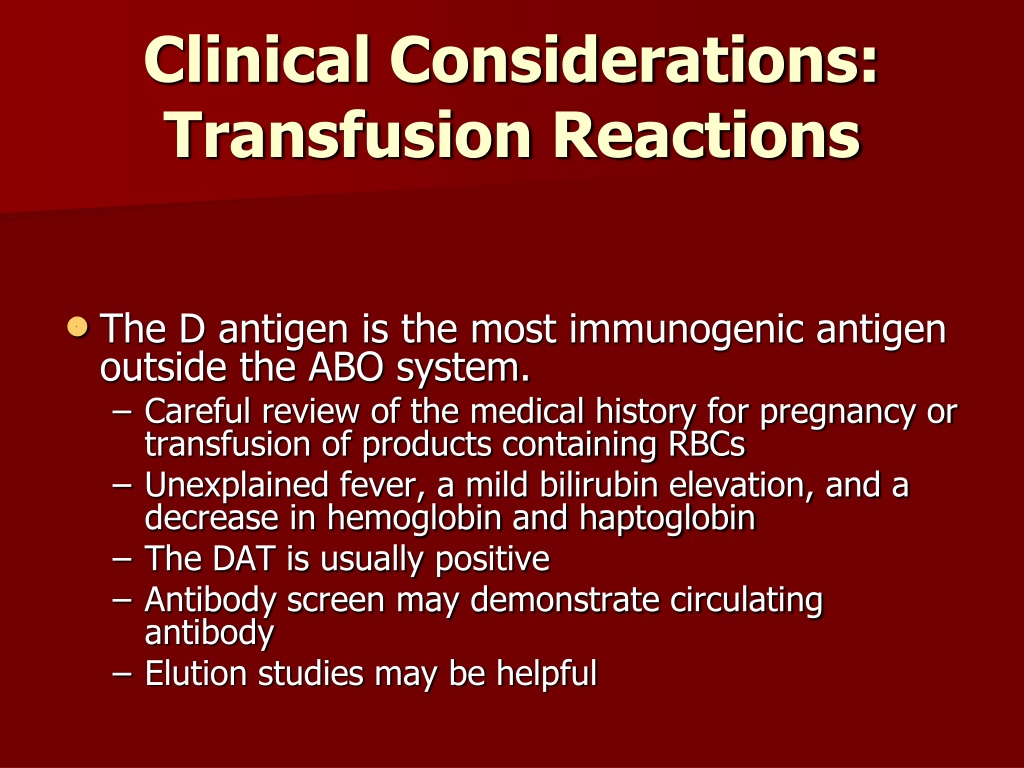
Transfusion reactions
Once a woman has antibodies, she is at high risk for a future transfusion reaction if she is in need of a blood transfusion. For this reason, she must carry a medical alert card at all times and inform all doctors and emergency personnel of her antibody status. The absence of antibodies however does not preclude a woman from having a transfusion reaction:
"Acute hemolytic transfusion reactions may be either immune-mediated or nonimmune-mediate…
Overview
Hemolytic disease of the newborn (anti-Kell1) is the second most common cause of severe hemolytic disease of the newborn (HDN) after Rh disease. Anti-Kell1 is becoming relatively more important as prevention of Rh disease is also becoming more effective.
Hemolytic disease of the newborn (anti-Kell1) is caused by a mismatch between the Kell antigens of the mother and fetus. About 91% of the population are Kell1 negative and about 9% are Kell1 posi…
Mechanism
Hemolytic disease of the fetus and newborn (HDN) is a condition where the passage of maternal antibodies results in the hemolysis of fetal/neonatal red cells. The antibodies can be naturally occurring such as anti-A, and anti-B, or immune antibodies developed following a sensitizing event. Isoimmunization occurs when the maternal immune system is sensitized to red blood cell surface antigens. The most common causes of isoimmunization are blood transfusion, and fetal …
Presentation
• High at birth or rapidly rising bilirubin
• Prolonged hyperbilirubinemia
• Bilirubin Induced Neuorlogical Dysfunction
• Cerebral Palsy
Cause
Mothers who are negative for the Kell1 antigen develop antibodies after being exposed to red blood cells that are positive for Kell1. Over half of the cases of hemolytic disease of the newborn owing the anti-Kell antibodies are caused by multiple blood transfusions, with the remainder due to a previous pregnancy with a Kell1 positive baby.
Diagnosis
Testing for HDN involves blood work from both mother and father, and may also include assessment with amniocentesis and Middle Cerebral Artery scans.
Blood testing for the mother is called an Indirect Coombs Test (ICT) or an Indirect Agglutination Test (IAT). This test tells whether there are antibodies in the maternal plasma. If positive, the antibody is identified and given a titer. Titers of 1:4 or higher is considered critical for Kell (comp…
Management
There are several intervention options available in early, mid and late pregnancies.
• IVIG - IVIG stands for Intravenous Immunoglobulin. It is used in cases of previous loss, high maternal titers, known aggressive antibodies, and in cases where religion prevents blood transfusion. Ivig can be more effective than IUT alone. Fetal mortality was reduced by 36% in the IVIG and IUT group than in the IUT alone group. IVIG and plasmapheresis together can reduce …
After Birth
• Coombs - after birth baby will have a direct coombs test run to confirm antibodies attached to the infant's red blood cells. This test is run from cord blood.
In some cases, the direct coombs will be negative but severe, even fatal HDN can occur. An indirect coombs needs to be run in cases of anti-C, anti-c, and anti-M. Anti-M also recommends antigen testing to rule out the presence of HDN.
Prevention
Suggestions have been made that women of child-bearing age or young girls should not be given a transfusion with Kell1 positive blood. Donated blood is not currently screened (in the U.S.A.) for the Kell blood group antigens as it is not considered cost effective at this time.
It has been hypothesized that IgG anti-Kell1 antibody injections would prevent sensitization to RBC surface Kell1 antigens in a similar way that IgG anti-D antibodies (Rho(D) Immune Globulin) …