Epinephrine is thought to improve the success of defibrillation with countershock therapy. However, a recent study failed to show any effect of epinephrine in dogs with normal coronary arteries undergoing electrically-induced ventricular fibrillation
Ventricular Fibrillation
A serious heart rhythm problem in which the heart beats quickly and out of rhythm.
What is epinephrine used for in cardiology?
Epinephrine is a vasopressor most often seen in the Adult Cardiac Arrest Algorithm, which is used to treat ventricular fibrillation (VF), pulseless ventricular tachycardia (VT), Asystole, and pulseless electrical activity (PEA). It can also be used to treat bradycardia, anaphylaxis, and severe hypotension.
Is epinephrine effective in dogs with ventricular fibrillation?
However, a recent study failed to show any effect of epinephrine in dogs with normal coronary arteries undergoing electrically-induced ventricular fibrillation (VF). In the current study, the effects of epinephrine were examined in dogs with coronary occlusion undergoing both spontaneous and electrically-induced fibrillation.
What is the effect of epinephrine on the VF threshold?
However, during VF epinephrine also reduces the VF threshold and cellular refractory period, thereby stabilizing fibrillation. In non-VF or asystolic situation, doses less than 10 mcg/min increases HR, contractility and decreases the refractory period. Doses above 10 mcg/min will cause peripheral vasoconstriction and renal vasoconstriction.
Is epinephrine a vasopressor or vasodilator?
Overview: Epinephrine is a vasopressor most often seen in the Adult Cardiac Arrest Algorithm, which is used to treat ventricular fibrillation (VF), pulseless ventricular tachycardia (VT), Asystole, and pulseless electrical activity(PEA). It can also be used to treat bradycardia, anaphylaxis, and severe hypotension.
How does epinephrine treat ventricular fibrillation?
The theoretical benefit of vasopressor medicines, such as epinephrine and vasopressin, is that they increase coronary perfusion pressure. Coronary perfusion pressure is the difference between aortic and right atrial pressure during the relaxation phase of CPR, and it determines myocardial blood flow.
Do you give epinephrine in V fib?
Currently, the ACLS protocol for v fib and pulseless v tach recommends that epinephrine be given after the second defibrillation. Many hospitals and EMS systems, however, have been giving it earlier.
Why is epinephrine used for ventricular tachycardia?
Vasoconstriction effects: epinephrine binds directly to alpha-1 adrenergic receptors of the blood vessels (arteries and veins) causing direct vasoconstriction, thus, improving perfusion pressure to the brain and heart.
Why is epinephrine given after defibrillation?
The receipt of epinephrine within two minutes after the first defibrillation was associated with decreased odds of survival to hospital discharge as well as decreased odds of return of spontaneous circulation and survival to hospital discharge with a good functional outcome.
What is the mechanism of action of epinephrine?
Mechanism of Action Through its action on alpha-1 receptors, epinephrine induces increased vascular smooth muscle contraction, pupillary dilator muscle contraction, and intestinal sphincter muscle contraction.
What is the drug of choice for VFib?
The guidelines recommend administration of amiodarone for sustained ventricular fibrillation (Vf) and ventricular tachycardia (VT) refractory to CPR, defibrillation, and vasopressor in out-of-hospital cardiac arrest. Lidocaine is recommended as an alternative to amiodarone.
When do you give epinephrine in shockable rhythm?
For patients with shockable rhythms (i.e., ventricular fibrillation or pulseless ventricular tachycardia), guidelines recommend epinephrine only after several refractory defibrillation attempts. However, epinephrine frequently is administered inappropriately prior to the first or second defibrillation attempt.
Why is EPI used in ACLS?
Epinephrine is the primary drug used in the cardiac arrest algorithm. It is used for its potent vasoconstrictive effects and also for its ability to increase cardiac output.
Does epinephrine reduce myocardial afterload?
Epinephrine increases peripheral vascular resistance, ventricular afterload, and oxygen demand. artery perfusion, thereby enhancing the potential for termination of ventricular fibrillation by attempted defibrillation. Answer D is incorrect. Epinephrine increases myocardial oxygen consumption.
What to do if a patient is in VFIB?
First call 911 or your local emergency number. Then start CPR by pushing hard and fast on the person's chest — about 100 to 120 compressions a minute. Let the chest rise completely between compressions. Continue CPR until an automated external defibrillator (AED) is available or emergency personnel arrive.
How do you treat V fib ACLS?
