| Class I | Minimal mesangial lupus nephritis |
|---|---|
| Class IV-S (C) | Chronic inactive lesions with scars: diffuse segmental sclerosing lupus nephritis |
| Class IV-G (C) | Chronic inactive lesions with scars: diffuse global sclerosing lupus nephritis |
| Class V | Membranous lupus nephritis |
What is the prevalence of Class 1 lupus nephritis?
Prevalence: Seen in 10-25% of people with lupus (SLE). 5% of lupus nephritis cases are class 1. Diagnosed: Immune complex (antigen-antibody complex) deposits are specific molecules that can result from SLE. They build up in trace amounts in the glomerulus in class 1 lupus nephritis. This build-up can be seen under an electron microscope.
What is Class 5 lupus nephritis?
Class 5 may also include class 3 and 4 pathology. Class 6 is advanced sclerosing lupus nephritis in which most of the glomeruli are sclerosed. However, immune complex deposits are not visualized on immunofluorescence since more than 90% of the glomeruli are scarred.
Which subtype of nephritis is the most severe?
Class IV disease ( diffuse proliferative nephritis) is both the most severe, and the most common subtype. More than 50% of glomeruli are involved. Lesions can be segmental or global, and active or chronic, with endocapillary or extracapillary proliferative lesions.
What is Class 3 glomerulonephritis?
Class 3 Known as: Focal glomerulonephritis Prevalence: 25% of lupus nephritis cases are class 3 Diagnosed: Active lesions exists in less than half of the glomeruli.
See more

What are the 5 types of lupus nephritis?
Explanation of Lupus Nephritis ClassesClass 1. Definition: Minimal mesangial glomerulonephritis. ... Class 2. Definition: Mesangial proliferative glomerulonephritis. ... Class 3. Definition: Focal glomerulonephritis. ... Class 4. Definition: Diffuse proliferative nephritis. ... Class 5. Definition: Membranous glomerulonephritis. ... Class 6.
What class is lupus nephritis?
Class I – Minimal mesangial lupus nephritis. Class II – Mesangial proliferative lupus nephritis. Class III – Focal lupus nephritis (active and chronic; proliferative and sclerosing) Class IV – Diffuse lupus nephritis (active and chronic; proliferative and sclerosing; segmental and global)
What is the difference between lupus nephritis and glomerulonephritis?
Lupus nephritis is an inflammation of the kidneys caused by systemic lupus erythematosus (SLE), an autoimmune disease. It is a type of glomerulonephritis in which the glomeruli become inflamed.
How is SLE nephritis diagnosed?
Lupus nephritis is diagnosed through urine and blood tests and a kidney biopsy.
What are the 4 stages of lupus?
When people talk about lupus, they may be referring to the most common form—systemic lupus erythematosus (SLE). However, there are actually four kinds. Click or scroll to read more about each of them: SLE, cutaneous lupus, drug-induced lupus, and neonatal lupus.
What are the 3 types of lupus?
There are three types: Acute cutaneous lupus. Chronic cutaneous lupus erythematosus, or discoid lupus erythematosus (DLE) Subacute cutaneous lupus erythematosus.
What are the 6 stages of lupus?
Stages of lupus nephritisClass I: Minimal mesangial lupus nephritis.Class II: Mesangial proliferative lupus nephritis.Class III: Focal lupus nephritis (active and chronic, proliferative and sclerosing)Class IV: Diffuse lupus nephritis (active and chronic, proliferative and sclerosing, segmental and global)More items...
What is active lupus nephritis?
Lupus nephritis occurs when lupus autoantibodies affect structures in your kidneys that filter out waste. This causes kidney inflammation and may lead to blood in the urine, protein in the urine, high blood pressure, impaired kidney function or even kidney failure.
What does Stage 5 lupus mean?
In class 5 lupus nephritis, a pathologist may detect an excessive amount of immune complexes in the kidneys. Signs and symptoms of class 5 lupus nephritis include high blood pressure, excess protein and/or blood in the urine, extreme swelling, and active lesions on the kidneys.
What is the best medication for lupus nephritis?
Treatments for lupus nephritis include immunosuppressive drugs such as glucocorticoids, cyclophosphamide, mycophenolate, and azathioprine. Belimumab and voclosporin are FDA-approved specifically for lupus nephritis.
What is the difference between lupus and lupus nephritis?
Lupus is basically an autoimmune disease in which your own immune system starts to cause inflammation and damage to pretty much any organ system in your body. The difference between lupus—which can be limited to the skin, joints, or other organs—and lupus nephritis is that the kidney is involved in lupus nephritis.
What is the treatment for nephritis?
Treatment for Nephritis Limiting salt, potassium and protein in the diet. Reducing fluid intake. Taking anti-inflammatory medications. Taking medication to control high blood pressure.
What are the 6 stages of lupus?
Stages of lupus nephritisClass I: Minimal mesangial lupus nephritis.Class II: Mesangial proliferative lupus nephritis.Class III: Focal lupus nephritis (active and chronic, proliferative and sclerosing)Class IV: Diffuse lupus nephritis (active and chronic, proliferative and sclerosing, segmental and global)More items...
What is the pathophysiology of lupus nephritis?
Lupus nephritis occurs when lupus autoantibodies affect structures in your kidneys that filter out waste. This causes kidney inflammation and may lead to blood in the urine, protein in the urine, high blood pressure, impaired kidney function or even kidney failure.
What is activity index in lupus nephritis?
NIH Lupus Nephritis Activity and Chronicity Indices: A way to monitor response to treatment and disease progression. A semi-quantitative grading system of pathologic features on kidney biopsies allows for monitoring response to treatment and showing disease progression.
What is the prognosis for lupus nephritis?
Abstract. Background: Lupus nephritis (LN) affects 30-45% of patients with systemic lupus erythematosus (SLE) and causes great morbidity and mortality. About 10-25% of patients will develop chronic kidney disease (CKD), and it has been described a mortality of 10-20% at 10 years.
What ethnicity is Lupus nephritis?
In a multiethnic international study, it was found that patients who were suffering from lupus nephritis were more frequently men, relatively younger, and of African, Asian, and Hispanic ethnicity. [13]
How old is lupus nephritis?
The mean age of diagnosis for lupus nephritis was observed to be 28.4 years. The risk for the development of lupus nephritis was significantly higher in younger individuals, men, and Hispanics. Interestingly, patients receiving antimalarial drugs had a significantly reduced risk of developing lupus nephritis. [14]
How long does it take for lupus nephritis to develop?
Lupus nephritis typically occurs three years after and usually within 5 years of the onset of SLE . Histological evidence of lupus nephritis is present in most patients with SLE, even in those who do not clinically manifest renal disease. Monitoring for the development of lupus nephritis is done with serial creatinine, urine albumin-to-creatine ratio, and urinalysis. This helps in gauging a rise in serum creatinine value from the baseline as well as for the presence of proteinuria that is commonly observed with lupus nephritis. Since lupus nephritis carries a high risk for increased morbidity, treatment plays an important role in preventing progression to end-stage renal disease (ESRD). [1][2][3][4]
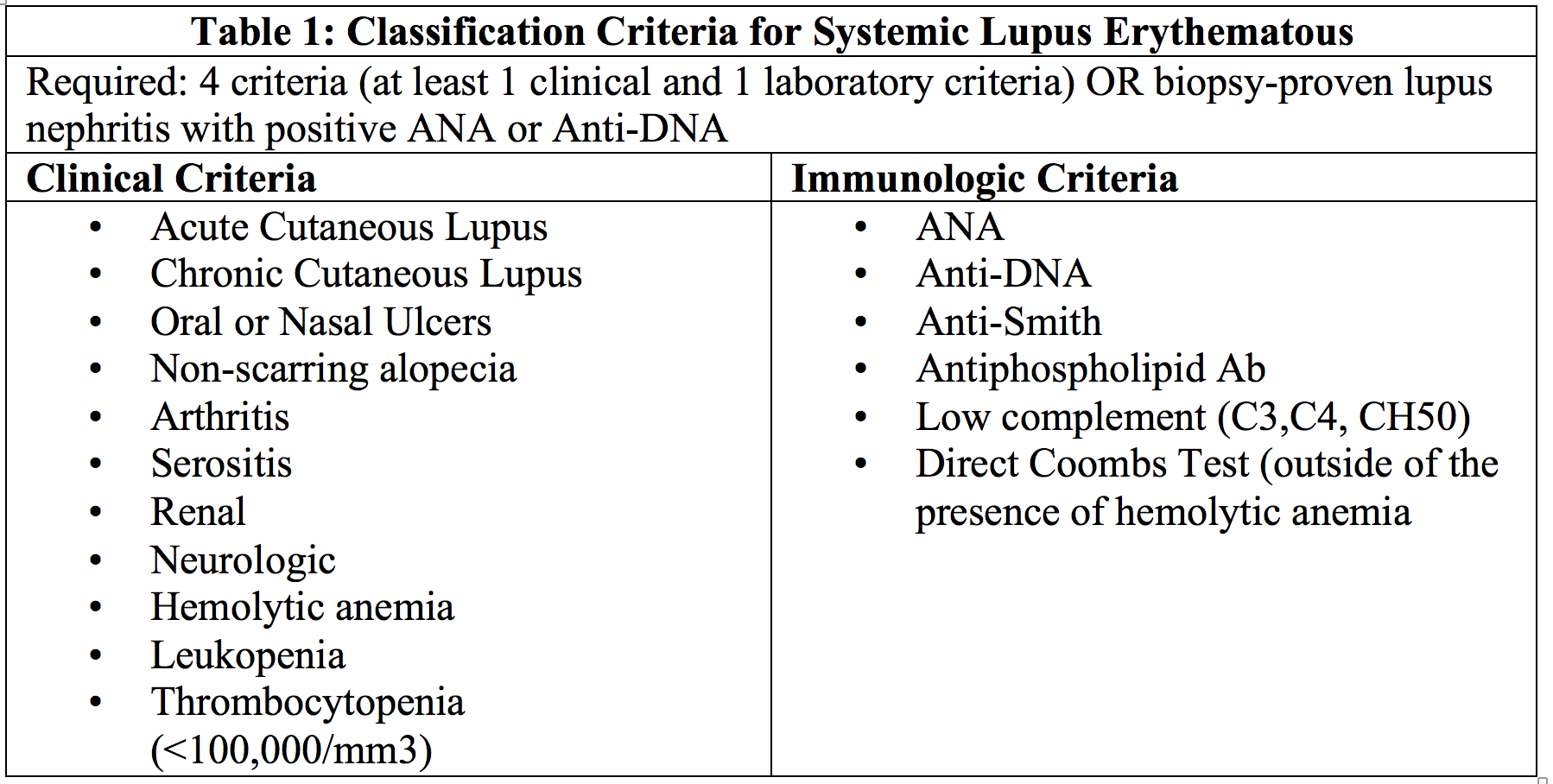
What is a lupus erythematosus?
Systemic lupus erythematosus (SLE) is an autoimmune disease that results in chronic inflammation and damage of more than one organ. It is diagnosed clinically and serologically with the presence of autoantibodies. "Lupus" is a Latin term meaning "wolf," since one of the hallmark facial SLE rashes is similar to the bitemark of a wolf. In 400 BC, the "father of medicine," Hippocrates, was the first to document a case of lupus. From 1700 to 1800s, it was debated whether lupus was associated with tuberculosis or syphilis. Lupus evolved from being viewed as solely a dermatologic manifestation into an all-inclusive multisystemic disease.
What is the primary goal of treatment for lupus nephritis?
The primary goal of treatment in lupus nephritis is the normalization of the kidney function or, at least, the prevention of progressive decline of kidney function. There is variability in the treatment options depending on the underlying pathologic lesion. [5][6]
What is the histologic type of Lupus?
In more severe forms of lupus nephritis, the proliferation of endothelial, mesangial, and epithelial cells and the production of matrix proteins lead to fibrosis.
Is SLE more common in women?
Generally, the prevalence of SLE is higher in women (female-to-male ratio of 9:1). Likewise, lupus nephritis is also more common in women; however, clinically evident renal disease with a worse prognosis is more common in men with SLE.
What is Lupus nephritis?
Lupus nephritis – Advanced definition. Lupus nephritis is a specific type of inflammation in the kidneys known as a glomerulonephritis. In this type of disease, the glomeruli are inflamed. The glomerulus is a network of tiny tubes that transport blood, known as capillaries. It is found at the beginning of the nephron in the kidney.
What is the prevalence of lupus nephritis?
Prevalence: Seen in 10-25% of people with lupus (SLE). 5% of lupus nephritis cases are class 1.
What is the treatment for kidney failure in class 4?
Often, there will be hypertension, elevated serum creatinine, and raises anti-dsDNA titres. Treatment: Treated with corticosteroids and immunosuppressant drugs. Kidney failure is common in class 4.
How many stages of Lupus nephritis are there?
The World Health Organization has subdivided lupus nephritis into 6 stages. The classes represent different severities and require different treatment options. These classes are identified by a clinician examining the kidney biopsy with specialized microscopes and immunofluorescence.
What is a class 1 lupus?
Class 1. Known as: Minimal mesangial glomerulonephritis. Prevalence: Seen in 10-25% of people with lupus (SLE). 5% of lupus nephritis cases are class 1. Diagnosed: Immune complex (antigen-antibody complex) deposits are specific molecules that can result from SLE.
What is a class 6 kidney disease?
Known as: Advanced sclerotic. Diagnosed: Global sclerosis – typically more than 90% of the glomeruli are involved and have active lesions. Class 6 is characterized by progressively worse kidney function.
How to know if you have kidney disease?
Because of this, it is important to be on the lookout for the following symptoms: foamy urine. blood in the urine. dark urine. changes in the frequency of urination. water retention or weight gain throughout the body, including the legs and hands.
What is the classification of Lupus nephritis?
The World Health Organization has divided lupus nephritis into five stages based on the biopsy. This classification was defined in 1982 and revised in 1995. Class I is minimal mesangial glomerulonephritis which is histologically normal on light microscopy but with mesangial deposits on electron microscopy.
What is class III nephritis?
Class III is focal proliferative nephritis and often successfully responds to treatment with high doses of corticosteroids. It constitutes about 25% of cases. Kidney failure is uncommon in this form.
What is class II glomerulonephritis?
Class II disease ( mesangial proliferative glomerulonephritis) is noted by mesangial hypercellularity and matrix expansion. Microscopic haematuria with or without proteinuria may be seen. Hypertension, nephrotic syndrome, and acute kidney injury are very rare at this stage.
What is diffuse proliferative lupus?
Diffuse proliferative lupus nephritis as seen in a pathology specimen. Class IV disease ( diffuse proliferative nephritis) is both the most severe, and the most common subtype. More than 50% of glomeruli are involved. Lesions can be segmental or global, and active or chronic, with endocapillary or extracapillary proliferative lesions.
What is the treatment for lupus nephritis?
Treatment. Corticosteroids may be used. Lupus nephritis is an inflammation of the kidneys caused by systemic lupus erythematosus (SLE), an autoimmune disease. It is a type of glomerulonephritis in which the glomeruli become inflamed.
How many people have Lupus nephritis?
Lupus nephritis affects approximately 3 out of 10,000 people.
What is class V kidney failure?
Class V is membranous nephritis and is characterized by extreme edema and protein loss. It constitutes about 10% of cases. Kidney failure is uncommon in this form.
What is the minimum mesangial hypercellularity required to make a diagnosis of class II lup?
The minimum mesangial hypercellularity required to make a diagnosis of class II lupus nephritis is the presence of ‘four or more nuclei fully surrounded by matrix in mesangial area not including the hilar region.’ This definition is identical to the definition of mesangial hypercellularity that is used in the Oxford classification of IgA nephropathy.
Which cell is infiltrated by inflammatory cells that reside primarily within the capillary lumen and cause?
An illustration of endocapillary hypercellularity. The glomerulus is infiltrated by inflammatory cells which reside primarily within the capillary lumen and cause luminal narrowing.
Is there a change in the classification of Lupus nephritis?
No changes have been made but it is recognized that a more precise distinction from advanced stages of chronic class IV lupus nephritis is needed.
Is karyorrhexis a separate grade?
This is because karyorrhexis is typically the result of neutrophil fragmentation and it is logical to group both lesions together. ‘Fibrinoid necrosis’ is now a separate item to be graded instead of being graded as ‘fibrinoid necrosis/karyorrhexis.’. ‘Cellular/fibrocellular crescents’ replaces ‘cellular crescent.’.
What is the classification of glomerulonephritis?
The classification of glomerulonephritis in systemic lupus erythematosus revisited.The currently used classification reflects our understanding of the pathogenesis of the various forms of lupus nephritis, but clinicopathologic studies have revealed the need for improved categorization and terminology. Based on the 1982 classification published under the auspices of the World Health Organization (WHO) and subsequent clinicopathologic data, we propose that class I and II be used for purely mesangial involvement (I, mesangial immune deposits without mesangial hypercellularity; II, mesangial immune deposits with mesangial hypercellularity); class III for focal glomerulonephritis (involving <50% of total number of glomeruli) with subdivisions for active and sclerotic lesions; class IV for diffuse glomerulonephritis (involving ≥50% of total number of glomeruli) either with segmental (class IV-S) or global (class IV-G) involvement, and also with subdivisions for active and sclerotic lesions; class V for membranous lupus nephritis; and class VI for advanced sclerosing lesions. Combinations of membranous and proliferative glomerulonephritis (i.e., class III and V or class IV and V) should be reported individually in the diagnostic line. The diagnosis should also include entries for any concomitant vascular or tubulointerstitial lesions. One of the main advantages of the current revised classification is that it provides a clear and unequivocal description of the various lesions and classes of lupus nephritis, allowing a better standardization and lending a basis for further clinicopathologic studies. We hope that this revision, which evolved under the auspices of the International Society of Nephrology and the Renal Pathology Society, will contribute to further advancement of the WHO classification.
What are the advantages of the current revised classification of Lupus nephritis?
One of the main advantages of the current revised classification is that it provides a clear and unequivocal description of the various lesions and classes of lupus nephritis, allowing a better standardization and lending a basis for further clinicopathologic studies.
What is the importance of a detailed description of renal biopsy findings?
The Consensus Conference in New York found that accurate reporting of the renal biopsy findings in a detailed and organized manner is an essential requirement to facilitate clear communication with the clinician. A detailed description (quantitative and qualitative) of all the findings by light microscopy, electron microscopy, and immunofluorescence should be followed by a diagnostic segment summarizing and including the class of lupus nephritis (sometimes more than one class), percentage of glomeruli with severe active lesions (fibrinoid necrosis, crescents), and of glomeruli with other active and chronic lesions. The extent, severity, and type of tubulointerstitial (tubular atrophy, interstitial inflammation, and fibrosis) and vascular disease Figure 12 (vascular deposits, thrombi, vasculitis, sclerosis) should also be documented and graded (mild, moderate, severe) in the diagnostic line.
What is class I lupus?
Class I is defined as minimal mesangial lupus nephritis with mesangial accumulation of immune complexes identified by immunofluorescence, or by immunofluorescence and electron microscopy, without concomitant light microscopic alterations. A complete lack of renal abnormalities by light microscopy, immunofluorescence, and electron microscopy no longer qualifies as class I, and in this respect is a change from the 1974 WHO classification.
How many glomeruli are needed for renal biopsy?
In order to reasonably exclude a focal lesion, the biopsy should contain a minimum of 10 glomeruli for light microscopic analysis [22]. Immunofluorescence is required for complete renal biopsy analysis and should include staining for IgG, IgA, and IgM isotypes, kappa and lambda light chains, and complement components C3 and C1q. Glomerular immune deposits attributable to lupus nephritis as detected by immunofluorescence almost always contain dominant polyclonal IgG, as well as C3 and in most instances C1q, with variable codeposits of IgA and IgM. If glomerular immunoglobulin deposits are restricted to IgA or IgM, diagnostic possibilities other than lupus nephritis should be considered in correlation with serologic and clinical findings.
When was Lupus nephritis revised?
With these objectives in mind, a group of renal pathologists, nephrologists, and rheumatologists convened to formulate a revised classification of lupus nephritis during a 3-day consensus conference held at Columbia University, New York, New York in May 2002.
What is class VI glomerulosclerosis?
Class VI (advanced-stage lupus nephritis) designates those biopsies with ≥90% global glomerulosclerosis Figure 11 and in which there is clinical or pathologic evidence that the sclerosis is attributable to lupus nephritis. There should be no evidence of ongoing active glomerular disease. Class VI may represent the advanced stage of chronic class III, class IV, or class V lupus nephritis. Without the aid of sequential renal biopsies, it may be impossible to determine from which the sclerotic glomerular lesions evolved.
