/GettyImages-493216369-5b96800746e0fb0050dfabdf.jpg)
Explore
Neuroleptic malignant syndrome (NMS) can affect anyone taking neuroleptic (antipsychotic) medications. Although two-thirds of NMS cases are thought to occur within the first week of starting neuroleptic medications, the syndrome may happen at any time during treatment. How common is neuroleptic malignant syndrome?
Can you have neuroleptic malignant syndrome with antipsychotics?
Background. Neuroleptic malignant syndrome (NMS) is a severe disorder caused by an adverse reaction to medications with dopamine receptor-antagonist properties or the rapid withdrawal of dopaminergic medications. The first reported case of NMS appeared in 1956, shortly after the introduction of the antipsychotic drug chlorpromazine (thorazine).
What is the history of neuroleptic malignant syndrome?
A case of neuroleptic malignant syndrome successfully treated with amantadine. J Clin Psychiatry. 1982;43(9):381–382 [PubMed] [Google Scholar] 61. Henderson VW, Wooten GF.
Which medications are used to treat neuroleptic malignant syndrome (NMS)?
The drugs most often associated with NMS are antipsychotics (neuroleptic drugs). These drugs are used to treat mental health disorders such as schizophrenia and bipolar disorder. NMS happens due to blockage of dopamine receptors. Dopamine is a chemical messenger that helps convey messages between cells.
What drugs are associated with non-modular neurotransmitters?

Which medication poses the greatest risk for neuroleptic malignant syndrome?
Any antipsychotic drug can cause NMS. But stronger drugs, like fluphenazine and haloperidol, are more likely to trigger it.
Which increases the risk for neuroleptic malignant syndrome NMS )?
Risk factors The main risk factor for developing NMS is taking antipsychotic medication. While some more potent drugs may increase a person's risk, all antipsychotic medications can cause this condition. Taking more than one antipsychotic drug can also increase a person's risk of developing NMS.
Which of the following is most likely a cause of neuroleptic malignant syndrome?
Causes. Neuroleptic malignant syndrome comes about, most likely, as a result of “dopamine D2 receptor antagonism”. Dopamine is a chemical substance (neurotransmitter) found in the brain and elsewhere in the central nervous system that acts to convey messages from one cell to another.
Which drugs are neuroleptic drugs?
Common low-potency, first-generation neuroleptics include thioridazine, chlorpromazine, and thiothixene. Among second-generation medications, clozapine, olanzapine, paliperidone, and risperidone are the most frequently prescribed.
Can antidepressants cause neuroleptic malignant syndrome?
Neuroleptic malignant syndrome (NMS) is a rare condition that can happen when someone takes antipsychotic or antidepressant medications. People taking antipsychotic medications at high doses are more likely to develop NMS. NMS is life-threatening, and its treatment requires hospitalization.
Can SSRI cause NMS?
SSRIs may cause NMS by their facilitative action on neurotransmitter serotonin along with central dopaminergic blockade. Addition of SSRI to second-generation antipsychotic is also reported to increase the risk of NMS by inhibiting dopamine release by SSRIs.
What does NMS feel like?
Your doctor will look for the two main symptoms of NMS: a high temperature and stiff muscles. To be diagnosed with it, you also need to have a few other warning signs, like a fast heartbeat, low or high blood pressure, and sweating. Some other disorders have symptoms that are similar to NMS.
How do you test for neuroleptic malignant syndrome?
However, the following laboratory studies may be indicated, to assess severity and complications or rule out other diagnostic possibilities:Complete blood count (CBC)Blood cultures.Liver function tests (LFTs)Blood urea nitrogen (BUN) and creatinine levels.Calcium and phosphate levels.Creatine kinase (CK) level.More items...•
How do you diagnose neuroleptic malignant syndrome?
Diagnostic Considerations The diagnosis is confirmed by the presence of recent treatment with neuroleptics (within the past 1-4 weeks), hyperthermia (temperature above 38°C), and muscular rigidity, along with at least five of the following features: Change in mental status.
