When is fibrinolytic therapy indicated in suspected acute stroke?
Probable acute ischemic stroke; consider fibrinolytic therapy. If the CT scan shows no sign of hemorrhage, it is probable that the patient experienced an ischemic stroke and is a candidate for fibrinolytic therapy.
What are the guidelines for fibrinolytic therapy for atrial fibrillation (AFIB)?
If the patient remains a candidate for fibrinolytic therapy, review the risks and benefits of the therapy with the patient and their family within 1 hour of arrival and 3 hours of symptom onset. If they agree to the treatment, administer rtPA and do not give the patient anticoagulants or antiplatelets for 24 hours.
When is a patient not a good candidate for fibrinolytic therapy?
If the patient had a witnessed seizure when symptoms started and neurological impairments are evident following the seizure, the patient may not be considered to be a good candidate for fibrinolytic therapy.
What is fibrinolytic therapy for blood clot?
Fibrinolytic therapy — or thrombolytic therapy — is an emergency treatment used to dissolve blood clots before they become fatal. If you or a loved one has a heart attack, stroke or another condition caused by a blood clot, fibrinolytic therapy can help prevent death and reduce long-term side effects.
Who is a candidate for thrombolytic therapy?
Thrombolytic therapy is used only to treat an ischemic stroke in people who do not have other bleeding disorders, among other criteria. A stroke is damage to the brain caused by interruption in the brain's blood supply. Stroke is a medical emergency and one of the leading causes of death and adult disability.
What are contraindications to fibrinolytic therapy?
Contraindications to Fibrinolytic TherapyAbsolute contraindicationsAortic dissectionActive internal bleeding (not menses)Intracranial tumorPericarditisRelative contraindicationsBlood pressure > 180/110 mm Hg after initial antihypertensive therapy8 more rows
How do you determine if a patient is a candidate for fibrinolytic therapy for stroke?
If the CT scan shows no evidence of hemorrhage, the patient may be a candidate for fibrinolytic therapy (Boxes 6 and 8). If hemorrhage is noted on the CT scan, the patient is not a candidate for fibrinolytic therapy. Consult a neurologist or neurosurgeon and consider transfer as needed for appropriate care (Box 7).
When is fibrinolytic therapy indicated?
Fibrinolytic therapy is the treatment of choice for STEMI patients who meet specific criteria: Patient has been symptomatic (Chest pain) for longer than 15 minutes but less than 12 hours. ECG is diagnostic for ST elevation indicating an MI or a new Left Bundle Branch Block.
Who is not a candidate for tPA?
Other Contraindications for tPA Arterial puncture at a noncompressible site in the previous 7 days. History of previous intracranial hemorrhage. Intracranial neoplasm, AVM, or an aneurysm. Recent intracranial or intraspinal surgery.
Who is not eligible for thrombolytic therapy?
Patients who have uncontrolled hypertension with a systolic blood pressure of greater than 180 mm Hg or a diastolic of greater than 110 mm Hg may also be excluded. Blood glucose levels are also taken into consideration. A glucose concentration of less than 50 mg/dL is considered a contraindication.
What requires fibrinolytic therapy?
Fibrinolytic therapy is used in the treatment of a ST segment elevation myocardial infarction (STEMI), acute stroke and other less common indications such as pulmonary embolism and acute deep venous thrombosis. During STEMI, fibrinolytic therapy must be instituted within 24 hours of symptom onset.
When should fibrinolytic therapy be administered in stroke?
As a result, intra-arterial fibrinolytic therapy is commonly administered as an off-label therapy for stroke at tertiary centers within 6 hours of onset in the anterior circulation and up to 12-24 hours after onset in the posterior circulation.
When can you not give fibrinolytic therapy?
The contraindications for fibrinolytic therapy include previous intracranial hemorrhage, malignant intracranial neoplasm, known structural cerebrovascular lesion (e.g., arteriovenous malformation), ischemic stroke within 3 months except for acute ischemic stroke within 4.5 h, significant facial trauma or closed-head ...
Which of the following is an absolute contraindication for receiving fibrinolytic therapy?
Absolute contraindications for fibrinolytic use in STEMI include the following: Prior intracranial hemorrhage (ICH) Known structural cerebral vascular lesion. Known malignant intracranial neoplasm.
When is a fibrinolytic checklist required?
If cardiopulmonary resuscitation was administered for >10 min. Major surgery within the last three weeks. Internal bleeding within the last two to four weeks. Vascular punctures that could not be compressed if they were to start bleeding.
