Explore
Pachymetry is a simple, painless test that quickly measures the thickness of the cornea . Why Measure Corneal Thickness? Corneal thickness as measured by pachymetry is important in the eye care field for several reasons. Pachymetry can tell doctors if the cornea is swollen.
What is pachymetry?
It's also beneficial to know your patient's corneal thickness after she's undergone refractive surgery so you can calculate her true IOP. The reason for performing pachymetry is to establish a more realistic IOP based on a patient's corneal thickness.
What is the purpose of pachymetry after refractive surgery?
Pachymetry is also performed on all patients who are at risk of glaucoma as well as those diagnosed with corneal diseases. It is also performed on patients who undergo corneal transplant or refractive surgery in the cornea. How painful is a pachymetry test?
Who should have a pachymetry test?
However, some are necessary because they give us information that we can't obtain by any other means. The corneal pachymeter is one of these vital instruments. It's cost-effective and should be available to any practitioner who manages glaucoma, co-manages refractive surgery or fits contact lenses.
Why do we need a corneal pachymeter?
What is the purpose of pachymetry?
A pachymeter is a medical device used to measure the thickness of the eye's cornea. It is used to perform corneal pachymetry prior to refractive surgery, for Keratoconus screening, Cataract, LRI surgery and is useful in screening for patients suspected of developing glaucoma among other uses.
What is a pachymetry eye test?
Cornea thickness test also called as Pachymetry test is a simple, painless test to measure the thickness of your cornea — the clear window at the front of the eye. A probe called a pachymeter probe is gently placed on the front of the eye (the cornea) to measure its thickness.
What does the corneal thickness test for?
Measuring corneal thickness is important because it can conceal an accurate reading of the intraocular (eye) pressure. The intraocular pressure (IOP) is important in determining your risk for glaucoma.
How is a pachymetry test done?
Pachymetry painlessly measures the thickness of the cornea with a small probe after the eye is numbed with an eye drop. A thin cornea may contribute to artificially low eye pressure readings, and a thick cornea may contribute to pressure readings that are higher than they actually are.
How accurate is pachymetry?
In addition, a correction factor is needed to adjust for differences in the indices of refraction of the cornea and the model material. Based on these limited results, it appears that the Pentacam gives accurate (to within 7 microns) and repeatable (+/- 3 microns) results for pachymetry.
Who performs a pachymetry?
The optometrist is the one in charge of performing the test and has the knowledge to confirm its correct performance. The one who has to interpret and report the results obtained is the ophthalmologist, who will do it having the clinical context after a complete anamnesis and examination of the patient.
What happens if your cornea is too thin?
Your corneas are too thin If your corneas are too thin, getting LASIK could cause severe vision complications. For someone with thinner corneas, removing any corneal tissue during LASIK could lead to complications.
What causes the cornea to thin?
These factors can increase your chances of developing keratoconus: Having a family history of keratoconus. Rubbing your eyes vigorously. Having certain conditions, such as retinitis pigmentosa, Down syndrome, Ehlers-Danlos syndrome, hay fever and asthma.
What does having thick corneas mean?
At the other end of the spectrum, people with very thick corneas tend to have an intraocular pressure measurement that reads higher than the pressure really is. This means that many of them are considered to have ocular hypertension (high pressure within the eye) but without signs of glaucoma.
What is the most accurate test for glaucoma?
Angle exam Your ophthalmologist uses eye drops to numb your eye, then touches your cornea with a special lens. The lens shows whether the angle is open or closed. If the angle is closed, the drainage system is blocked, which may indicate glaucoma. The test is also called gonioscopy.
Do corneas thin with age?
Thinning of the cornea at a rate of 3–7 μm per decade has been observed in older age in some ethnic groups. A study in 1998 with 1,242 participants aged 10–87 years showed that CCT decreased by 5–6 μm for each decade of life.
What tests are done to diagnose glaucoma?
What happens during a glaucoma test?Tonometry. In a tonometry test, you will sit in an exam chair next to a special microscope called a slit lamp. ... Pachymetry. ... Perimetry, also known as a visual field test, measures your peripheral (side) vision. ... Dilated eye test. ... Gonioscopy.
What does it mean if you have a thick cornea?
A Thicker Cornea – May Mean Less Reason to Worry About Glaucoma. Those patients with thicker CCT may show a higher reading of IOP than actually exists. This means their eye pressure is lower than thought, a lower IOP means that risk for developing glaucoma is lowered.
Can a thick cornea cause high eye pressure?