Why does neuroleptic malignant syndrome occur?
Scientists are still learning about the exact cause of neuroleptic malignant syndrome (NMS), but it's currently hypothesized that it's caused by dopamine D2 receptor antagonism. Dopamine is a neurotransmitter (chemical substance) that acts to convey messages from one cell to another.
What is the most common antipsychotic drug?
Haldol (haloperidol) and Thorazine (chlorpromazine) are the best known typical antipsychotics. They continue to be useful in the treatment of severe psychosis and behavioral problems when newer medications are ineffective. However, these medications do have a high risk of side effects, some of which are quite severe.
What is the most powerful antipsychotic drug?
Clozapine, which has the strongest antipsychotic effect, can cause neutropenia. A problem in the treatment of schizophrenia is poor patient compliance leading to the recurrence of psychotic symptoms.
What is neuroleptic malignant syndrome NMS?
INTRODUCTION Neuroleptic malignant syndrome (NMS) is a life-threatening neurologic emergency associated with the use of antipsychotic (neuroleptic) agents and characterized by a distinctive clinical syndrome of mental status change, rigidity, fever, and dysautonomia.
Why does neuroleptic malignant syndrome occur?
Scientists are still learning about the exact cause of neuroleptic malignant syndrome (NMS), but it's currently hypothesized that it's caused by dopamine D2 receptor antagonism. Dopamine is a neurotransmitter (chemical substance) that acts to convey messages from one cell to another.
Why do antipsychotics cause neuroleptic malignant syndrome?
These drugs block a brain chemical called dopamine. That can make your muscles stiff and can cause rigid movements in people with Parkinson's disease. Any antipsychotic drug can cause NMS. But stronger drugs, like fluphenazine and haloperidol, are more likely to trigger it.
What are the symptoms of NMS?
What are the symptoms of neuroleptic malignant syndrome?very high fever.rigid muscles.changes in mental state, such as agitation, drowsiness, or confusion.excessive sweating.rapid heartbeat.trouble swallowing.tremors.blood pressure abnormalities.More items...•
What is neuroleptic malignant syndrome?
Neuroleptic malignant syndrome (NMS) is a rare and life-threatening reaction to the use of any neuroleptic medication. Neuroleptics, also known as antipsychotic medications, treat and manage symptoms of many psychiatric conditions.
What are neuroleptic medications?
Neuroleptics, also known as antipsychotic medications, fall into two classes: first-generation or “typical” antipsychotics and second-generation or “atypical” antipsychotics.
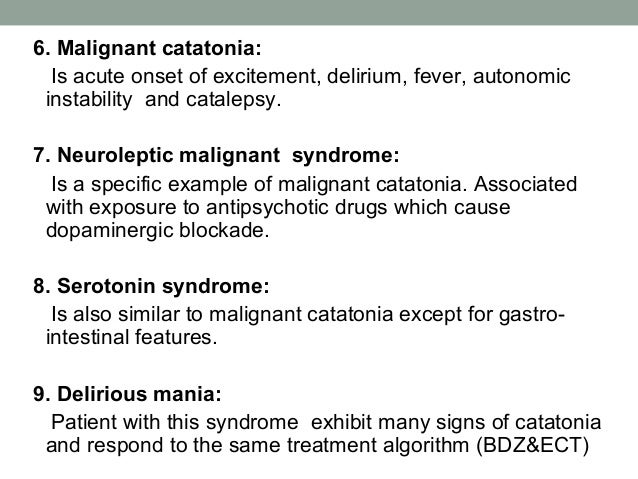
What is the difference between neuroleptic malignant syndrome and malignant hyperthermia?
Malignant hyperthermia is a rare and severe reaction to general anesthesia drugs and muscle relaxants.
What is the difference between neuroleptic malignant syndrome and serotonin syndrome?
Serotonin syndrome is caused by serotonergic agents such as antidepressants, amphetamines, antihistamines and mood stabilizers. Serotonin syndrome happens when there’s too much serotonin in your body.
Who does neuroleptic malignant syndrome affect?
