
Who is allowed to give consent for medical treatment?
In the case of children, parents or guardians must usually give consent for medical treatment, or in mentally incompetent adults, an appointed guardian, who may or may not be a relative, would need to give permission for treatment.
Who cannot give informed consent?
No other person or body authorised by law to make decisions for the patient can give or refuse informed consent to treatment. Thismeans that a guardian or a person responsible under the Guardianship and Administration Act 1986 or an agent under the Mental Treatment Act 1988 cannot give or refuse informed consent on behalf of a patient.
What medical procedures require consent?
Medical procedures that may require you to give written informed consent include: Most surgeries, even when they are not done in the hospital. Other advanced or complex medical tests and procedures, such as an endoscopy (placing a tube down your throat to look at the inside of your stomach) or a needle biopsy of the liver.
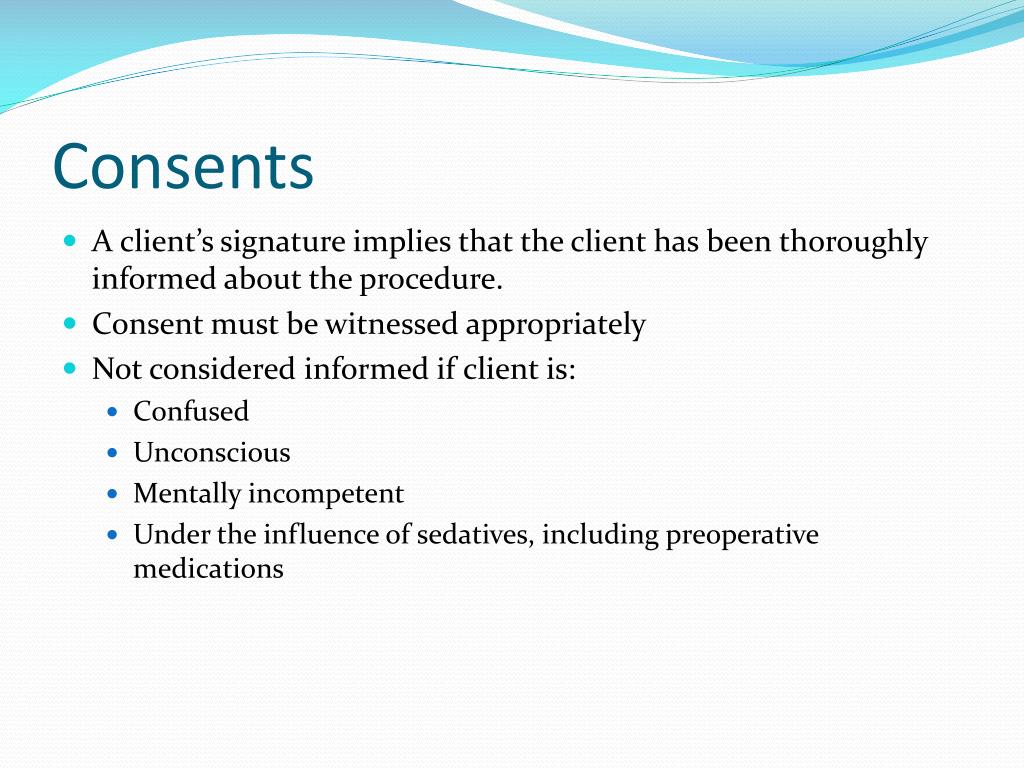
What do you need to know about informed consent?
- Identify an appropriate person to provide informed consent for the client (e.g., client, parent, legal guardian)
- Provide written materials in the client's spoken language, when possible
- Describe components of informed consent
- Participate in obtaining informed consent
- Verify that the client comprehends and consents to care and procedures
Who Cannot sign an informed consent?
Children and Informed Consent Children (typically under 17) cannot provide informed consent.
Who is responsible for obtaining informed consent from the patient?
physicianTHE DUTY TO OBTAIN INFORMED CONSENT The duty to obtain a patient's consent for treatment rests on the patient's treating physician (6). Hospitals, nurses, surgical assistants, and referring physicians do not owe this duty to their patients (7).