This might be caused by the effect of corneal thickness on intraocular pressure (IOP) measurements. Goldmann applanation tonometry measurements are correlated with corneal thickness. Thick corneas lead to false high readings whereas thin corneas lead to false low readings.
Why is pachymetry done in glaucoma?
Pachymetry readings can be used in managing glaucoma patients and glaucoma suspects when determining the correlation between the patient's corneal thickness and the patient's intraocular pressure.
What does it mean to have thin corneas?
Thin corneas are when the thickness falls below 500 microns (half a millimeter) since the average normal thickness of a cornea is about 540 microns. 1. They can lead to a variety of vision symptoms that can have short term and long term effects.
How is pachymetry performed?
How Pachymetry Is Performed. Pachymetry can be performed by two methods, by ultrasound techniques or by optical techniques. Ultrasound Pachymetry: 5 Ultrasound pachymetry as the name implies, uses ultrasound principles to measure the thickness of the cornea. This method uses devices that are cost-effective and portable.
What is the name of the device that is used to measure pachymetry?
Some optical pachymeters are designed to be mounted onto a biomicroscope that eye doctors use called the slit lamp. Other devices can measure pachymetry using specular microscopy. This device does not come into direct contact with the cornea.
Why Measure Corneal Thickness?
Corneal thickness as measured by pachymetry is important in the eye care field for several reasons.
What is the name of the optical pachymetry that does not touch the cornea?
One type of optical pachymetry that has gained in popularity is OCT or optical coherence tomography pachymetry. OCT pachymetry also does not touch the cornea to achieve the measurements. OCT uses a principle called optical interferometry.
Why is corneal thickness important?
Knowledge of corneal thickness is important to determine if a person is a candidate for laser vision correction. Because part of the procedure includes removing tissue which will leave the corneal thinner, it is important to know exactly how much will remain.
Is corneal thickness accurate?
Any slight displacement and the reading may not be accurate.
Does insurance pay for ultrasound pachymetry?
The one drawback of optical pachymetry is that insurance companies traditionally pay for ultrasound pachymetry and not always for optical pachymetry so it is possible that your doctor may ask you for payment.
Why do we use pachymeters?
In our practice, weve been using the pachymeter for almost two years to measure central corneal thickness in patients. We have become so dependent on the pachymeter for the evaluation of glaucoma risk that we now have two such devices. It has been eye-opening in how measuring corneal thickness has helped guide us in patient care.
What is a pachymeter used for?
This device historically has been used to measure corneal thickness for assessing corneal health related to pathologies and to evaluate corneal swelling following surgery or injury. Back when radial keratotomy was more common, refractive surgeons used the pachymeter to determine the depth of their incisions.
What is optical pachometer?
The Dictionary of Visual Science and Related Terms defines optical pachometer as A pachymeter used in connection with the slit-lamp biomicroscope for computing corneal thickness. It also defines pachymeter as An instrument for measuring thickness. Here, weve chosen to use pachymeter because that is the more universally accepted spelling ...
Why is corneal thickness important?
Corneal thickness is a key consideration when counseling patients interested in refractive surgery. It is traumatic for the patient and professionally embarrassing for the optometrist to prepare a patient for LASIK only to have the patient turned away because his or her cornea is too thin for LASIK surgery.
How long does it take to test a pachymeter?
A technician can operate the pachymeter. The test takes less than 30 seconds per eye. Most pachymeters are easy to move from one room to another or even between offices. At least one pachymeter operates on a battery, which makes it even more portable for moving around. Pachymeters are light and have a small footprint, so they can easily sit on a counter or a wall shelf.
When to measure corneal thickness?
A convenient time to measure corneal thickness is immediately after you perform applanation tonometry and while the patient is in the examination chair. We prefer to have the patient stay in the exam chair and have the technician bring the pachymeter in to the patient. This makes the battery feature very important to us.
How much does a pachymeter cost?
Several companies manufacture pachy-meters (see list below). These devices range in price from approximately $3,000 to $5,000, depending on the manufacturer and whether or not it comes with a printer.
Where does pachymetry come from?
Pachymetry comes from the Greek word Pachys, which means ‘thick’. Corneal pachymetry is the measurement of corneal thickness. There are several primary reasons why you would need to do this.
What other conditions can a pachymeter help diagnose?