Neuroleptic malignant syndrome (NMS) can affect anyone taking neuroleptic (antipsychotic) medications.
How common is neuroleptic malignant syndrome?
Neuroleptic malignant syndrome (NMS) is rare. Approximately 0.01% to 3.2% of people taking neuroleptic (antipsychotic) medications develop NMS.
What are the symptoms of neuroleptic malignant syndrome?
Symptoms of neuroleptic malignant syndrome typically develop over one to three days and include:
What is neuroleptic malignant syndrome?
Neuroleptic malignant syndrome (NMS) is a life-threatening syndrome associated with the use of dopamine-receptor antagonist medications or with the rapid withdrawal of dopaminergic medications. NMS has been associated with virtually every neuroleptic agent but is more commonly reported with the typical antipsychotics like haloperidol and fluphenazine. Classic clinical characteristics include mental status changes, fever, muscle rigidity, and autonomic instability. While uncommon, NMS remains an important part of the differential diagnosis of fever and mental status changes because it requires early diagnosis and treatment to prevent significant mortality and death. Treatment involves immediately discontinuing the offending agent, aggressive supportive care to manage and prevent complications, and pharmacologic therapy in severe cases. The empiric medications most frequently used for refractory NMS include bromocriptine mesylate, a dopamine agonist, and dantrolene sodium, a muscle relaxant. If the syndrome is due to the rapid withdrawal of dopaminergic medication, rapid re-institution of the medication may improve symptoms.[1][2][3]
What is the cause of NMS?
The primary trigger for NMS is dopamine receptor blockade, most often due to an antipsychotic agent. NMS is usually associated with high-potency first-generation neuroleptic agents but also may be caused by low-potency and atypical antipsychotic agents, antiemetics, tricyclic antidepressants, and lithium. Rapid withdrawal of dopaminergic drugs, most often used to manage parkinsonian diseases, such as levodopa and amantadine, also may cause this syndrome. The rapid switching of one Parkinson medication to another also is associated with the development of NMS. [4][5][6]
What are the symptoms of NMS?
The concurrent use of multiple neuroleptic agents or lithium also increases the risk. Abrupt withdrawal of dopaminergic agents is a less common but important cause of NMS. Symptoms of NMS develop over one to three days and include distinctive clinical features: fever, muscle rigidity, mental status changes, and autonomic rigidity.
What is the pathophysiology of NMS?
The pathophysiology of NMS is complex and incompletely understood. Most symptoms are attributed to the sudden reduction in central dopaminergic activity due to a D2 receptor blockade or abrupt withdrawal of D2 receptor stimulation. This accounts for the characteristic muscle rigidity, hyperthermia, and mental status changes. Other neurotransmitters are involved, and NMS has features suggestive of disruption of the sympathetic nervous system. Other theories suggest a calcium-mediated disruption of the musculoskeletal system, pathophysiologically similar to malignant hyperthermia. Familial clusters of patients with NMS and genetic testing suggest a predisposition to the development of NMS in certain individuals. [7][8][9]
How to treat NMS?
[10][11] This includes aggressive cooling and correction of volume deficits and any electrolyte imbalances. Patients are prone to cardiac dysrhythmias and respiratory failure due to chest wall rigidity. Treat with antiarrhythmic agents and mechanical ventilation as needed. More severe cases are managed with empiric pharmacologic therapy. Meta-analyses and case reports suggest that these may shorten the course and reduce morbidity and mortality. Bromocriptine, a dopamine agonist, given orally or via a gastric tube, is used to reverse the hypodopaminergic state. Dantrolene, a muscle relaxant may be administered intravenously or orally in less severe cases. Benzodiazepines also may be useful in controlling agitation. If the syndrome is due to a rapid withdrawal of dopaminergic agents, restarting the drug may reduce symptoms. Electroconvulsive therapy also has been reportedly effective in refractory cases. Patients should be admitted for close monitoring in an intensive care unit setting. [12]
Is the prognosis good after a drug is discontinued?