When is fibrinolytic therapy indicated in ACS?
Fibrinolytic therapy is currently indicated, in the absence of contraindications (Table 1), for patients with STEMI who have experienced symptom onset within the previous 12 hours and in whom electrocardiography (ECG) demonstrates ST-segment elevation of more than 0.1 mV in at least 2 contiguous precordial leads or at ...
When can you not give fibrinolytic therapy?
The contraindications for fibrinolytic therapy include previous intracranial hemorrhage, malignant intracranial neoplasm, known structural cerebrovascular lesion (e.g., arteriovenous malformation), ischemic stroke within 3 months except for acute ischemic stroke within 4.5 h, significant facial trauma or closed-head ...
Which of the following are considered as an absolute contraindication to thrombolytic therapy in MI select all that apply?
Answer. Absolute contraindications for fibrinolytic use in STEMI include the following: Prior intracranial hemorrhage (ICH) Known structural cerebral vascular lesion.
Why is fibrinolytic contraindicated in Nstemi?
In NSTEMI the blood flow is present but limited by stenosis. In NSTEMI, thrombolytics must be avoided as there is no clear benefit of their use. If the condition stays stable a cardiac stress test may be offered, and if needed subsequent revascularization will be carried out to restore a normal blood flow.
Why is thrombolytic therapy contraindicated in hypertension?
Background. Intravenous thrombolysis (IVT) with (recombinant) tissue plasminogen activator is an effective treatment in acute ischemic stroke. However, IVT is contraindicated when blood pressure is above 185/110 mmHg, because of an increased risk on symptomatic intracranial hemorrhage.
What is the purpose of fibrolytic therapy?
Fibrinolytic Therapy Contraindications. The goal of stroke care is to minimize injury to the brain and prevent neurological deficits. Identifying symptoms of a stroke quickly and seeking prompt treatment can improve prognosis and maximize patient recovery. Fibrinolytic therapy can be a lifesaving treatment for stroke.
How does fibrolytic therapy work?
Fibrinolytic therapy works by dissolving clots which are obstructing blood flow to the brain. In order to be considered a suitable candidate for the therapy, patients must be over the age of 18 and have a firm diagnosis of ischemic stroke with deficits.
Is intracranial hemorrhage a contraindication for fibrinolytic therapy?
In addition, since intracranial hemorrhage is also a possible complication of fibrinolytic therapy, conditions that increase the risk of a hemorrhage are also viewed as fibrinolytic therapy contraindications. For example, if the patient has a history of a previous stroke within the past three months, it may increase their risk ...
Is fibrinolytic therapy contraindicated?
Although fibrinolytic therapy may be the recommended treatment, in some cases the risks outweigh the benefits and the therapy is contraindicated. A thorough assessment of the patient’s condition and medical history is an essential part of determining if fibrinolytic therapy is appropriate. There are several absolute and relative contraindications ...
Can you use fibrinolytics on a CT scan?
If a patient has a clinical presentation suggestive of a subarachnoid bleed, such as severe headache, orbital pain, vision loss, and dizziness, even with a normal CT scan, treatment with a fibrinolytic agent may not be advised . A previous subarachnoid bleed is also considered a contraindication.
Can fibrinolytic therapy be used for myocardial infarction?
Myocardial infarction within the previous three months may also exclude a patient from fibrinolytic therapy. Additional relative contraindications include major trauma or surgery within the previous two weeks or recent gastrointestinal hemorrhage. This is due to the increased risk of bleeding.
Can fibrinolysis be used for ST elevation?
Fibrinolysis can be effective for the treatment of ST-segment elevation myocardial infarction. The medication can dissolve the thrombus/embolus that is lodged in a coronary artery, thus restoring blood flow to the heart.
Can you give fibrinolysis before a cardiac event?
This is because several studies have shown that fibrinolytic agents given to people who are suffering from an acute cardiac event have better outcomes if they receive fi brinolysis (a clot-busting drug) before they reached the hospital. This is especially true in rural settings where the time to reach a hospital can be substantial. However, this may also apply in urban settings where wait times in emergency departments can be equally substantial.
What is the purpose of fibrinolytic agents?
Rationale: The administration of a fibrinolytic agent results in the lysis of the acute thrombus, thus recanalizing, or opening, the obstruct ed corona ry artery and restoring blood flow to the affected tissue. After perfusion is restored, adjunctive measures are taken to prevent further clot formation and reocclusion.
What happens if a cardioverter defibrillator is programmed to defibrill?