Can family members give informed consent?
In case of incapacitated persons, close family members or legal guardians can give consent. Adequate information should be provided to a prudent patient during informed consent.
Can a nurse sign an informed consent?
The nurse's role in structured informed consent processes has technical and professional components. Technically, the nurse serves as a witness to the patient (or proxy) signing the form, but nurses don't abdicate their professional responsibility or commitment to the patient in those moments.
Which of the following persons can legally give informed consent?
The patient or their legal representative must give consent voluntarily and without any coercion by others. They must also ask questions and clarify things until they are certain about the procedure, the benefits, the risks, and possible alternatives.
Who can witness an informed consent?
Any member of the healthcare team may sign as a witness to the patient's signature, although this serves only to verify that it was the patient who signed the form. The witness does not obtain consent or verify the patient's competency to give consent.
What are the 3 main requirements of valid consent?
An effective consent process needs to address three elements: Capacity — who can give informed consent? Disclosure — what information do patients need? Voluntariness — are they giving consent freely?
What are 3 things a person must be to give consent?
The individual is adequately informed before giving consent; The consent is specific; The consent is current; and. The individual has the capacity to understand and communicate their consent.
What are the two exceptions to informed consent?
There are two well-recognized exceptions to the need for informed consent to medical treatment. The more common is a medical emergency, in which an unconscious or delirious patient cannot consent. The second is rare and involves certain court-ordered treatments or treatments and tests mandated by law.
Can a nurse take consent?
Nurses have a legal duty to ensure they obtain informed consent from their patients before carrying out any intervention or treatment.
Can a nurse sign for a patient?
What is it? Signature recognition refers to state laws that authorize nurse practitioners (NPs) to sign or otherwise complete forms related to patient care within their scope of practice.
What is the nurse's role for consent?
Nurses may serve to ensure patient comprehension, facilitate documentation of consent, address patient anxiety, and identify the appropriate surrogate decision-maker when needed [10].
Who is legally responsible for obtaining informed consent from a patient quizlet?
The physician who is performing the biopsy is responsible for providing informed consent to the patient about the procedure. The nurse is responsible for witnessing the signing of the consent. The patient must be 18 years or older and legally competent to give and/or refuse consent.
Who is responsible for obtaining the person's informed consent quizlet?
Who's responsibility is obtaining informed consent? The health care professional performing the procedure or treatment. Assumed when, during a life threatening emergency, consent cannot be obtained from the patient or family.
Who is responsible for informed consent quizlet?
- A competent client older than 18 years must sign the consent form. - The primary health care provider performing the procedure is responsible for obtaining informed consent.
What is consent to treatment?
Patient Consent to Treatment. Every human being of adult years and sound mind has a right to determine what shall be done with his/her own body [i]. All types of medical treatment require a patient’s consent. Consent is the permission necessary to start treatment.
What is consent given without knowing its dangers?
A consent given without knowing its dangers and the degree of danger, is a consent that does not represent a choice and is inadequate [vi]. Only the physician giving treatment or performing an operation has a duty to inform the patient of the risks involved.
What is consent in medical terms?
Consent is the permission necessary to start treatment. Medical ethics and international human rights law necessitate consent as a prerequisite for initiating medical treatment. The essentials of a valid consent are: Consent must be voluntarily made; The patient must be informed of all the information regarding the treatment before the application;
What is express consent?
Express consent is given to carry out a specific action. Implied consent can be inferred from their actions, the facts and circumstances of a particular situation. Implied consent can be obtained from a patient’s silence. There is no legal requirement to obtain written consent from a patient for medical treatment.
Why do doctors give information about a particular treatment?
Doctors give information about a particular treatment or test in order that a patient can decide whether or not to undergo such treatment or test. This process of understanding the risks and benefits of treatment is known as informed consent. It is based on the moral and legal premise of patient autonomy.
Which state requires a physician to obtain the signature of the patient to a statement containing an explanation of the procedure?