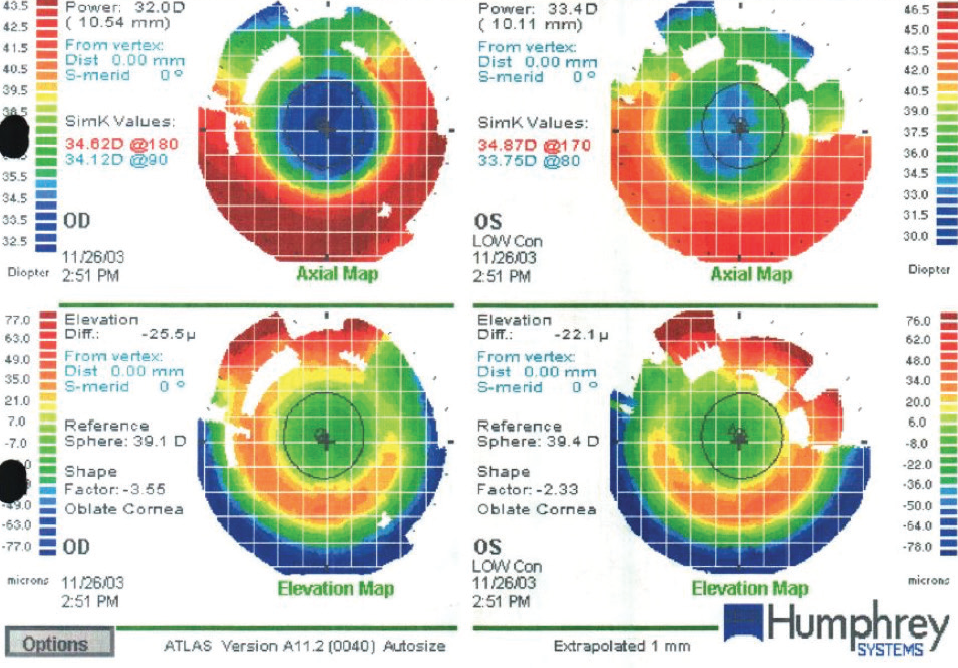
Another condition that can cause sight-threatening damage is Keratoconus. This is a form of Ectasia (chronic thinning of the cornea). It typically develops in childhood and the teens and gradually there is central thinning of the cornea leading to misshaping and reduced vision (the cornea becomes ‘cone shaped’ – hence keratoconus). Screening for this is important and measuring CCT is a key tool.
How do modern pachymeters work?
Modern pachymeters rely either on ultrasound devices which (handheld sometimes) contact the cornea and therefore require anaesthetic and risk cross-infection or corneal abrasion – including potentially Covid, or they are large desktop-based devices using Scheimpflug cameras, OCT or other optical methods. These tend to be expensive and non-portable products.
Can a tonometer be used to measure IOP?
Also, tonometry (the measurement of the IOP) relies on an assumption of the patient’s corneal centre thickness (CCT). If the patient’s CCT is a lot different to the assumed thickness, the tonometer might significantly over or underestimate the IOP. This could lead to false positives and false negatives and may mean some people ‘slip through the net’ of glaucoma screening until they’ve lost some level of vision unnecessarily. Measuring CCT and then correcting the IOP result has been shown to provide a better diagnostic result and improves patient outcomes.
Why is pachymetry important?
In conclusion, pachymetry is a very important aspect of eye health and all individuals are advised to know at least their average corneal thickness as this will enable you to know if you are at risk of glaucoma or not.
What Is A pachymeter?
Pachymeter is a device that is used in the measurement of corneal thickness. It is used before corneal molding evaluation as well as in LASIK surgery.
What is the expected corneal thickness?
The average expected corneal thickness is 540 microns i.e basically half of a millimeter.
How painful is a pachymetry test?
The pachymetry test is not a painful examination and does not constitute any danger to the overall health of the eyes.
What is the purpose of pachymetry for corneal edema?
Corneal experts use accurate results from pachymetry measurements to manage the health conditions of the cornea like corneal ectasias like keratoconus and keratoglobus as well as other causes of corneal edema.
What is the medical term for measuring the thickness of the cornea?
Pachymetry is the medical term for the measurement of the corneal thickness. Hence, pachymetry involves the measurement of the corneal thickness. It is a quick test that does not require ambiguous procedures and does not cause any pain or discomfort. Pachymetry measurement will enable your doctor to understand properly your intraocular pressure ...
What is the best way to measure cornea thickness?
1. Ultrasound pachymetry: It uses ultrasound medical systematic principles to measure the thickness of the cornea. The devices used in ultrasound pachymetry are cost-effective and very portable so performing the test is made easier and simpler.
Why do you do pachymetry?
