June 9, 2009 -- Genetic testing confirms that high levels of a type of cholesterol known as lipoprotein(a) are associated with an increased risk for heart attacks, but the clinical implications of the finding are unclear. Lipoprotein(a) has long been suspected of contributing to cardiovascular risk.
Does lipoprotein(a) contribute to heart disease?
However, some studies suggest that having high levels of lipoprotein (a) circulating in your blood could put you at a higher risk of developing heart disease. Made in your liver and then entering your bloodstream, lipoprotein (a) has been shown to build up under the inner lining of arteries.
Are high lipoprotein(a) concentrations associated with high risk of ischemic cardiovascular disease?
Background: High lipoprotein (a) concentrations present in 10%-20% of the population have long been linked to increased risk of ischemic cardiovascular disease. It is unclear whether high concentrations represent an unmet medical need.
What are the effects of high lipoprotein(A) levels?
Higher lipoprotein (a) levels have been shown to lower the chances of survival after a heart attack. Blood test findings for levels of lipoprotein (a) are expressed in milligrams per deciliter (mg/dL). A level of 30 mg/dL is considered normal. Levels higher than 30 mg/dL may indicate a 2- to 3-fold increased risk for heart disease.
Are lipoprotein cholesterol concentrations causal for different CVDs?
Mendelian randomization studies have shown that Lp(a) concentrations are causal for different CVDs, including coronary artery disease, calcified aortic valve disease, stroke, and heart failure, despite optimal low-density lipoprotein cholesterol (LDL-C) management. Lp(a) consists of apolipoprotein (apo) B100 covalently bound to apoA.
Is LDL a cardiovascular disease?
The fact is, elevated low-density lipoprotein (LDL), the bad cholesterol, is a major cause of heart disease. LDL causes the build-up of fatty deposits within your arteries, reducing or blocking the flow of blood and oxygen your heart needs. This can lead to chest pain and heart attack.
Does High HDL cause cardiovascular disease?
Higher levels of HDL have been associated with a lower risk of cardiovascular disease. However, pharmaceutical approaches to reduce heart disease risk by raising HDL levels have had disappointing results.
Does LDL increase CVD risk?
In addition to LDL-C, nonhigh-density lipoprotein cholesterol ≥160 mg/dL may also be considered as a risk factor for increased long-term risk of CVD and coronary heart disease mortality.
Can LDL and HDL be high?
Thyroid hormones help your body make and break down cholesterol. People whose thyroid gland is underactive, a condition called hypothyroidism, have higher levels of both HDL and LDL cholesterol.
Does low HDL cause heart disease?
Cholesterol is cholesterol. There are no symptoms associated with low HDL levels, but low HDL levels increase your risk for cardiovascular disease, which does have symptoms. Understanding what HDL is can help protect your health from illness like cardiovascular disease.
Which lipoprotein reduces the risk of cardiovascular disease?
HDL (high-density lipoprotein), or “good” cholesterol, absorbs cholesterol and carries it back to the liver. The liver then flushes it from the body. High levels of HDL cholesterol can lower your risk for heart disease and stroke.
What do LDL and HDL do?
HDL cholesterol can be thought of as the “good” cholesterol because a healthy level may protect against heart attack and stroke. HDL carries LDL (bad) cholesterol away from the arteries and back to the liver, where the LDL is broken down and passed from the body.
What is the relationship of HDL and LDL levels to cardiovascular disease?
