Substances from the blood can easily pass through the peritoneum
Peritoneum
The peritoneum is the serous membrane forming the lining of the abdominal cavity or coelom in amniotes and some invertebrates, such as annelids. It covers most of the intra-abdominal organs, and is composed of a layer of mesothelium supported by a thin layer of connective tissue. This peritoneal lining of the cavity supports many of the abdominal organs and serves as a conduit for their blood ves…
What substances cannot pass through the peritoneal membrane?
Peritoneal membranes allow the passage of amino acids, polypeptides, and plasma proteins. Glucose, creatinine, and fatty acids cannot permeate the peritoneal membrane. ... The nurse is preparing to perform peritoneal dialysis for a patient with chronic kidney disease. Which osmotic agent will the nurse obtain for the dialysis exchanges?
Which osmotic agent will the nurse obtain for peritoneal dialysis?
Glucose, creatinine, and fatty acids cannot permeate the peritoneal membrane. ... The nurse is preparing to perform peritoneal dialysis for a patient with chronic kidney disease. Which osmotic agent will the nurse obtain for the dialysis exchanges? Dextrose is the most commonly used osmotic agent used in peritoneal dialysis.
What is the pathophysiology of peritonitis?
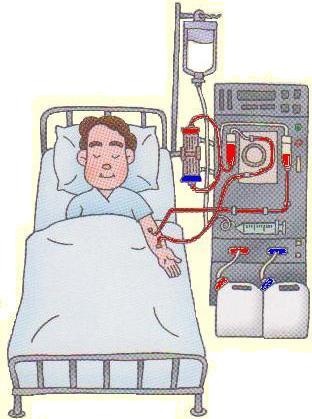
Peritonitis results from contamination or from progression of an exit site or tunnel infection. Exit site infection is caused by infection of the peritoneal catheter. Hepatitis and hypotension are complications of hemodialysis. A patient who has been on hemodialysis for several weeks asks the nurse what substances are being removed by the dialysis.
What is the function of the peritoneal membrane?
How is excess fluid removed from the peritoneal membrane?
What causes peritoneal effluent to be cloudy?
What is the primary clinical manifestation of peritonitis?
Why does my peritoneum hurt?
Can you drink breakfast on hemodialysis?
Does PD restrict potassium intake?
See 2 more
About this website
What type of fluid is used in peritoneal dialysis?
In peritoneal dialysis, the inside lining of your own belly acts as a natural filter. Wastes are taken out by means of a cleansing fluid called dialysate, which is washed in and out of your belly in cycles.
Is the peritoneal membrane permeable?
The two main properties of the peritoneal membrane are: a. Semi permeable – this allows substances of certain sizes to move from an area of greater concentration to less concentration.
What is membrane permeability in peritoneal dialysis?
Peritoneal membrane permeability determines the rate of solute equilibration between body fluids and the solution within the peritoneal cavity and is, therefore, a significant determinant of the solute removal rate.
Can you remove fluid with PD?
Peritoneal dialysis (PD) removes waste and extra fluid through the blood vessels that line the walls of your abdomen.
Where is the peritoneal membrane?
abdominal cavityThe peritoneum is the serous membrane that lines the abdominal cavity. It is composed of mesothelial cells that are supported by a thin layer of fibrous tissue and is embryologically derived from the mesoderm.
What is the peritoneum and what is its function?
What is the peritoneum? Your peritoneum is a membrane, a sheet of smooth tissue that lines your abdominopelvic cavity and surrounds your abdominal organs. It pads and insulates your organs, helps hold them in place and secretes a lubricating fluid to reduce friction when they rub against each other.
How is peritoneal fluid reabsorbed?
The three-pore model of peritoneal fluid transport predicts that once the osmotic gradient has dissipated, fluid reabsorption will be due to a combination of small-pore reabsorption driven by the intravascular oncotic pressure, and an underlying disappearance of fluid from the cavity by lymphatic drainage.
What is ultrafiltration in peritoneal dialysis?
Ultrafiltration is the removal of fluid from a patient and is one of the functions of the kidneys that dialysis treatment replaces. Ultrafiltration occurs when fluid passes across a semipermeable membrane (a membrane that allows some substances to pass through but not others) due to a driving pressure.
Which electrolyte is not added to peritoneal dialysis solutions?
Chronic patients that have been stabilized on peritoneal dialysis therapy should have routine evaluation of electrolyte blood chemistries and hematologic factors measured in order to determine the patient's ongoing condition. peritoneal dialysis solutions do not include potassium.
What dialysis Cannot remove?
Dialysis can't replace hormones Unfortunately, dialysis cannot replace or manufacture these chemicals. These will need to be replaced in the body with medication.
What toxins are removed during dialysis?
The most common toxins removed by hemodialysis were lithium and ethylene glycol. There were more dialysis treatments for poisonings with valproate and acetaminophen in 2001-2005 than for methanol and theophylline, although hemodialysis for acetaminophen removal is generally not recommended.
What is removed during dialysis?
Hemodialysis removes extra potassium, which is a mineral that is normally removed from your body by your kidneys. If too much or too little potassium is removed during dialysis, your heart may beat irregularly or stop.
What is the use of peritoneal membrane?
The peritoneal membrane is the smooth, transparent membrane that lines the abdominal cavity and contains the internal organs of the abdomen and pelvis, such as the stomach and large intestine. The peritoneal membrane helps to protect and separate the internal structures of the abdomen and pelvis.
What is the difference between peritoneum and omentum?
Peritoneum is a serous membrane lining the abdominal cavity. Omentum is a fold of the peritoneal layer. It may be two-layered or four-layered with patches that give it a lacy appearance. The parietal peritoneum lines the pelvic and abdominal cavities.