Rationale: If the dysrhythmia deteriorates into ventricular fibrillation , the implantable cardioverter defibrillator is programmed to defibrillate at a higher energy. If the dysrhythmia terminates spontaneously, the device will not discharge.
What is TAVR surgery?
Transcatheter aortic valve replacement (TAVR) is a transformational therapy for patients who have severe aortic stenosis but who are extremely high-risk surgical candidates or who are inoperable by virtue of associated co-morbidities. A patient is diagnosed with third-degree heart failure.
Can a nurse monitor for bleeding?
Rationale: The nurse must continually monitor for clinical manifestations of bleeding. Mild gingival bleeding and oozing around venipuncture sites are common and not causes for concern. However, severe lower back pain and ecchymoses are suggestive of retroperitoneal bleeding. If serious bleeding occurs, all fibrinolytic heparin therapies are discontinued, and volume expanders, coagulation factors, or both are administered.
How long to review fibrinolytic therapy?
If the patient remains a candidate for fibrinolytic therapy, review the risks and benefits of the therapy with the patient and their family within 1 hour of arrival and 3 hours of symptom onset. If they agree to the treatment, administer rtPA and do not give the patient anticoagulants or antiplatelets for 24 hours.
What to do if CT scan indicates hemorrhage?
Consult a neurologist or neurosurgeon. If the CT scan indicates hemorrhage, consult neurologists and neurosurgeons, and begin the stroke or hemorrhage pathway.
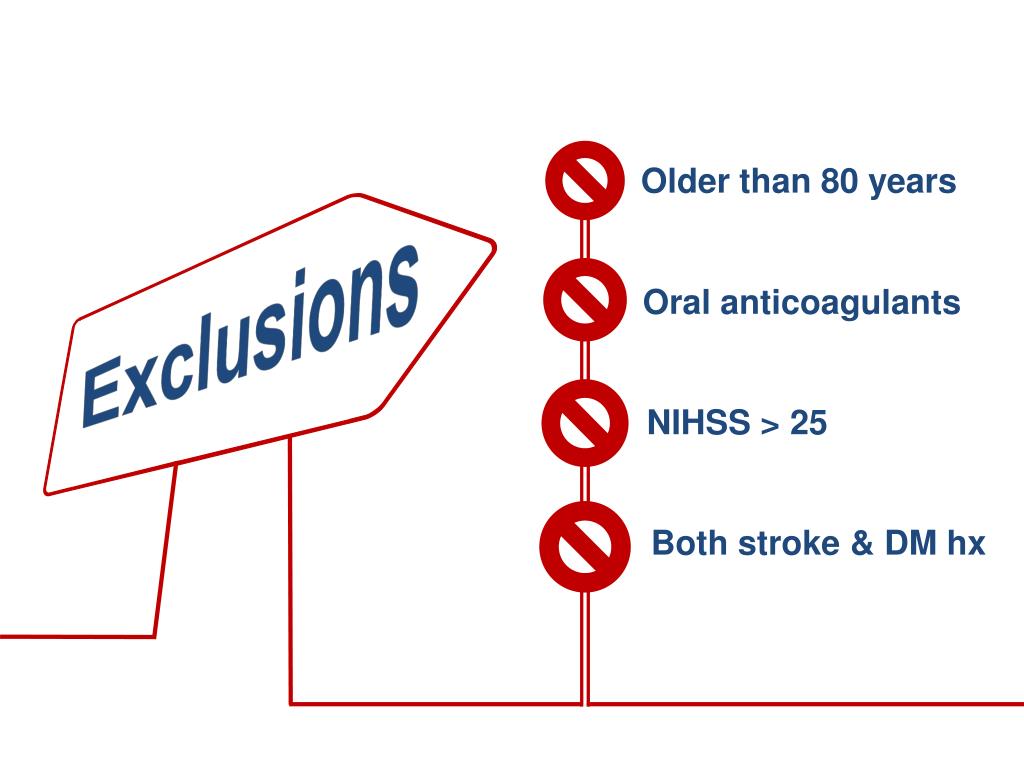
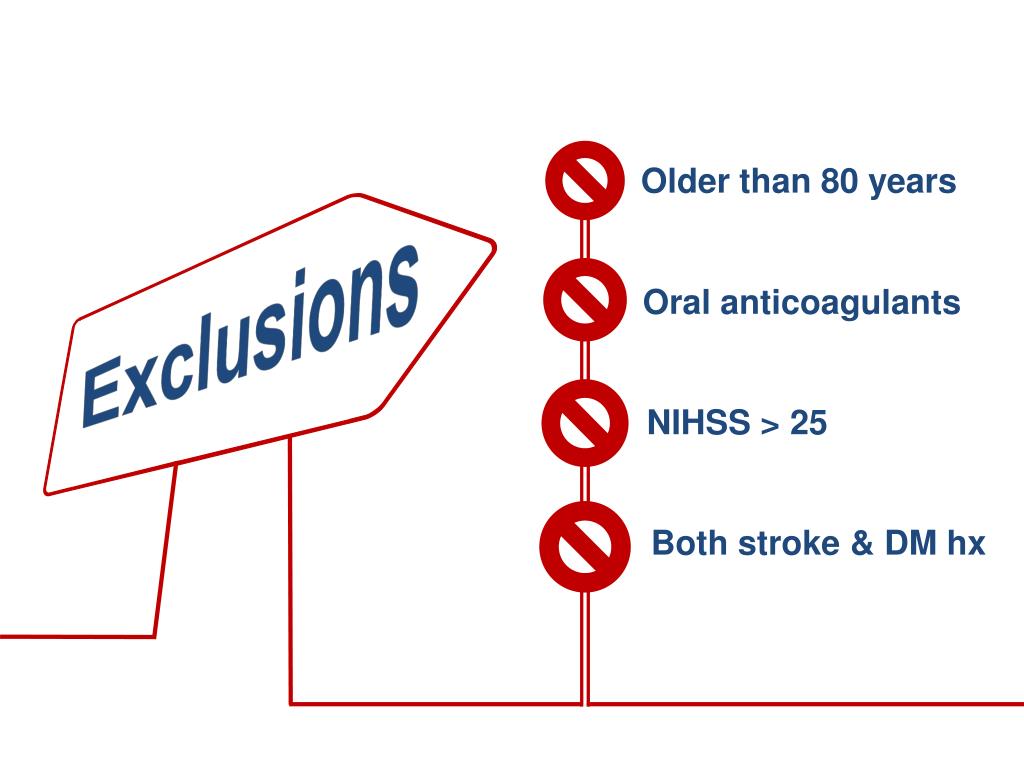
Can fibrinolytic therapy be used for ischemic stroke?
Probable acute ischemic stroke; consider fibrinolytic therapy. If the CT scan shows no sign of hemorrhage, it is probable that the patient experienced an ischemic stroke and is a candidate for fibrinolytic therapy. Check for fibrinolytic exclusions such as significant head trauma or stroke in the previous 3 months, history of intracranial hemorrhage, elevated blood pressure, active internal bleeding, or a blood glucose concentration less than 50 milligrams per deciliter. Then repeat the neurologic exam.