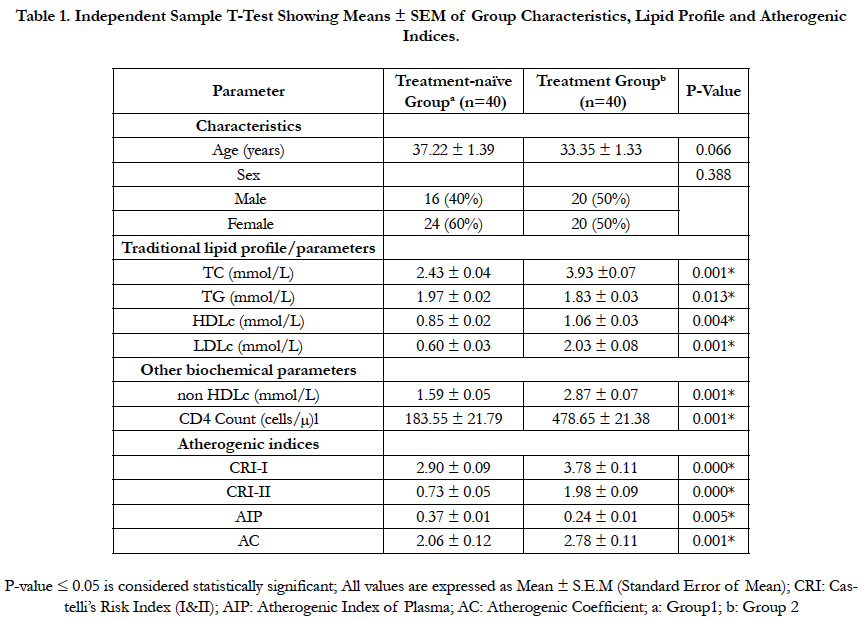
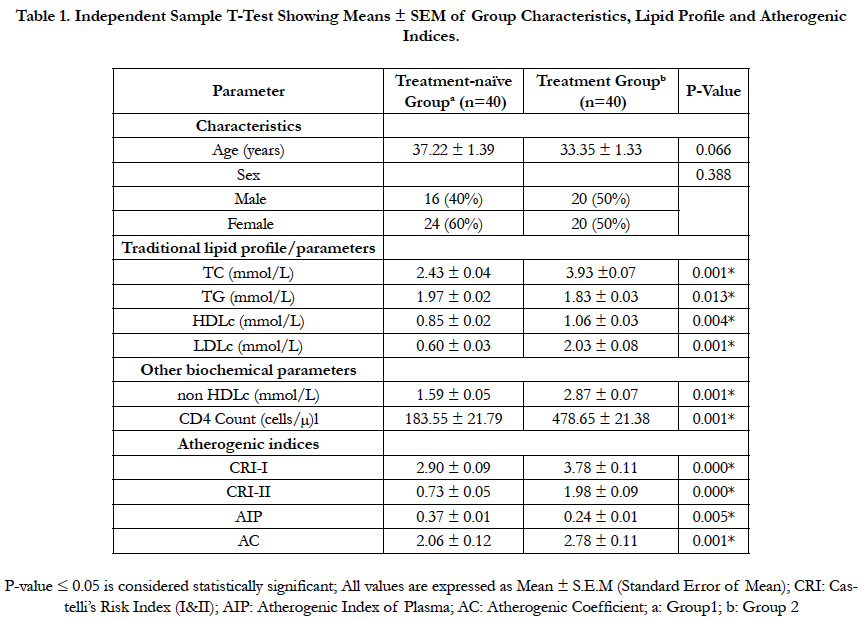
Lipoprotein cholesterol data from the Framingham Heart Study show that low-density lipoprotein (LDL) and high-density lipoprotein (HDL) cholesterol levels are important in determining risk for coronary artery disease (CAD). Increased LDL and decreased HDL cholesterol levels are associated with an increase in CAD.
What is the relationship of HDL levels to cardiovascular disease?
The cholesterol contained within HDL is inversely associated with risk of coronary heart disease and is a key component of predicting cardiovascular risk. However, despite its properties consistent with atheroprotection, the causal relation between HDL and atherosclerosis is uncertain.
Does High HDL prevent heart disease?
Generally speaking, cholesterol in LDL is linked to increased risk while cholesterol in HDL is associated with protection against heart disease.
What does it mean if you have a high HDL level?
For HDL cholesterol, or "good" cholesterol, higher levels are better. High-density lipoprotein (HDL) cholesterol is known as the "good" cholesterol because it helps remove other forms of cholesterol from your bloodstream. Higher levels of HDL cholesterol are associated with a lower risk of heart disease.
How high is too high for HDL?
Our HEART UK experts say the protective effect of HDL cholesterol appears to reach its maximum at roughly 1.4mmol/L, and higher levels may not provide extra protection. Over 2.3mmol/L, HDL may behave more like LDL cholesterol (or 'bad cholesterol') and raise the risk of disease, according to current research.
What are the risk factors for heart disease?
For most of the general population, these numbers, along with an assessment of risk factors, such as blood pressure, body mass index (BMI), and smoking status, are a good determination of risk. Over the past few years, more emphasis has been placed on the role of lipoprotein (a), or Lp (a), which greatly increases the risk for premature cardiovascular disease (CVD), especially when it is combined with other risk factors.
What are the different types of lipoproteins?
Lipoproteins are particles that carry cholesterol and triglycerides through the bloodstream. Chylomicrons (which carry triglycerides), VLDL, LDL, and HDL are all types of lipoproteins, and each of these has subtypes of lipoproteins. Lp (a) is a subtype of LDL lipoprotein that is associated with increased inflammation and atherosclerosis. It is found in very small amounts in most people, but about 1 in 5 individuals worldwide, or about 63 million people in the United States1 has a genetic trait that causes them to have much higher levels of Lp (a).