For most patients in whom the offending drug is discontinued, the prognosis is good. An interprofessional approach to the education of the family, monitoring, and treatment by clinicians, nurses, and pharmacists will provide the best outcomes. [Levell 5]
Is NMS a medical emergency?
NMS is a medical emergency that is best managed by an interprofessional team. These patients are ideally managed in the ICU with very close nursing monitoring and reporting to the team. A pharmacist trained in toxicology and a toxicologist should be involved in assisting with treatment and management decisions. The key is hydration and supportive therapy. There is no specific drug to reverse this disorder. Anecdotal reports on dantrolene continue to appear but a few case studies indicate that the drug may neither be effective or safe. [14]
Which neuroleptic drug is most commonly associated with NMS?
Potent typical neuroleptics such as haloperidol, fluphenazine, chlorpromazine, trifluoperazine, and prochlorperazine have been most frequently associated with NMS and thought to confer the greatest risk.
What is neuroleptic malignant syndrome?
Neuroleptic malignant syndrome (NMS) is a severe disorder caused by an adverse reaction to medications with dopamine receptor-antagonist properties or the rapid withdrawal of dopaminergic medications.
What is the next step in the management of NMS?
The next key step in the management of NMS is the initiation of supportive medical therapy. Aggressive hydration is often required, especially if highly elevated CPK levels threaten to damage the kidneys, and treatment of hyperthermia with cooling blankets or ice packs to the axillae and groin may be needed.
What are the laboratory findings of NMS?
Characteristic laboratory findings seen in NMS include elevated creatinine phosphokinase (CPK) due to rhabdomyolysis and leukocytosis, but these are neither specific for the syndrome nor present in all cases.14When rhabdomyolysis is present, it can be severe enough to cause renal failure, requiring hemodialysis.13Additional common laboratory abnormalities include a metabolic acidosis and iron deficiency.15The cerebrospinal fluid (CSF) and imaging studies are usually normal, but an electroencephalogram (EEG) may show nongeneralized slowing.7
What is the best treatment for NMS?
In more severe cases of NMS, empiric pharmacologic therapy is typically tried. The two most frequently used medications are bromocriptine mesylate, a dopamine agonist, and dantrolene sodium, a muscle relaxant that works by inhibiting calcium release from the sarcoplasmic reticulum.
What are the hallmarks of a CNS infection?
In addition to fever and mental status changes, hallmarks of a CNS infection include a history of prodromal illness, headaches, meningeal signs, focal neurological signs, seizures, and frequently positive CSF and neuroimaging studies.
Does levodopa cause NMS?
The abrupt cessation or reduction in dose of dopaminergic medications such as levodopa in Parkinson disease may also precipitate NMS.27The rapid switching from one type of dopamine receptor agonist to another in such patients has also been associated with NMS,28and there may be some risk of NMS associated with the abrupt withdrawal of Parkinson medications that are not known to have direct dopaminergic activity such as amantadine29and tolcapone.30Neuroleptic malignant syndrome has also been rarely associated with a number of other medications not known to have any central antidopaminergic activity such as lithium,31desipramine, trimipramine, dosulpin,32and phenelzine (Table 2).33
What is neuroleptic malignant syndrome?
Neuroleptic Malignant Syndrome (NMS) is a rare but potentially serious idiosyncratic reaction to drugs which is characterised by a tetrad of symptoms including altered mental status, fever, extrapyramidal symptoms, and autonomic instability.(1) For more information on the symptoms and diagnosis of NMS, please refer to Medicines Q&A number 309 ‘What is Neuroleptic Malignant Syndrome?’
When was metoclopramide first used?
The anti-emetic metoclopramide was first described as a cause for NMS in 1985.(25) A case report describes a six month old child with Freeman-Sheldon Syndrome who suffered NMS following administration of metoclopramide syrup. This is the youngest patient who has been reported to experience NMS, confirming that children are also at risk of developing the syndrome.(26)
When was olanzapine first reported?