When should thrombolytic therapy be administered?
Thrombolytic therapy must be administered as early as possible after symptoms of an ischemic stroke to achieve maximum benefits. After an ischemic stroke, neurons in the core ischemic region are likely to suffer irreversible damage that results in tissue death (infarction).
What are the benefits and risks of thrombolytic therapy?
The primary benefit of thrombolytic therapy is improved chances of functional recovery after a stroke by revitalizing the penumbral neurons. Earlier the therapy is initiated, higher the chances of recovering most of the functional abilities.
What is the goal of early thrombolytic therapy for ischemic stroke?
The goal of early thrombolytic therapy is to salvage the brain cells (neurons) that have suffered only partial damage, and limit the injury to the brain . Thrombolytic therapy must be administered as early as possible after symptoms of an ischemic stroke to achieve maximum benefits.
How is thrombolytic therapy performed?
Thrombolytic therapy is administered intravenously or intra-arterially depending on the location of the clot. Ideally, the medication must be administered as quickly as possible after patient admission. The important steps taken during a thrombolytic therapy include:
What is the prognosis for ischemic stroke after thrombolytic therapy?
Following is the approximate prognosis for ischemic stroke patients, based on patient data recorded three months after their thrombolytic stroke therapy:
What is the treatment for a thrombolytic stroke?
Thrombolytic therapy is a treatment to break up the blood clot in the brain’s blood vessel which caused the ischemic stroke. An enzyme known as tissue plasminogen activator (tPA) is administered to dissolve the blood clot and restore normal blood flow to the brain.
How long after stroke can you get thrombolytic therapy?
The American Heart Association/American Stroke Association (AHA/ASA) recommends the following eligibility criteria for administration of thrombolytic therapy within three hours after symptoms of ischemic stroke: