Tuberculosis may become a chronic illness and cause extensive scarring in the upper lobes of the lungs. The upper lung lobes are more frequently affected by tuberculosis than the lower ones. The reason for this difference is not clear. It may be due to either better air flow, or poor lymph drainage within the upper lungs.
How does tuberculosis affect the upper lung lobes?
Tuberculosis may become a chronic illness and cause extensive scarring in the upper lobes of the lungs. The upper lung lobes are more frequently affected by tuberculosis than the lower ones. The reason for this difference is not clear. It may be due to either better air flow, or poor lymph drainage within the upper lungs.
What bacteria causes tuberculosis (TB)?
The bacterium Mycobacterium tuberculosis causes tuberculosis (TB), a contagious, airborne infection that destroys body tissue. Pulmonary TB occurs when M. tuberculosis primarily attacks the lungs.
What is tuberculosis?
Infectious disease caused by the bacterium Mycobacterium tuberculosis. Tuberculosis (TB) is an infectious disease usually caused by Mycobacterium tuberculosis (MTB) bacteria. Tuberculosis generally affects the lungs, but can also affect other parts of the body.
Is lower lobe tuberculosis associated with diabetes?
ographic tuberculosis. No cases of diabetes were described in two widely quoted reports of lower lobe disease. 27•28 Lower lobe disease was found in these two latter reports to be more commonly associated with younger
Why is TB in lung Apices?
Moreover, ex vivo experiments conducted with macrophages demonstrated that a high oxygen pressure induced a higher bacillary growth than a low oxygen pressure 39, thus explaining why most cases of lung TB develop at the apex of the lungs, where oxygen concentrations are higher 6.
Which lobe is affected in tuberculosis?
Parenchymal disease in primary TB commonly affects the middle and lower lung zones on CXR, corresponding to the middle lobe, basal segments of lower lobes, and anterior segments of upper lobes.
Is primary TB upper or lower lobe?
primary infection can be anywhere in the lung in children whereas there is a predilection for the upper or lower zone in adults.
What is the most common localization of pulmonary tuberculosis?
The early pathologists recognized that the principal lesions of pulmonary tuberculosis in European adults were cavitations and fibrocaseous nodules in the cephalad third of the lungs, and it was realized that the first cavities usually appeared near the apex, more often on the right.
What part of the lung you can commonly see infiltrates and densities due to tuberculosis infection?
In active pulmonary TB, infiltrates or consolidations and/or cavities are often seen in the upper lungs with or without mediastinal or hilar lymphadenopathy. However, lesions may appear anywhere in the lungs.
Why is the right lung prone to infection?
The right main bronchus is larger in diameter and more vertical making it directly in line with the trachea than the left main bronchus. Thus swallowed objects that accidentally enter the lower respiratory tract are most likely to become lodged in the right main bronchus.
How do primary and secondary TB differ?
Primary and secondary TB are also thought to have characteristic radiographic and clinical features: primary TB is said to be characterized by lower-lobe disease, adenopathy, and pleural effusions, and termed atypical, whereas secondary, or reactivation, TB is associated with upper lobe disease and cavitation, termed ...
What is PTB both upper lungs?
Pulmonary tuberculosis (PTB) is an infectious disease caused by Mycobacterium tuberculosis. This microorganism not only infects the lung but also other organs such as brain, kidneys and lymph nodes. Today, tuberculosis constitutes global public health problem with a greater impact in less industrialized countries.
What are the sites of primary tuberculosis?
The resulting lung infection is called primary TB. The usual site of TB is the lungs (pulmonary TB), but other organs can be involved. In the United States, most people with primary tuberculosis get better and have no further evidence of disease.
Where does TB disseminate to?
Disseminated tuberculosis is a mycobacterial infection in which mycobacteria have spread from the lungs to other parts of the body through the blood or lymph system.
What are the 3 types of tuberculosis?
