When were evaluation and management codes developed?
1995E/M standards and guidelines were established by Congress in 1995 and revised in 1997. It has been adopted by private health insurance companies as the standard guidelines for determining type and severity of patient conditions.
Who created the CPT?
the American Medical Association (AMA)The Current Procedural Terminology (CPT®) system, developed by the American Medical Association (AMA), is used for just these purposes.
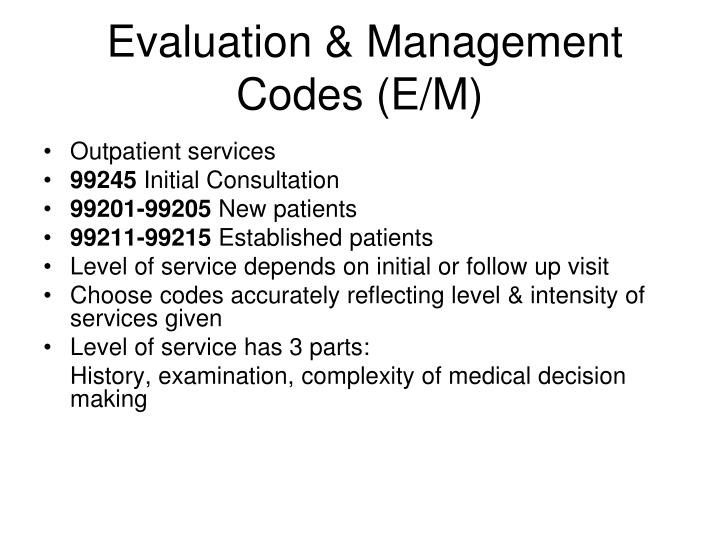
What are Evaluation and management CPT codes?
99202 to 99499Evaluation and management codes, often referred to as E&M codes or E and M codes are a coding system that involve the use of CPT codes from the range 99202 to 99499 which represent services provided by a physician or other qualified healthcare professional.
What is an E&M code?
Evaluation and management (E/M) coding and billing are crucial to maintaining the efficiency and productivity of a medical practice today. E&M coding involves use of CPT codes ranging from 99202 to 99499. These represent services by a physician (or other health care professional) in which the pr.
Who owns the CPT system?
the American Medical AssociationThe Current Procedural Terminology (CPT) code set, created and maintained by the American Medical Association, is the language of medicine today and the code to its future.
How was CPT created?
In 1965, the AMA recognized the need for common language and helped create the Current Procedural Terminology (CPT) system to describe medical services and procedures. The first edition of CPT was published in 1966 and, for the most part, was focused on surgery.
What is the difference between E&M codes and CPT codes?
E/M stands for “evaluation and management”. E/M coding is the process by which physician-patient encounters are translated into five digit CPT codes to facilitate billing. CPT stands for “current procedural terminology.” These are the numeric codes which are submitted to insurers for payment.
Are E&M codes the same as CPT codes?
E/M services represent a category of Current Procedural Terminology (CPT) codes used for billing purposes. Most patient visits require an E/M code.
Can you bill an E&M with a procedure?
You can bill an E/M and a minor procedure (procedure with 0 or 10 global days) on the same calendar date. The writer quoted the CMS Claims Processing Manual. The same language is in the CMS manual and the NCCI manual.
Who can bill EM codes?
PhysiciansReimbursement Guidelines CPT guidance instructs that E/M (CPT codes 99091, 99202-99499) should only be reported by Physicians or other qualified health care professionals.
What services do evaluation and management codes report?
As the name E/M indicates, these medical codes apply to visits and services that involve evaluating and managing patient health. Examples of E/M services include office visits, hospital visits, home services, and preventive medicine services.
What are the requirements for E M coding?
The seven components to the code selection are:The extent of History.The extent of Exam.The extent of Medical Decision Making.New or established patient.Nature of the presenting problem.Counseling or coordination of care.Amount of time spent with the patient.
Why was CPT codes created?
The Current Procedural Terminology (CPT®) codes offer doctors and health care professionals a uniform language for coding medical services and procedures to streamline reporting, increase accuracy and efficiency.
WHO publishes Current Procedural Terminology CPT )? Quizlet?
Published in 1966 by AMA. It provides a uniform language that describes medical, surgical, and dx svcs. to facilitate communication among providers, patients, and insurers. CPT organizes category 1 procedures and services within six sections, including the Index as the seventh section.
What are the historical facts of CPT coding?
CPT History In 1966, the AMA published the first edition of CPT, which at that time focused on surgical procedures. The first edition sought to standardize terminology and reporting. The second edition, in 1970, expanded CPT's scope. The third and fourth editions were released in the 1970's.
What coding system was created in 1984?
Common Lisp was introduced in 1984. Gene Dolgoff created the first digital projector in 1984.
When selecting E/M code level based on the three key components of history, exam, and MDM, what?
When selecting E/M code level based on the three key components of history, exam, and MDM, pay attention to whether the code requires you to meet the stated levels for three out of three or two out of three key components.
How many components are in an E/M code?
There are seven components used in the descriptors of many E/M codes, according to the CPT ® E/M guidelines section “Guidelines for Hospital Observation, Hospital Inpatient, Consultations, Emergency Department, Nursing Facility, Domiciliary, Rest Home, or Custodial Care, and Home E/M Services.” The first three are called key components for E/M level selection.
What is the AMA CPT code set?
The AMA CPT ® code set includes E/M guidelines, but CMS has also published more specific guidance on proper E/M coding and documentation. Most notably, CMS issued the 1995 E/M Documentation Guidelines and the 1997 Documentation Guidelines to help providers and medical coders distinguish the various E/M service levels. Both the 1995 and 1997 E/M Documentation guidelines from CMS are still in use. Many third-party payers also apply these guidelines.
How many categories are there in CPT?
CPT ® includes more than two dozen categories of E/M codes, from office and other outpatient services to advance care planning. You may find further divisions within each category, such as separate options for new patients and established patients.
Why is E/M coding so difficult?
E/M coding can be difficult because of the factors involved in selecting the correct code. For example, many E/M codes require the coder to determine the type of history, examination, and medical decision making, which can involve using special grids and tables to check requirements.
What is E/M billing?
E/M service codes also may be used to bill for outpatient facility services. Facilities and practices may use E/M codes internally, as well, to assist with tracking and analyzing the services they provide. E/M services are high-volume services.
What are some examples of E/M services?
Examples of E/M services include office visits, hospital visits, home services, and preventive medicine services . Codes for services like surgeries and radiologic imaging are found outside of the E/M section of the CPT ® code set.
When will the E/M codes change?
The office and other outpatient E/M codes for established patients changed in line with the revisions to the new patient codes in 2021.
Why was the CPT code set revised in 2021?
Because the role of time changed for office and other outpatient E/M codes in 2021, the AMA revised the Prolonged Services section of the CPT ® code set.
How many pages are needed to use the 2021 MDM table?
To use the 2021 level of MDM table properly, you need to know CPT ® ’s definitions for many terms. In fact, you need to know roughly two pages of definitions. Below is an overview of many of those terms, but you should review the official guidelines to see the complete list of definitions.
What is MDM 2021?
In the 2021 MDM guidelines, CPT ® states that MDM “includes establishing diagnoses, assessing the status of a condition, and/or selecting a management option.”. Three elements define MDM for office/outpatient visits in 2021, and they are similar but not identical to the 2020 elements: 1.
What is CPT code E/M?
Healthcare professionals across a wide range of specialties report evaluation and management (E/M) CPT ® codes on insurance claims to request reimbursement for services performed in the office or other outpatient setting.
What is the AMA code for outpatients?
The American Medical Association (AMA), which holds copyright in CPT ®, and the Centers for Medicare & Medicaid Services (CMS) implemented major revisions related to office and outpatient E/M codes 99201-99215 in 2021. One goal of these changes was to streamline the coding and documentation requirements for these commonly reported codes.
What is the 2020 CPT code set?
AMA’s 2020 CPT ® code set included guidelines on using patient history, clinical examination, and medical decision making (MDM) to determine the correct level of E/M codes. The guidelines also offered information on how to use time to select E/M codes when counseling, coordination of care, or both made up more than 50% of the intraservice time.
What is the code for prolonged Medicare?
Rather, physicians should use Healthcare Common Procedure Coding System (HCPCS) code G2212 for prolonged services for Medicare patients when the total time on the date of service exceeds the maximum required time of the primary procedure code that has been selected using total time on the date of the primary service.
What is E/M in Medicare 2021?
Many health systems that employ members are not implementing the evaluation and management (E/M) increases included in the 2021 Medicare physician fee schedule. Continuing to compensate at pre-2021 levels means meaningful investments in primary care are not being shared with employed physicians.
Is history and physical exam eliminated?
History and physical exam elements eliminated (when not appropriate): The patient history and physical exam elements are no longer components of E/M level code selection. Physicians should still document the history and physical exam as medically appropriate.
Is CPT code 99201 still valid?
These elements may still be necessary for clinical practice, professional liability (i. e., malpractice) reasons, and quality measurement. 99201 is no longer a valid code: CPT code 99201 has been deleted and is no longer available as a CPT code selection.
Why do physicians use E&M codes?
Physicians use E&M CPT codes to bill for services and obtain reimbursement. The AMA is responsible for creating the evaluation and management codes and the guidelines for how those codes are utilized. Physicians and coders must understand the guidelines so that they can accurately select the appropriate E&M codes for the service. Below are some important considerations to better understand the guidelines for selecting the appropriate evaluation and management codes.
What is an E&M code?
Evaluation and management codes, often referred to as E&M codes or E and M codes are a coding system that involve the use of CPT codes from the range 99202 to 99499 which represent services provided by a physician or other qualified healthcare professional. These evaluation and management CPT codes are utilized when the provider is involved in either evaluating or managing patient health. These E&M CPT codes are commonly used by specialty care consultants, emergency room physicians and primary care physicians. For example, office visits, hospital visits, home services and preventive medicine services are considered E&M codes. Codes for procedures like surgeries, radiology and diagnostic tests, and certain treatment therapies are not considered evaluation and management services.
What is CPT 4?
According to CMS, Current Procedural Terminology (CPT-4) is a numeric coding system maintained by the American Medical Association (AMA). The CPT-4 is a uniform coding system consisting of descriptive terms and identifying codes that are used primarily to identify medical services and procedures furnished by physicians and other healthcare professionals. These health care professionals use the CPT-4 to identify services and procedures for which they bill public or private health insurance programs. Evaluation and management codes are a part of the CPT-4 system and reviewed on a periodic basis by the AMA. In addition, CMS considers the CPT-4 as Level-I HCPCS for provider reimbursement under its HCPCS (Healthcare Common Procedure Coding System) reimbursement methodology.
Is physical examination considered an element of outpatient codes?
However, the extent of the physical examination is not an element in selection of the level of office or other outpatient codes.
Should CPT codes be reported separately?
Any additional procedure performed during the same encounter with a specific procedure code should be reported separately. For example, any diagnostic tests performed or interpreted and billed separately should not be included in determining the amount of time utilized when determining the appropriate evaluation and management CPT codes.
When was the CPT E/M revision approved?
To address this, on Feb. 9, 2019, the AMA-convened CPT Editorial Panel approved revisions to the CPT E/M office or other outpatient visit reporting guidelines and code descriptors. These revisions were in direct response to the leadership demonstrated by CMS Administrator, Seema Verma, to take on the challenge of revising the (E/M) office visit reporting guidelines.
What was the workgroup's proposal to the CPT Editorial Panel?
The Workgroup brought their proposal to the CPT Editorial Panel as consensus recommendations and only minor modifications were made by the Panel prior to approving them.
What is the AMA workgroup?
The AMA led a consensus-driven, open and transparent workgroup process to ensure the reimagined approach to office visits represented input from the broad array of medical specialties that perform these visits. The Workgroup was created with members who had both CPT Editorial Panel and AMA/Specialty Society RVS Update Committee (RUC) experience. In addition, the process engaged participants with diverse medical specialty backgrounds including primary care, several surgical specialties (e.g. General Surgery, Cardiology and Vascular Surgery), private payers and qualified healthcare professionals (i.e. Physician Assistants).
What is the CPT code for E/M office visit?
This provision includes revisions to the Evaluation and Management (E/M) office visit CPT® codes (99201-99215) code descriptors and documentation standards that directly address ...
What is the scope of the AMA proposal?
The scope of the AMA proposal is solely focused on revisions to the E/M office or other outpatient visits (CPT codes 99201, 99202, 99203, 99204, 99205, 99211, 99212, 99213, 99214, 99215). The code set revisions will be effective Jan. 1, 2021.
When did the AMA revisions become effective?
Once the revisions became effective on Jan. 1, 2021, the AMA received a lot of feedback on areas causing confusion. In response, the CPT Editorial Panel’s executive committee accepted technical corrections to the E/M guidelines to provide clarifications in a number of key areas. These revisions were posted March 9, ...
How is medical decision making revised?
Medical decision making is revised in the following ways: Clarifying when reporting a test that is considered, but not selected after shared decision making. Providing a definition of “Analyzed” for reporting tests in the data column. Clarifying the definition of a “unique” test. Clarifying what is meant by “discussion” between physicians, ...