For example the state of Nevada requires a physician to obtain the signature of the patient to a statement containing an explanation of the procedure, alternative methods of treatment, and risks involved [iv]. The principles governing consent for medical treatment are: consent must be valid;
Is consent necessary in an emergency?
Moreover, in case of an emergency, consent is not necessary [ii]. In case of an emergency, a surgeon can operate on a child without waiting for authority from the parents where it appears impracticable to secure consent [iii]. Consent can be either explicit or implied.
What is consent form?
This form is a legal document that shows your participation in the decision and your agreement to have the procedure done.
Why is informed consent required in research?
It informs the participants about the trial and lets them make educated decisions about taking part in the study. The process is similar to informed consent in healthcare. In a research setting, it involves discussing the following:
When a healthcare provider recommends a specific procedure, do you have the right to accept or refuse it?
If you decide to move forward, you’ll need to give informed consent first.
What to do if you have questions about your medical care?
As the patient, you have the right to make informed choices about your medical care and what works best for you.
What does it mean when you sign a medical form?
When you sign the form, it means: You received all the relevant information about your procedure from your healthcare provider. You understand this information. You used this information to determine whether or not you want the procedure. You agree, or consent, to get some or all of the treatment options.
What is the role of medical information in decision making?
your understanding of the medical information. your voluntary decision to get treatment. These components are essential elements of the shared decision-making process between you and your healthcare provider. Most importantly, it empowers you to make educated and informed decisions about your health and medical care.
What to do if you don't want a procedure?
If you don’t want a procedure or treatment, you can choose to not sign the form. Your healthcare provider won’t be able to provide specific types of treatment if you don’t agree to it.
What is consent to treatment?
Consent to treatment is the agreement that an individual makes to receive medical treatment, care, or services, including tests and examinations. Anyone who can independently decide whether they want treatment must provide consent.
What is informed consent?
Informed consent requires the healthcare professional to provide information that outlines what the treatment entails, the benefits and risks, and other potential treatment options. They must also explain to the person the possible outcomes of refusing the recommended treatment.
How old do you have to be to get Gillick treatment?
Children under the age of 16 years can consent to treatment on their own if healthcare professionals decide that they have Gillick competence, which is the intelligence and capacity to understand fully what the treatment entails. Individuals without this ability require consent from a person with parental responsibility.
What is the obligation of healthcare professionals?
Healthcare professionals have an ethical and legal obligation to disclose information related to various treatment options to help people make an informed choice. This includes the risks, possible outcomes, and alternative options, if they are available. Healthcare providers can provide information verbally or in writing. They may also provide audio or video materials.
What does it mean when you don't have the mental capacity to comprehend treatment choices?
In these cases, the healthcare team must make the decisions that best serve the interests of the individual.
What is nonverbal consent?
Nonverbal consent, sometimes called implied or implicit consent, includes gestures such as nodding the head, extending the arm for a blood test, or opening the mouth during a dental exam. Doctors may refer to verbal consent as explicit consent.
What is written consent?
Written consent involves completing and signing a consent form, which is a legal document that gives the doctor permission to proceed with the treatment. Consent forms ensure that doctors provide the appropriate information related to the medical condition and treatment options and that the individual selects their preferred option.
How old do you have to be to give consent to a patient?
In most states, age 18 is the age of majority and thus, before treating a patient under the age of 18, consent must be obtained from the patient’s parent or legal guardian. This seems relatively straightforward; however, with today’s reality of blended families and children being chauffeured around by nannies and other caregivers, it is not always easy to determine who is accompanying the patient and whether he or she has legal authority to grant consent. In order to avoid confusion, consider the following:
What is the age limit for minors to consent to treatment?
In several states, such as Vermont and California, this right is granted to minors as young as 12.2
What to do if a minor is in custody of a legal guardian?
If the minor is in the custody of a legal guardian, ask for proof of guardianship before treating.
When a parent or guardian is not available to give consent and a delay in treatment would be life answer?