Olanzapine induced NMS was first reported in 1998 and since then multiple case reports have linked olanzapine with NMS onset. Only a minority of these cases seem to suggest an atypical onset, with most cases describing typical NMS features.(4)
When was NMS first described?
NMS was first described in the literature in 1960, following the introduction of the first typical antipsychotic agents, originally known as neuroleptic drugs.(3, 4) Typical antipsychotic agents have been reported in the literature to cause NMS more frequently than other agents which may reflect their longer history of use, although it has proven difficult to estimate differences in incidence between the two groups.(5, 6) Use of high potency agents may be a risk factor for developing NMS.(1) Estimates of incidence of NMS with typical antipsychotics range from 0.2 to 1% of patients treated.(1,
Does lithium cause NMS?
In overdose, lithium alone has been reported to cause NMS, and lithium toxicity may contribute to an increased risk of permanent brain damage following an NMS episode.(28)
Can antidepressants cause NMS?
In cases reported following antidepressants alone, some of the diagnoses have been dubious. Tricyclic antidepressants (TCAs) appeared to be more likely to cause NMS than selective serotonin reuptake inhibitors. A review of the case reports concludes that NMS associated with antidepressants alone is a very rare occurrence, but that antidepressants may increase serum levels of antipsychotics, leading to an increased risk of NMS due to the antipsychotic itself.(22)
Does Amisulpride cause altered onset?
The limited numbers of cases of NMS reported with amisulpride appear to describe a slightly altered onset, in that more cases are reported in older patients, and cases seemed to appear more rapidly after initiation of the drug.(4, 9)
What is neuroleptic malignant syndrome?from verywellhealth.com
Neuroleptic malignant syndrome (NMS) is a reaction to some specific types of medications. It’s characterized by symptoms like very high fever, rigid muscles, and rapid heartbeat. Although rare, NMS is potentially life-threatening and requires prompt medical treatment. Read on to learn more about NMS, what causes it, and how it can be treated.
What is the difference between neuroleptic malignant syndrome and serotonin syndrome?from healthline.com
Neuroleptic malignant syndrome vs. serotonin syndrome. Serotonin syndrome (SS) is a condition that’s similar to NMS. It occurs when too much serotonin accumulates in the body. Like dopamine, serotonin is a chemical messenger that facilitates communication between cells. Like NMS, SS often occurs when beginning a new drug or increasing the dosage ...
What happens if you stop taking a dopamine blocker?from verywellhealth.com
If a person stops, steps down, or switches these types of medications, NMS might occur. In other words, NMS has its greatest potential risk when increasing the dose of a dopamine-blocking drug (like haloperidol) or decreasing the dose of a dopamine-stimulating drug. In both cases, a person is receiving less dopamine stimulation than before.
Why does NMS occur?from healthline.com
NMS happens due to blockage of dopamine receptors. Dopamine is a chemical messenger that helps convey messages between cells. It’s believed that drugs associated with NMS block dopamine receptors in the brain, leading to NMS symptoms. Although severe, NMS is rare. It’s estimated to occur in only 0.01 to 3.2 percent.
What causes NMS in Parkinson's patients?from healthline.com
NMS can also be caused by the rapid withdrawal of dopaminergic drugs. These drugs are often used to treat Parkinson’s disease. They increase dopamine-related activity in the brain and in rare cases abrupt withdrawal can cause NMS.
Why does dopamine trigger NMS?from verywellhealth.com
It probably involves a complex series of physiological events. The abrupt change in stimulation to dopamine receptors seems to dysregulate the autonomic nervous system (part of your body that regulates many unconscious bodily functions). This is what leads to problems such as increased pulse and breathing rate. Changes in dopamine may also lead to unexpected effects on muscle cells, triggering muscular rigidity. 4
What are the symptoms of NMS?from healthline.com
The concurrent use of multiple neuroleptic agents or lithium also increases the risk. Abrupt withdrawal of dopaminergic agents is a less common but important cause of NMS. Symptoms of NMS develop over one to three days and include distinctive clinical features: fever, muscle rigidity, mental status changes, and autonomic rigidity.