If the patient remains in ventricular fibrillation, pharmacological treatment should begin. Epinephrine is the first drug given and may be repeated every 3 to 5 minutes. If epinephrine is not effective, the next medication in the algorithm is amiodarone 300 mg.
Does epinephrine decrease myocardial oxygen consumption?
Although large doses of epinephrine increase coronary perfusion pressure and flow during cardiopulmonary resuscitation, epinephrine also increases myocardial oxygen consumption during ventricular fibrillation.
What is epinephrine used for?
Epinephrine is one of the most commonly used agents in various settings as it functions as medication and hormone. It is currently FDA-approved for various situations, including emergency treatment of type 1 hypersensitivity reactions, including anaphylaxis, induction, and maintenance of mydriasis during intraocular surgeries and hypotension due to septic shock.[1] Off-label uses of epinephrine include, but are not limited to, ventricular fibrillation, pulseless ventricular tachycardia, asystole, pulseless electrical activity (PEA), croup, and severe asthma exacerbations unresponsive to standard treatment. [2][3]In the operating room (OR) setting, epinephrine is also used as a local anesthetic block. Produced by the adrenal medulla, epinephrine plays a vital role in the body’s acute stress response by stimulating the sympathetic nervous system. [4]
What are the effects of epinephrine?
Epinephrine is a hormone that produces widespread effects. Certain effects need monitoring. Tachycardia and hypertension are expected effects when giving epinephrine intravenously, so it is important to titrate the drug carefully while monitoring hemodynamics. Epinephrine is also used with anesthetic agents to provide analgesia. In locations where extravasation of epinephrine has occurred, prevention and treatment of ischemia-induced necrosis are necessary. The infiltrated area should receive treatment with a 10 mL to 15 mL saline solution containing 5 mL to 10 mg of phentolamine, an alpha-adrenergic blocking agent. A study showed how hospitalized patients in the ICU with finger ischemia were associated with the use of vasopressors, including epinephrine. [7]
How much epinephrine is effective for mydriasis?
Epinephrine is effective at a dilution of between 1 to 100,000 and 1 to 400,000 for mydriasis induction and maintenance in pediatric intraocular surgeries.
How long does epinephrine stay in your system?
When administered parenterally, epinephrine has a rapid onset but a short duration of action. When given intravenously, it has a half-life of fewer than 5 minutes. Metabolism is primarily in the liver, along with various other locations such as the kidneys, skeletal muscle, and mesenteric organs. It is degraded into an inactive metabolite named vanillylmandelic acid by MAO and COMT and excreted into the urine. However, a small amount of the drug is excreted unchanged as well.
Which level of management of epinephrine therapy yields the best patient outcomes with the fewest adverse?
Interprofessional management of epinephrine therapy will yield the best patient outcomes with the fewest adverse effects. [Level 5]
Where is epinephrine injected?
For the treatment of anaphylaxis, epinephrine is preferably injected intramuscularly into the anterolateral aspect of the thigh due to rapid absorption. Subcutaneous injection is also an option. For advanced cardiovascular life support (ACLS), patients can receive epinephrine intravenously or intraosseous if needed. Another route of administration is through an endotracheal tube often used in neonatal resuscitation.
Is epinephrine FDA approved?
Epinephrine is one of the most commonly used agents in various settings as it functions as medication and hormone. It is currently FDA-approved for various situations, including emergency treatment of type 1 hypersensitivity reactions, including anaphylaxis, induction, and maintenance of mydriasis during intraocular surgeries and hypotension due to septic shock. It also has several off-label uses. This activity will highlight the mechanism of action, adverse event profile, pharmacology, monitoring, and relevant interactions of epinephrine, pertinent for members of the interprofessional team in treating patients with conditions where this agent is indicated.
What is the concentration of epinephrine?
Definition. Epinephrine in a concentration of 0.02 mg/kg (approximately 1.0 mg in adults) is given for cardiovascular collapse, asystole, ventricular fibrillation, electromechanical dissociation, or anaphylactic shock.
Does epinephrine reduce VF threshold?
According to Miller, this “may be the single most important determinant of survival.”. However, during VF epinephrine also reduces the VF threshold and cellular refractory period, thereby stabilizing fibrillation.
Does epinephrine cause bradycardia?
Doses above 10 mcg/min will cause peripheral vasoconstriction and renal vasoconstriction. Rarely, epinephrine may cause reflex bradycardia due to the marked elevation in BP from the peripheral vasoconstriction.
How long does it take to die from ventricular fibrillation?
Ventricular fibrillation can lead to death within a few minutes or a few days. The survival rate for a person who has a VF attack outside the hospital ranges between 2% and 25%.