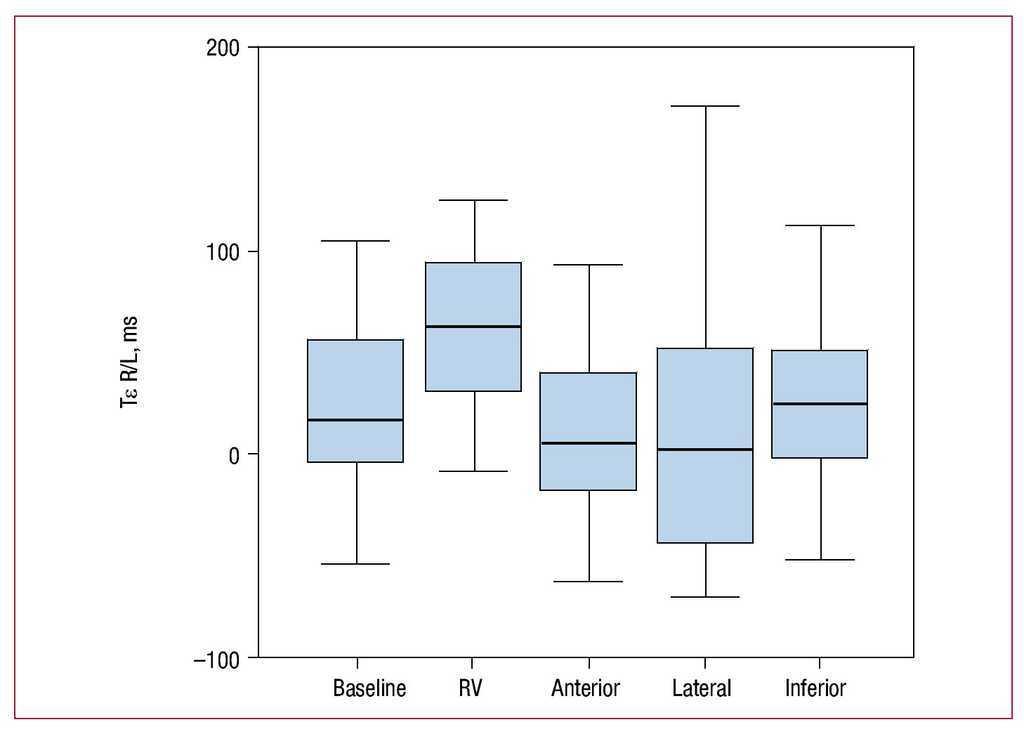
The reason for performing pachymetry is to establish a more realistic IOP based on a patient's corneal thickness. You may have two patients, each with pressures of 25 mmHg and similar disc changes. If one has a corneal thickness of 480 µm and the other is 580 µm, then their target pressures will be completely different because their corrected pressures are probably eight to 10 points apart, instead of being the same at 25 mmHg.
How to explain pachymetry?
I typically explain pachymetry to patients as the difference between pressing on a basketball and pressing on a balloon (on the premise that the exterior of the ball is thicker than the balloon). This helps them understand the concept of thin corneas giving different pressure readings than thick ones. For the cost of a few thousand dollars, you can gain peace of mind, knowing that you've done all that's possible for your patients. Do them a favor before submitting them to a lifetime of expensive treatment. Give them the benefit of the doubt before forever changing their lives with the psychologically devastating diagnosis of an incurable, potentially blinding disease.
Why are corneal pachymeters important?
However, some are necessary because they give us information that we can't obtain by any other means. The corneal pachymeter is one of these vital instruments. It's cost-effective and should be available to any practitioner who manages glaucoma, co-manages refractive surgery or fits contact lenses.
What is the new CPT code for corneal pachymetry?
76514 Ophthalmic ultrasound, echography, diagnostic; corneal pachymetry, unilateral or bilateral (determination of corneal thickness) is the new CPT code. However, some payers are slow to adapt to the new code and still accept or demand the older 0025T code. It does seem to be a source of confusion, real or imaginary, to some of them.
Is pachymetry good for glaucoma?
But the benefits of pachymetry aren't limited to glaucoma and LASIK. It's also useful in monitoring conditions of the cornea such as corneal edema, Fuch's dystrophy, bullous keratopathy, posterior polymorphous dystrophy, contact lens overwear, herpes keratitis and keratoconus.
Is a pachymeter a diagnostic instrument?
As with many other advanced instruments at our disposal, the pachymeter isn't a one-test diagnostic instrument. Instead, it's simply another device that we have in our optometric toolboxes.