Tuberculosis is a bacterial infection that usually infects the lungs. It may also affect the kidneys, spine, and brain. Being infected with the TB bacterium is not the same as having active tuberculosis disease. There are 3 stages of TB—exposure, latent, and active disease.
What are some common of extrapulmonary TB sites?
The most common forms of extrapulmonary TB are:Lymph node TB. This is the most common form of extrapulmonary TB. ... Pleural TB. Pleural TB is TB of the thin skin surrounding the lungs. ... TB of the bone and the joint. ... TB of the central nervous system. ... TB of other places.
What is TB in the body?
Depiction of a man with tuberculosis . Tuberculosis ( TB) is an infectious disease usually caused by Mycobacterium tuberculosis (MTB) bacteria. Tuberculosis generally affects the lungs, but can also affect other parts of the body. Most infections show no symptoms, in which case it is known as latent tuberculosis.
What is extrapulmonary TB?
In 15–20% of active cases, the infection spreads outside the lungs, causing other kinds of TB. These are collectively denoted as "extrapulmonary tuberculosis". Extrapulmonary TB occurs more commonly in people with a weakened immune system and young children. In those with HIV, this occurs in more than 50% of cases. Notable extrapulmonary infection sites include the pleura (in tuberculous pleurisy), the central nervous system (in tuberculous meningitis ), the lymphatic system (in scrofula of the neck), the genitourinary system (in urogenital tuberculosis ), and the bones and joints (in Pott disease of the spine), among others. A potentially more serious, widespread form of TB is called "disseminated tuberculosis", it is also known as miliary tuberculosis. Miliary TB currently makes up about 10% of extrapulmonary cases.
How long does it take to treat tuberculosis?
If multiple drug-resistant TB (MDR-TB) is detected, treatment with at least four effective antibiotics for 18 to 24 months is recommended.
What are the symptoms of active TB?
Typical symptoms of active TB are a chronic cough with blood-containing mucus, fever, night sweats, and weight loss.
How many droplets of TB can be released from a sneeze?
A single sneeze can release up to 40,000 droplets. Each one of these droplets may transmit the disease, since the infectious dose of tuberculosis is very small (the inhalation of fewer than 10 bacteria may cause an infection).
When did tuberculosis become epidemic in Europe?
In Europe, rates of tuberculosis began to rise in the early 1600s to a peak level in the 1800s, when it caused nearly 25% of all deaths. In the 18th and 19th century, tuberculosis had become epidemic in Europe, showing a seasonal pattern. By the 1950s mortality in Europe had decreased about 90%.
Is M. bovis a common cause of tuberculosis?
M. bovis was once a common cause of tuberculosis, but the introduction of pasteurized milk has almost completely eliminated this as a public health problem in developed countries. M. canetti is rare and seems to be limited to the Horn of Africa, although a few cases have been seen in African emigrants.
MATERIALS AND METHODS
Records of patients attending the Cleveland (Ohio) Metropolitan General Hospital during the five-year period (July 1983 to June 1988) were evaluated. Patients were included in the study if they had a positive culture for Mycobacterium tuberculosis from specimens of sputum, bronchial washings, or lung biopsy.
RESULTS
Of the 142 patients in the study group, 93 were men and 49 were women. Twenty-nine patients (20.4 percent) were 65 years of age or older, while 62 (43.6 percent) were between 40 and 65 years; 51 patients (36 percent) were younger than 40 years.
DISCUSSION
A number of reports over recent years have drawn attention to the unusual roentgenographic presentations of pulmonary tuberculosis.
ACKNOWLEDGMENTS
The authors thank Emanuel Wolinsky M.D., for his critical review of the manuscript and Kristy Foust for her secretarial assistance.