What is the purpose of cutting through peritoneal membrane?
Cutting through the transparent membrane gives access to some of the internal abdominal organs. The cavity is dominated by the liver (large, brown organ at anterior of cavity) and the small intestine, but the large intestine may be visible.
What is the peritoneal lining?
Your peritoneum is the tissue that lines your abdominal wall and covers most of the organs in your abdomen. A liquid, peritoneal fluid, lubricates the surface of this tissue.
What is the function of the peritoneal membrane?
Peritoneal membranes allow the passage of amino acids, polypeptides, and plasma proteins. Glucose, creatinine, and fatty acids cannot permeate the peritoneal membrane. A patient has undergone successful kidney transplantation but develops a sudden rapid decrease in urine output five days after the surgery.
How is excess fluid removed from the peritoneal membrane?
In PD, excess fluid is removed by increasing the osmolality of the dialysate (osmotic gradient) through the addition of glucose. Excess water is removed when there is an osmotic gradient or pressure gradient across the membrane. The addition of glucose does not affect the shift of potassium into the cells. Excess serum potassium is removed by dialyzing with a potassium-free solution, not glucose. Heating the dialysate encourages removal of serum urea by dilatation of peritoneal blood vessels.
What causes peritoneal effluent to be cloudy?
Peritonitis is caused by either a Staphylococcus aureus or a Staphylococcus epidermidis infection. It is manifested by abdominal pain, cloudy peritoneal effluent, and increased white blood cell count. Oliguria, hyperkalemia, and hyponatremia are complications associated with acute kidney injury.
What is the primary clinical manifestation of peritonitis?
The primary clinical manifestations of peritonitis are abdominal pain and cloudy peritoneal effluent with a white blood cell (WBC) count greater than 100 cells/L (more than 50% neutrophils). An activated immune response may attract WBCs, and an elevated level of WBC in the peritoneal fluid indicates peritonitis.
Why does my peritoneum hurt?
Cloudy peritoneal effluent. Peritonitis may manifest as vomiting due to the inflammatory process in the peritoneum. The patient may have pain in the abdomen due to peritoneal irritation caused by the inflammatory process in the peritoneum. The primary clinical manifestations of peritonitis are abdominal pain and cloudy peritoneal effluent ...
Can you drink breakfast on hemodialysis?
The patient may even take liquid or powdered breakfast drinks in case of inadequate protein intake. Patients on hemodialysis have a more restricted fluid intake than patients receiving peritoneal dialysis (PD). The nurse is caring for a patient undergoing peritoneal dialysis.
Does PD restrict potassium intake?
The patient undergoing regular peritoneal dialysis (PD) does not need to restrict potassium intake; instead, this patient may be prescribed oral potassium supplementation because of hypokalemia caused by dialysis. The patient need not restrict protein or fluid intake. The patient should include enough protein in the diet to compensate for loss of protein in dialysate. The patient may even take liquid or powdered breakfast drinks in case of inadequate protein intake. Patients on hemodialysis have a more restricted fluid intake than patients receiving peritoneal dialysis (PD).
What is the function of the peritoneal membrane?
Peritoneal membranes allow the passage of amino acids, polypeptides, and plasma proteins. Glucose, creatinine, and fatty acids cannot permeate the peritoneal membrane. A patient has undergone successful kidney transplantation but develops a sudden rapid decrease in urine output five days after the surgery.
How is excess fluid removed from the peritoneal membrane?
In PD, excess fluid is removed by increasing the osmolality of the dialysate (osmotic gradient) through the addition of glucose. Excess water is removed when there is an osmotic gradient or pressure gradient across the membrane. The addition of glucose does not affect the shift of potassium into the cells. Excess serum potassium is removed by dialyzing with a potassium-free solution, not glucose. Heating the dialysate encourages removal of serum urea by dilatation of peritoneal blood vessels.
What causes peritoneal effluent to be cloudy?
Peritonitis is caused by either a Staphylococcus aureus or a Staphylococcus epidermidis infection. It is manifested by abdominal pain, cloudy peritoneal effluent, and increased white blood cell count. Oliguria, hyperkalemia, and hyponatremia are complications associated with acute kidney injury.
What is the primary clinical manifestation of peritonitis?
The primary clinical manifestations of peritonitis are abdominal pain and cloudy peritoneal effluent with a white blood cell (WBC) count greater than 100 cells/L (more than 50% neutrophils). An activated immune response may attract WBCs, and an elevated level of WBC in the peritoneal fluid indicates peritonitis.
Why does my peritoneum hurt?
Cloudy peritoneal effluent. Peritonitis may manifest as vomiting due to the inflammatory process in the peritoneum. The patient may have pain in the abdomen due to peritoneal irritation caused by the inflammatory process in the peritoneum. The primary clinical manifestations of peritonitis are abdominal pain and cloudy peritoneal effluent ...
Can you drink breakfast on hemodialysis?
The patient may even take liquid or powdered breakfast drinks in case of inadequate protein intake. Patients on hemodialysis have a more restricted fluid intake than patients receiving peritoneal dialysis (PD). The nurse is caring for a patient undergoing peritoneal dialysis.
Does PD restrict potassium intake?
The patient undergoing regular peritoneal dialysis (PD) does not need to restrict potassium intake; instead, this patient may be prescribed oral potassium supplementation because of hypokalemia caused by dialysis. The patient need not restrict protein or fluid intake. The patient should include enough protein in the diet to compensate for loss of protein in dialysate. The patient may even take liquid or powdered breakfast drinks in case of inadequate protein intake. Patients on hemodialysis have a more restricted fluid intake than patients receiving peritoneal dialysis (PD).