When a parent or guardian is not available to give consent and a delay in treatment would be life-threatening or cause the patient serious harm, consent is presumed. To the extent feasible, however, consent should be obtained for any resultant ongoing treatment.
When a minor is allowed to consent to treatment, a conversation should occur in which the minor’s expectations regarding?
When a minor is allowed to consent to treatment, a conversation should occur in which the minor’s expectations regarding privacy are discussed. Typically, the right to consent to treatment goes hand-in-hand with the right to confidentiality. While it is important to honor a patient’s privacy rights, a minor’s health situation may be such that it is preferable (or even necessary) to make the minor’s parents aware. As such, minor patients should be told up front that there may be times when you will not be able to honor their requests for confidentiality. “In cases when the physician believes that without parental involvement and guidance, the minor will face a serious health threat, and there is reason to believe that the parents will be helpful and understanding, disclosing the problem to the parents is ethically justified. When the physician does breach confidentiality to the parents, he or she must discuss the reasons for the breach with the minor prior to the disclosure.”3
Who is the legal guardian of a minor?
There may be minor patients for whom a guardian ad litem or legal guardian has been appointed to represent the interests of the minor. In these instances, it is often a state agency that has legal custody of the minor and is the legal guardian. The responsibilities and limits of authority of the guardian will be stated in a court order. Obtain a copy of the court order and examine it carefully prior to treatment to determine any limits on the ability of the legal guardian to consent to treatment of the minor patient.
Can a minor consent to a psychiatrist?
When allowing a minor to consent to treatment, it is important to remember that although a minor may meet the legal criteria for granting consent, a psychiatrist should still satisfy him or herself that the minor patient possesses the capacity and maturity to understand to what he or she is consenting. Thoroughly document under what circumstances the minor is being allowed to consent to treatment on his or her own behalf.
When should consent be obtained?
Consent should be obtained for all major therapeutic and diagnostic procedures (except emergencies) where disclosure of significant medical information, including major risks involved, would assist a patient in making an intelligent decision about the proposed procedure.
Who is responsible for obtaining informed consent?
Physicians are responsible for obtaining their patient's informed consent, although others may assist in facilitating and documenting consent. Any other physicians (particularly house staff) involved in obtaining consent must be sufficiently knowledgeable about the procedure in order to adequately communicate the risks, benefits, and alternatives.
What to address in informed consent discussion?
During the informed consent discussion, address the most serious risks, the less serious risks with a high likelihood of occurring, and any other risks to which your patient attaches significance. Enter documentation of the discussion on either the form or in the patient's medical record.
What to do if a patient refuses life saving treatment?
If you, and other clinicians involved, believe a patient who is refusing life saving treatment may not be fully competent, you may need to proceed without a completed consent form. Fully document your decision and your reasons. You may also want to contact your risk manager or institutional legal department.
What is consent in medical terms?
Consent is given voluntarily, without coercion, and may be withdrawn. The patient is competent and able to understand the nature and consequences of the proposed treatment or procedure.
Why is informed consent important?
Ideally, informed consent discussions build trust and reduce surprise and disappointment if complications or adverse events occur. Informed consent covers general issues of managing an illness and specific procedures being proposed. Completion of a consent form is necessary for most invasive procedures.
Why is it important to document informed refusal?
Documentation of the informed refusal is also crucial to support the clinical decision making.
Who must sign the informed consent or parental permission document?
When a written consent or parental permission form is used that embodies some or all of the elements of informed consent required by the regulations at 45 CFR 46.116, the regulations only require that the informed consent or parental permission document be signed by the subjects or the subjects' legally authorized representatives or by the parents of children who are subjects ( 45 CFR 46.117 (a)) and 45 CFR 46.408 (d) ). Only in situations where a short form is used, stating that the elements of informed consent required by 45 CFR 46.116 have been presented orally to the subject or the subject’s legally authorized representative or to the parent (s) of a child who is a subject, are there additional requirements for signatures ( 45 CFR 46.117 (b) (2) ).
What is informed consent and when, why, and how must it be obtained?
When informed consent is required, it must be sought prospectively, and documented to the extent required under HHS regulations at 45 CFR 46.117. [Food and Drug Administration (FDA) regulations at 21 CFR part 50 may also apply if the research involves a clinical investigation regulated by FDA.]
What are the basic elements of informed consent?
The basic required elements of informed consent can be found in the HHS regulations at 45 CFR 46.116 (a). Also see OHRP Informed Consent Tips.
Should the initial consent or parental permission procedure ever be repeated or supplemented?
Likewise, for research involving children, permission of the potential subjects' parents or guardians must be obtained ( 45 CFR46.408 (c) ), unless an IRB has waived this requirement. Ensuring an adequate consent or parental permission process may require repeating or supplementing the initial consent procedure. The regulations also stipulate that “An investigator shall seek such consent only under circumstances that provide the prospective subject or the representative sufficient opportunity to consider whether or not to participate and that minimizes the possibility of coercion or undue influence” ( 45 CFR 46.116 ). This requirement also might necessitate repeating or supplementing the initial consent procedure.
How far in advance of research participation can consent be obtained?
The HHS regulations at 45 CFR part 46 do not specify how far in advance of study entry a subject can provide consent. The amount of time required by a subject to make a decision would presumably depend on the nature of the study, taking into account, among other factors, the degree of risk, potential benefits, alternatives, and desire to consult with family members or others. However, if a prolonged period of time elapses from the date of consent to the date of entry into the study even if there have been no changes in the study design or no new significant findings affecting the study it might be prudent to review the information contained in the consent form with the subject prior to initiating any research procedures with the subject.
Can records or databases be reviewed to identify potential subjects without obtaining informed consent or parental permission?
Yes, under certain circumstances. Although the HHS regulations do not specifically reference this type of activity, sometimes referred to as “preparatory to research,” such an activity must be reviewed and approved by an IRB in accordance with HHS regulations at 45 CFR 46.109 (a) when:
How can the consent and parental permission processes be designed to facilitate understanding?
The procedures used in obtaining informed consent and parental permission should be designed to inform the subject population or the parents of the subject population about the research in terms that they can understand. Therefore, informed consent and parental permission language and its documentation in the accompanying forms (especially explanation of the study’s purpose, duration, experimental procedures, alternatives, risks, and benefits) should be provided in language that is understandable and culturally sensitive to those being asked to participate or provide permission for their child’s participation.
Why are minors allowed to provide consent for treatment of alcohol and drug related issues and STDs under the law?
Minors are allowed to provide consent for treatment of alcohol and drug related issues and STDs under the law because the law wants to protect them. Sexual health problems are confidential and providers will work with the adolescent to treat something like chlamydia without informing the patient's parents.
What is the law of unconscious consent?
The law assumes that an unconscious patient would consent to emergency care if the patient were conscious and able to consent. This is a "reasonable man" standard; that is the law assumes that reasonable person would want medical care in an emergency.
What is the age of consent for a minor?
A minor is someone who is under the age of 18 (unless laws where you live say differently). Therefore, someone who is 18 is at the age of majority and may sign consent for his or her parents. It has to do with being legally recognized as an adult.
How old do you have to be to sign consent in Nebraska?
Has 11 years experience. Unless it is a state where 19 is the age of majority, like Nebraska, an18 year old can legally sign consent on behalf of their incapacitated parent (though medication, injury,illness, etc). Though a spouse is first choice.
What happens if a parent is unable to sign?
For those who don't have any of those and are unable to sign their own consent, the court can appoint someone to act on the patient's behalf. In the case of emergency, implied consent is used.
What is implied consent?
In the case of emergency, implied consent is used. Say someone comes in unconscious with a gunshot to the chest, is actively dying, and will die without surgical intervention. That patient is taken into surgery without a signed consent form. This is why it is important for everyone to set up a health care POA.
Can implied consent overrule explicit rejection of medical care?
The health care providers may rely upon implied consent only in the absence of consent. Implied consent can never overrule the explicit rejection of medical care.