What causes LPA?
Inherited Lp (a) is caused by a genetic mistake or Single Nucleotide Polymorphism (SNP) in the apo (a) LPA gene.4 It affects all ethnic groups but is more common in African Americans and South Asians.1 Those with a family history of early CVD or heart attack in men younger than 50 years and women younger than 60 years are at greatest risk.
What is lipoprotein A?
Made in your liver and then entering your bloodstream, lipoprotein (a) has been shown to build up under the inner lining of arteries. This buildup may contribute to the development of atherosclerosis — the formation of fatty plaques in your arteries that can lead to heart disease, heart attack, and stroke — by promoting arterial inflammation ...
What percentage of the population has lipoprotein A?
That’s because 1) not enough is known about lipoprotein (a)’s effect on heart health and 2) it’s found in only about 15% of the general population, with persons of non-Hispanic Caucasian, Chinese, and Japanese origins having the lowest levels.
Which cholesterol is most damaging to the arterial walls?
High levels of lipoprotein (a) are believed to be most damaging to arterial walls when LDL cholesterol is also high.
What is the name of the protein that is bonded to the lipoprotein?
Lipoprotein (a), also known as Lp (a), is low-density lipoprotein (LDL, or “bad” cholesterol) that has another form of protein, called a glycoprotein, bonded to it. (The name of this glycoprotein is apolipoprotein (a). )
What does 30 mg/dL mean in blood test?
A level of 30 mg/dL is considered normal. Levels higher than 30 mg/dL may indicate a 2- to 3-fold increased risk for heart disease.
Is lipoprotein a back burner?
However, it’s not routinely used for that purpose. If you’re trying to lower your risk of developing heart disease, it’s best to put lipoprotein (a) on the treatment “back burner” for now and focus instead on methods for reducing the well-established risk factors for heart disease.
Can you check your lipoprotein levels?
That said, there are a few situations where it may be best to routinely check lipoprotein (a) levels. Mainly, these are when a person has: Diagnosed heart disease and normal levels of HDL, LDL, and triglycerides. A strong family history of heart disease but, again, normal HDL, LDL, and triglyceride levels.
What is the LPA gene?
The LPA gene controls the formation of the lipoprotein (a) molecule. Variants in the gene cause the body to create more Lp (a). These first two genetic variants cover about 40% of the variation in Lp (a) levels — there are other, less common variants that also raise Lp (a) levels.
What is Lp (a)?
Lipoprotein (a) or LP (a) — said “L- P- little a” — is a blood particle that carries LDL cholesterol and proteins. Elevated levels of Lp (a) are a strong risk factor for having a heart attack due to atherosclerosis. [ ref]
What is C/T risk?
C/T: risk of elevated Lp (a), increased risk for heart disease, increased risk of aortic stenosis
How many people die from heart disease in the US?
Heart disease is the number one cause of death in the US and in most countries around the world. Statistics show that one in four people in the US will die of heart disease. We often have a picture in our heads of someone at risk for a heart attack: an obese, older man who looks unhealthy, probably with a stressful job.
Does lipoprotein increase atherosclerosis?
It also promotes clotting by interfering with the way that the body dissolves clots. [ ref] So, you have a double-whammy of increasing atherosclerosis via increased inflammation plus oxidized LDL. The LDL has a tendency to oxidize once inside a vessel wall adding more inflammation responses because their structure has changed. This all adds to a mechanism that increases the risk of blood clots. [ ref]
Is lipoprotein a genetic risk?
Lipoprotein (a): A big genetic risk for heart disease . By reading this information, you could possibly save your life today. This isn’t a scare tactic or overblown “health-alert!” type of article – just statistics and solid genetics research on the increased risk of cardiovascular disease.
Does carrying one risk allele for both of the above double the risk of aortic stenosis?
Studies also showed that carrying one risk allele for both of the above — compound heterozygous — also doubled the risk of aortic stenosis. [ ref]
How does lipoprotein affect cardiovascular disease?
Evidence from mechanistic, observational, and genetic studies support a causal role of lipoprotein (a) in the development of cardiovascular disease, including coronary heart disease and peripheral arterial disease, as well as aortic valve stenosis, and likely also ischemic stroke. Effect sizes are most pronounced for myocardial infarction, peripheral arterial disease, and aortic valve stenosis where high lipoprotein (a) concentrations predict 2- to 3-fold increases in risk. Lipoprotein (a) measurements should be performed using well-validated assays with traceability to a recognized calibrator to ensure common cut-offs for high concentrations and risk assessment. Randomized cardiovascular outcome trials are needed to provide final evidence of causality and to assess the potential clinical benefit of novel, potent lipoprotein (a) lowering therapies.