Can a cardioverter be used for ventricular fibrillation?
Yes, I did research on ventricular fibrillation, and an implantable cardioverter-defibrillator is the only treatment. I hope that it is not ventricular fibrillation. Although the doctor seems to be stressing that the vasovagal sycnope is caused by postural hypotension because my mom rose from the chair to reach out to turn on the electric fan.
Is ventricular fibrillation serious?
Ventricular fibrillation is very serious. Collapse and sudden cardiac death will follow in minutes unless medical help is provided immediately. If treated in time, V fib and ventricular tachycardia (extremely rapid heartbeat) can be converted into normal rhythm. This requires shocking the heart with a device called a defibrillator.
What does it mean when you have ventricular fibrillation?
You would be dead. Ventricular fibrillation = cardiac arrest. You don't have an irregular heart rhythm with ventricular fibrillation, you don't have a heart rhythm. What is more difficult to know for sure (and maybe that's what you really are asking) is to differ other arrhythmias based on just checking the pulse.
What does RVR mean in a ventricular flutter?
Atrial Fibrillation with “RVR (rapid ventricular response) this means that the ventricular response rate to the a-fib is so fast that the chambers can’t fill with blood between the beats. No filling, no blood pressure. How did they end up terminating this? When this happend to me, the ER Dr's tried IV Cardizem, Lopressor and Digoxin. All did nothing but drop my bp to 60 palp. Ultimately had to be cardioverted.
What is the procedure to destroy small, carefully selected parts of the heart that are causing tachycardia?
The type and severity of an arrhythmia may also require more invasive surgery in order to correct the problem. Ablation is a procedure to destroy very small, carefully selected parts of the heart that are causing tachycardia – an abnormally fast heartbeat. Ablation enables the heart to beat more slowly and normally again.
What are the abnormal heart rhythms caused by magnesium deficiency?
The abnormal heart rhythms that can arise due to magnesium deficiency include premature atrial contractions, premature ventricular contractions, multifocal atrial tachycardia, atrial fibrillation, and even ventricular tachycardia, fibrillation, and Torsade de Pointes (all potentially fatal). Magnesium is important! Magnesium supplementation is therefore necessary for just about everybody to maintain normal tissue levels.
Can ventricular fibrillation be treated?
The only treatment against ventricular fibrillation is an ICD. Or, if there is any cause for it, it can be treated too, but most people that are resucitated from VF will get an ICD implanted.
What is epinephrine used for?
Epinephrine is a vasopressor most often seen in the Adult Cardiac Arrest Algorithm, which is used to treat ventricular fibrillation (VF), pulseless ventricular tachycardia (VT), Asystole, and pulseless electrical activity (PEA). It can also be used to treat bradycardia, anaphylaxis, and severe hypotension.
Can epinephrine cause angina?
Additional Notes on Epinephrine Usage: - The increase in heart rate and blood pressure can cause myocardial ischemia, angina, and increase myocardial oxygen. Therefore, epinephrine should be used with caution when dealing with patients suffering from myocardial infarction.
Does epinephrine help with ROSC?
While administering epinephrine has been proven to be a valuable short-term solution by improving ROSC and hospital admission rates, there have been no major studies that have connected epinephrine usage with long-term survival rates.
Why do people need epinephrine before defibrillation?
Several factors could explain why patients with ventricular fibrillation or pulseless ventricular tachycardia might be receiving epinephrine before defibrillation. Firstly, asystole and pulseless electrical activity comprise >85% of all in-hospital cardiac arrests in the US, for which early epinephrine is the recommended treatment. Recently, epinephrine within five minutes was adopted by GWTG-R as a quality metric for in-hospital cardiac arrest due to a non-shockable rhythm. 10 37 Possibly, the preponderance of non-shockable rhythms among patients with in-hospital cardiac arrest and the increased emphasis on timely epinephrine in such patients might have had a spillover effect from management of in-hospital cardiac arrest with a shockable rhythm. Secondly, nurses are usually the first responders when patients have a cardiac arrest. Although they are usually skilled in initiating cardiopulmonary resuscitation and administering drugs, they might be less inclined to perform defibrillation independently. Epinephrine might be given while waiting for the code team to arrive and perform defibrillation. Understanding the factors that explain the use of epinephrine before defibrillation in patients in hospital who arrest is an important next step, and will be crucial for designing hospital interventions to ensure that patients with shockable in-hospital cardiac arrest are treated with timely defibrillation instead of epinephrine first.
What is the primary outcome of epinephrine and defibrillation?