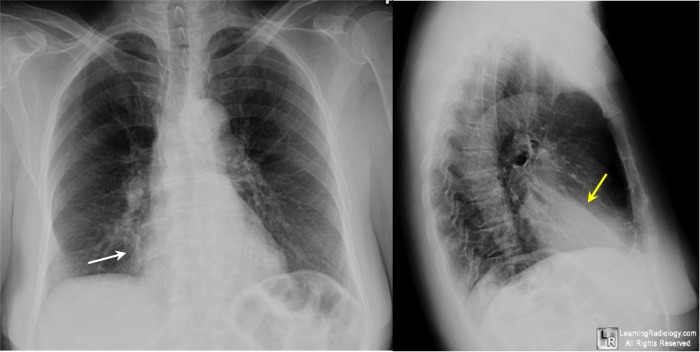
Figures
FIGURE 1 Chest roentgenogram of patient 1 demonstrating a nodular mass in the anterior segment of right upper lobe. Left, posteroanterior view: right, lateral view.
Tables
Abbreviations: RAS = right anterior segment; RPS = right posterior segment; RApS = right apical segment; LAS = left anterior segment; and LAPS = left apico-posterior segment.
When did TB spread?
Pulmonary TB, also known as consumption, spread widely as an epidemic during the 18th and 19th centuries in North America and Europe. After the discovery of antibiotics like streptomycin and especially isoniazid, along with improved living standards, doctors were better able to treat and control the spread of TB.
How to diagnose pulmonary TB?
To diagnose pulmonary TB specifically, a doctor will ask a person to perform a strong cough and produce sputum up to three separate times. The doctor will send the samples to a laboratory. At the lab, a technician will examine the sputum under a microscope to identify TB bacteria.
What is MDR TB?
Multi-drug resistant TB (MDR-TB) is TB that is resistant to the typical antibiotics used to treat the condition, which are isoniazid and rifampin. Some of the factors that contribute to MDR-TB include: healthcare providers prescribing an incorrect drug to treat TB. people stopping treatment early.
How long do you have to take TB drugs?
If you have pulmonary TB, your doctor may prescribe several medicines. You’ll need to take these drugs for six months or longer for the best results.
What percentage of TB deaths are in developing countries?
However, TB remains in the top 10 causes of death worldwide, according to the World Health Organization (WHO) Trusted Source. , with an estimated 95 percent of TB diagnoses as well as TB-related deaths occur in developing countries. That said, it’s important to protect yourself against TB.
Is TB contagious?
The bacterium Mycobacterium tuberculosis causes tuberculosis (TB), a contagious, airborne infection that destroys body tissue. Pulmonary TB occurs when M. tuberculosis primarily attacks the lungs. However, it can spread from there to other organs. Pulmonary TB is curable with an early diagnosis and antibiotic treatment.
Is pulmonary TB the highest risk?
The risk for getting pulmonary TB is highest for people who are in close contact with those who have TB. This includes being around family or friends with TB or working in places such as the following that often house people with TB:
What is the parenchymal zone of TB?
Parenchymal disease in primary TB commonly affects the middle and lower lung zones on CXR, corresponding to the middle lobe, basal segments of lower lobes, and anterior segments of upper lobes. Generally, the primary disease is self-limiting and immune-competent persons remain asymptomatic.
How many cases of TB were there in 2012?
TB is a global health problem and the second leading infectious cause of death, after human immunodeficiency virus (HIV). As per the World Health Organization (WHO) reports, 6.1 million cases of TB were notified by national TB programs in 2012, of which 5.4 million were new cases.[5] .
How big are foci in EPTB?
Initially, the foci are about 1 mm in diameter . Untreated, they may reach 3-5 mm in size and may become confluent, presenting a “snow-storm” appearance. Pleural involvement . Involvement of the pleura is one of the most common forms of EPTB and is more common in the primary disease.
Is CTB a disease?
Chest tuberculosis (CTB) is a widespread problem, especially in our country where it is one of the leading causes of mortality. The article reviews the imaging findings in CTB on various modalities.
Does CXR show TB?
Chest radiograph (CXR) finds its place in sputum-negative patients not responding to a course of antibiotics. Though computed tomography (CT) is frequently employed in the diagnosis and follow-up of TB, it does not find a place in the national and international guidelines.
Is there consensus on ultrasound for TB?