What is lipoprotein A?
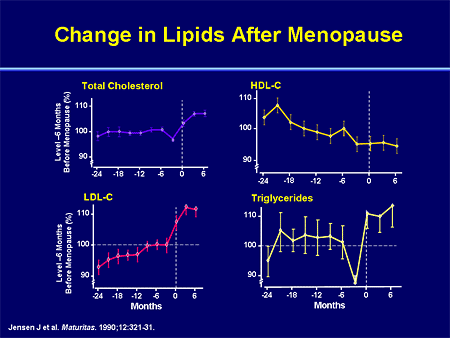
Lipoprotein (a) is a unique liver-derived lipoprotein with primarily genetically determined concentrations and large interindividual concentration variation with values ranging from <1 to >200 mg/dL in the general population ( Fig. 1) ( 3 ); an estimated approximately 20% of the population have high concentrations corresponding to >42 mg/dL total mass lipoprotein (a) in a Danish general population cohort and using a lipoprotein (a) assay traceable to an international calibrator. Notably, lipoprotein (a) concentration distributions vary with race/ethnicity with individuals of African descent having on average higher concentrations than individuals of European or Asian descent ( 3 ). High lipoprotein (a) concentrations have long been linked to increased risk of ischemic CVD and, in particular, coronary heart disease (CHD) ( 3, 5 ). In the past decade, high concentrations have additionally been associated with increased risk of aortic valve stenosis (AVS) ( 6–8 ), heart failure ( 9 ), and low concentrations, paradoxically, with increased risk of type 2 diabetes (T2D) ( 10 ).
When was lipoprotein first described?
Lipoprotein (a) was first described in 1963 as a distinct beta-lipoprotein ( 26) and in the following years numerous studies on lipoprotein (a) were published, many of which were observational epidemiologic studies of lipoprotein (a) concentrations and CVD risk. While initial smaller cross-sectional studies generally demonstrated increased risk at high concentrations, the first large prospective studies published in the early nineties yielded null findings for atherosclerotic disease and myocardial infarction (MI) ( 27, 28 ), in retrospect likely due to the use of poor measurement methods. Thus, scientific interest in lipoprotein (a) was severely dampened, as demonstrated by the subsequent decrease in lipoprotein (a) publications. More recent large prospective general population studies (e.g., the Copenhagen City Heart Study, Fig. 2) using fresh samples and well-validated assays have since then documented marked, independent, and stepwise increases in risk of CHD with increasing lipoprotein (a) concentrations ( 29 ). In 2009, results from prospective studies were summarized in a large individual participant data meta-analysis by the Emerging Risk Factors Collaboration documenting robust and independent, albeit moderate, increases in risk of non-fatal MI and coronary death with increasing concentrations of lipoprotein (a) (13% increased risk per 1 SD higher concentration) and also increased risk of ischemic stroke (IS) (10% increased risk per 1 SD higher concentration) ( 30 ). Importantly, while the meta-analysis primarily included studies conducted in whites, other ethnic/racial groups were represented, and no evidence of differences in risk estimates in different ethnic/racial groups was found, consistent with subsequent findings from the Atherosclerosis Risk in Communities Study where associations with cardiovascular outcomes were at least as strong in blacks with 2- to 3-fold higher median concentrations compared to whites ( 31 ). Of note, the reported risk estimates from the meta-analysis likely represent minimal estimates as early (false) negative studies were included. Nonetheless, the meta-analysis together with the subsequent publication of two large genetic epidemiologic studies, causally implicating high lipoprotein (a) concentrations in ischemic CVD ( 22, 23), generated renewed interest in lipoprotein (a) as an emerging risk factor and possible new target for treatment.
Which protein is involved in fibrinolysis?
In vitro and animal studies have indicated that lipo protein (a), with similar kringle structures and an inactive protease region, inhibits fibrinolysis through competitive inhibition of plasmin activation and function, thus ultimately promoting thrombosis ( 11, 12 ). It is, however, unclear if this mechanism of competitive inhibition is active in vivo in humans, as plasminogen is generally in large molar excess of lipoprotein (a).
Is VTE associated with LPA?