The primary outcome was survival to discharge . Given that both epinephrine and defibrillation are used for achieving return of spontaneous circulation, we also examined survival after acute resuscitation, defined as return of spontaneous circulation for at least 20 minutes. Finally, to determine whether difference in survival was clinically important, we also examined neurological disability using the cerebral performance category scores 23: a score of 1 denoting mild or no neurological disability; 2, moderate neurological disability; 3, severe neurological disability, 4, coma or vegetative state; and 5, brain death. Favorable neurological survival was defined as survival with a cerebral performance category score of 1 or 2. Discharge scores were missing in 7.5% of patients, and thus analyses after discharge were limited to patients with available discharge cerebral performance category scores.
What is the best treatment for cardiac arrest?
Guidelines recommend prompt defibrillation for treatment of in-hospital cardiac arrest due to an initial rhythm of ventricular fibrillation (or pulseless ventricular tachycardia)
What is the primary exposure to epinephrine?
The primary exposure was administration of epinephrine before first defibrillation. For each patient, we calculated the time intervals (in minutes) from the onset of cardiac arrest to the administration of epinephrine and first defibrillation, respectively, which were used to determine whether patients were treated with epinephrine first or defibrillation first. Patients with identical administration times for epinephrine and defibrillation were included in the defibrillation first group in the primary analysis.
How long does it take for a cardiac arrest to be defibrillated?
27 28 The American Heart Association recommends that patient with in-hospital cardiac arrest with an initial shockable rhythm receive defibrillation within two minutes of cardiac arrest, whereas epinephrine is recommended only if the patient remains refractory to at least two defibrillation attempts (three defibrillation attempts according to UK and European guidelines). 8 9 Accordingly, the GWTG-R registry has adopted time to defibrillation within two minutes in patients with a shockable in-hospital cardiac arrest as a key hospital resuscitation quality metric and has devoted considerable effort and resources towards reducing delays in defibrillation in patients with a shockable rhythm.
Is epinephrine used before defibrillation?
Contrary to resuscitation guidelines and protocols for adult cardiac life support, treatment with epinephrine before defibrillation is common and is associated with lower survival for in-hospital cardiac arrests due to a shockable rhythm.
Is epinephrine first or defibrillation first random?
Our findings should also be interpreted considering the following limitations. Firstly, the assignment of epinephrine first or defibrillation first was not random and there is potential for residual confounding from unmeasured patient variables. Secondly, data on time to epinephrine and time to defibrillation relied on reported times of cardiac arrest, epinephrine, and defibrillation, respectively, within hospital records. Possibly, a lack of synchronization between cardiac monitors and defibrillators, and the generally chaotic resuscitation environment, contributed to errors in measurement, leading to potential misclassification of exposure. Such misclassification is expected to be non-differential, however, and would bias our findings toward the null hypothesis as there is no reason to believe that misclassification of time in the same patient would be differential. Thirdly, our findings cannot establish causation, and it is possible that the use of epinephrine before defibrillation is a marker of lower quality resuscitation care delivery (eg, lower quality chest compressions or quality and experience of the first responders/code team), which is unmeasured. No randomized controlled trials on this treatment strategy are planned or ongoing, however, and such a trial would not be ethically feasible given the strong recommendation for immediate defibrillation in patients with a shockable rhythm. Therefore, despite our study’s limitations, we believe these are the best data on this topic. Finally, hospitals participating in the GWTG-R database represent <5% of all acute care hospitals in the US, and therefore our findings might not be generalizable to non-participating hospitals. The GWTG-R registry represents hospitals that are committed to quality improvement of resuscitation, and use of epinephrine before defibrillation for shockable in-hospital cardiac arrest might be even more pervasive in non-participating hospitals.
What is VF in cardiac arrest?
Ventricular fibrillation (VF or V-fib) is the most common initial heart rhythm in patients with out-of-hospital cardiac arrest (OHCA), and the most salvageable one . 5 In VF, the etiology of arrest is often attributed to either acute ischemia or non-ischemic arrhythmia. 8
What are the causes of VF?
The easiest way to remember the most common causes of VF are to review the reversible “Hs and Ts” in cardiac arrest. The Hs include hypoxia, hypovolemia, hypothermia, hyper/hypokalemia, and hydrogen ions (acidosis). The Ts are tension pneumothorax, cardiac tamponade, toxins, and thrombosis (pulmonary or coronary).
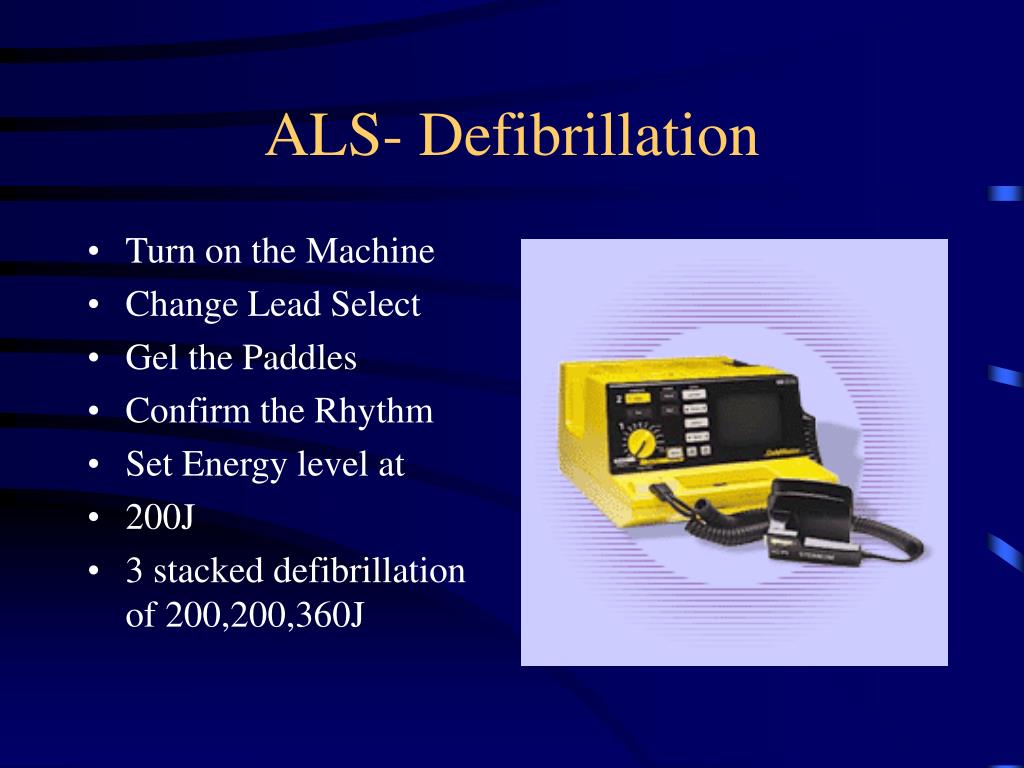
How many joules should a defibrillator deliver?
If a monophasic defibrillator is in use, 360 joules should be delivered to the patient. If the defibrillator is biphasic, the manufacturer recommended joules should be selected (usually 120 to 200 joules). If the amount is unknown, use the maximum available and subsequent doses should be equivalent, and possibly higher. 1
How long does it take to give a defibrillator?
Defibrillation and medication are given in an alternating fashion between cycles of 2 minutes of high-quality CPR. Continue until the patient achieves return of spontaneous circulation (ROSC) or the cardiac arrest team determines it is time to stop the resuscitation efforts.
What is the most important intervention for cardiac arrest?
Irrespective of the cause of cardiac arrest, the most important interventions are early recognition and calling for help—including appropriate management of the deteriorating patient—early defibrillation, high-quality cardiopulmonary resuscitation (CPR) with minimal interruption of chest compressions, and treatment of reversible causes. 6
Is VF a chaotic rhythm?
Although VF appears as a chaotic and disorganized rhythm, characteristics of the ventricular fibrillation waveform such as amplitude, frequency, and organization can be systematically quantified in real-time. 4 These measures have correlated with arrest physiology and are strongly related to clinical outcomes. 7 Current guidelines call for prompt and repetitive defibrillation in the setting of VF during cardiac resuscitation. 2 Early defibrillation is key, but its success largely depends on several other factors, including witnessing of the arrest, early bystander cardiopulmonary resuscitation (CPR) and most importantly, the time from arrest to the first shock. 3
Abstract
Epinephrine is thought to improve the success of defibrillation with countershock therapy. However, a recent study failed to show any effect of epinephrine in dogs with normal coronary arteries undergoing electrically-induced ventricular fibrillation (VF).
Keywords
Original Contributions Effect of Epinephrine on Defibrillation in Ischemic Ventricular Fibrillation CHARLES W. OTTO, MD,"t RONALD W. YAKAITIS, MD,* GORDON A. EWY, MDt Epinephrine is thought to improve the success of defibrillation with countershock therapy.