Literature is lacking and no consensus exists on use of ultrasound (USG), CT, and magnetic resonance imaging (MRI) in such patients. With India having a large burden of TB, it is important to have established imaging criteria and recommendations.
Can a tuberculous cavity rupture into pleural space?
Tuberculous cavities can rupture into pleural space, resulting in empyema and even bronchopleural fistula. Erosion into the pulmonary artery branches can lead to massive hemoptysis (Rasmussen pseudoaneurysm). Erosion into systemic vessels or pulmonary veins can lead to hematogenous dissemination and miliary TB.
What is the upper lobe of the lung?
The upper portion, lobe, of your right lung is showing signs that suggest you may have tuberculosis. It is determined by the shading of the x-ray. Anything that restricts the x-rays passing through the tissue shows as a lighter shade.
Does Kylieanne cure tuberculosis?
Kylieanne, it usually doesn't cure.#N#There is scar tissue in your lungs, from tuberculosis. The alveoli, air sacs, that take in oxygen and expel carbon dioxide, are trapped in the scar tissue. They can't function as before.#N#Speak to your doctor. He's seen the x-rays and knows the prognosis better.#N#Hope it helps.

Overview
Signs and symptoms
Tuberculosis may infect any part of the body, but most commonly occurs in the lungs (known as pulmonary tuberculosis). Extrapulmonary TB occurs when tuberculosis develops outside of the lungs, although extrapulmonary TB may coexist with pulmonary TB.
General signs and symptoms include fever, chills, night sweats, loss of appetite, weight loss, and fatigue. Significant nail clubbing may also occur.
Causes
The main cause of TB is Mycobacterium tuberculosis (MTB), a small, aerobic, nonmotile bacillus. The high lipid content of this pathogen accounts for many of its unique clinical characteristics. It divides every 16 to 20 hours, which is an extremely slow rate compared with other bacteria, which usually divide in less than an hour. Mycobacteria have an outer membrane lipid bilayer. If a Gram stain is performed, MTB either stains very weakly "Gram-positive" or does not retain dye as a resu…
Pathogenesis
About 90% of those infected with M. tuberculosis have asymptomatic, latent TB infections (sometimes called LTBI), with only a 10% lifetime chance that the latent infection will progress to overt, active tuberculous disease. In those with HIV, the risk of developing active TB increases to nearly 10% a year. If effective treatment is not given, the death rate for active TB cases is up to 66%.
Diagnosis
Diagnosing active tuberculosis based only on signs and symptoms is difficult, as is diagnosing the disease in those who have a weakened immune system. A diagnosis of TB should, however, be considered in those with signs of lung disease or constitutional symptoms lasting longer than two weeks. A chest X-ray and multiple sputum cultures for acid-fast bacilli are typically part of the initial evaluation. Interferon-γ release assays and tuberculin skin tests are of little use in most of …
Prevention
Tuberculosis prevention and control efforts rely primarily on the vaccination of infants and the detection and appropriate treatment of active cases. The World Health Organization (WHO) has achieved some success with improved treatment regimens, and a small decrease in case numbers.
The only available vaccine as of 2021 is bacillus Calmette-Guérin (BCG). In children it decreases t…
Treatment
Treatment of TB uses antibiotics to kill the bacteria. Effective TB treatment is difficult, due to the unusual structure and chemical composition of the mycobacterial cell wall, which hinders the entry of drugs and makes many antibiotics ineffective.
Active TB is best treated with combinations of several antibiotics to reduce the risk of the bacteria developing antibiotic resistance. The routine use of rifabutin instead of rifampicin in HIV-positive p…
Prognosis
Progression from TB infection to overt TB disease occurs when the bacilli overcome the immune system defenses and begin to multiply. In primary TB disease (some 1–5% of cases), this occurs soon after the initial infection. However, in the majority of cases, a latent infection occurs with no obvious symptoms. These dormant bacilli produce active tuberculosis in 5–10% of these latent cases, often many years after infection.