The abovementioned findings for atherosclerotic disease and VTE are generally consistent with results from large studies examining the associations of LPA SNPs with CVD (50,51); Helgadottir et al. combined 35 case-control series to detect increased risk of PAD, abdominal aortic aneurism, and IS subtype large artery atherosclerosis in minor allele carriers of LPA rs10455872 and/or rs3798220 associated with increased lipoprotein (a) concentrations ( 51 ). However, no association with VTE, carotid intima media thickness, IS subtype cardioembolic, or small vessel disease was found. Likewise, in the Women’s Health Study (n = 21 000) no association with VTE for either of these SNPs (nor lipoprotein (a) concentrations) was found ( 52 ). Thus, large genetic epidemiologic studies have not been able to provide unequivocal evidence of causal associations of lipoprotein (a) with risk of VTE ( 24, 51) despite clear prothrombotic effects of lipoprotein (a) demonstrated in experimental studies ( 3, 11, 12 ), and despite positive findings in meta-analyses of observational studies ( 53 ).
Is low lipoprotein a causality?
Further support for a causal association of lipoprotein (a) with risk of CHD has come from studies documenting decreased risk in carriers of loss-of-function LPA variants associated with low lipoprotein (a) concentrations ( 41, 42 ). In the PROCARDIS study ( 41) including circa 4000 cases and a similar number of controls, carriers had on average 39% lower median lipoprotein (a) concentrations and 21% decreased risk of CHD, indicating the potential therapeutic benefit of lowering lipoprotein (a) concentrations. Similarly, in a very large genetic study (n > 100 000) by Emdin et al., a gene risk score based on 4 LPA SNPs, strongly associated with low plasma lipoprotein (a) concentrations, predicted a 29% decrease in risk of CHD (and decreased risk of peripheral arterial disease (PAD), AVS, heart failure, and stroke) per one SD genetically lowered lipoprotein (a) concentrations ( 43 ). Finally, convincing evidence of causality has been provided by recent Mendelian randomization studies using genetic data to estimate the lipoprotein (a) lowering required to result in clinically meaningful CVD risk reductions given future therapeutic options ( 40, 44, 45 ).
Is lipoprotein a risk factor for CHD?
In 2009, two large genetic epidemiologic studies were published that collectively implicated lipoprotein (a) as a causal risk factor for CHD ( 22, 23 ). First, a classic Mendelian randomization study of >40 000 individuals demonstrating increased risk of MI as a function of both increased lipoprotein (a) concentrations and low number of LPA KIV2 repeats, associated with increased concentrations ( 22 ). A clear stepwise increase in risk with higher lipoprotein (a) concentrations and corresponding lower number of LPA KIV2 repeats was seen. Upon instrumental variable analysis, a doubling in lipoprotein (a) concentrations was associated with an approximate 20% increase in risk of MI. Second, a large case-control study including 3100 CHD cases genotyped for circa 49 000 genetic variants in 2100 candidate genes, identifying (with replication in an additional circa 4800 cases) two LPA SNPs (the intronic rs10455872 and the missense rs3798220), as having the strongest association with risk of CHD ( 23) of all SNPs tested. In a subset of participants, SNP carriers vs. noncarriers had higher lipoprotein (a) concentrations, lower numbers of LPA KIV2 repeats, and smaller isoform size. Combined, these 2 genetic epidemiologic studies provided strong genetic evidence of a causal association of lipoprotein (a) with CHD consistent with data from previous studies on apolipoprotein (a) phenotype and CHD risk ( 3) and purely genetic studies, including genome-wide association studies, identifying the LPA gene locus, and some studies specifically the LPA rs3798220 SNP, as being associated with increased risk of CHD ( 34–39 ). In follow-up studies on the Copenhagen general population cohorts, high lipoprotein (a) concentrations and corresponding LPA risk genotypes were associated also with cardiovascular (and all-cause) mortality and with recurrent major adverse cardiovascular events providing genetic evidence of causality also in recurrent CVD ( 25, 40 ).
What is the molecule that is synthesized by the liver?
Lipoprotein(a)(Lp[a]) is a low density lipoprotein (LDL)– like particle synthesized by the liver that consists of an apolipoprotein B100 (apo B100) molecule covalently linked to a very large glycoprotein known as apolipoprotein(a) (apo[a]).1-3The physiological and vascular effects of the particle remain uncertain, but Lp(a) has been shown to enter the arterial intima of humans4; in vitro and animal studies have reported that Lp(a) can promote thrombosis, inflammation, and foam cell formation.5-7
Why do bnumbers sum to less than the total of CHD events?
bNumbers sum to less than the total of CHD events because 1 study46did not provide seperate data on CHD death and nonfatal MI.