In the context of DKA the anion gap will be elevated. In addition to lactic acidosis, DKA is one of the the most common causes of an elevated anion gap. The anion gap refers to the difference between the concentration of cations other than sodium and the concentration of anions other than chloride and bicarbonate.
What are the reasons for high anion gap?
This is referred to as a high anion gap. Acidosis with a large anion gap is usually caused by an excess of organic acids or a proportionate reduction in anion excretion. Lactic acidosis, ketoacidosis, toluene intoxication, metabolic alkalosis, respiratory alkalosis, and severe hyperphosphatemia cause a spike in the anion gap.
What does anion gap mean in medical terms?
Your doctor might order the anion gap test if you have symptoms of high blood acid levels, like:
- Shortness of breath
- Nausea or vomiting
- Abnormal heartbeat
- Confusion or fatigue
What is an increased anion gap?
Conditions that can cause acidosis (and therefore a high anion gap value) include:
- diabetic ketoacidosis, a condition requiring immediate medical attention
- overdose of salicylates, such as aspirin
- uremia (urea in the blood)
- ethylene glycol (antifreeze) poisoning
What is the expected anion gap in diabetic ketoacidosis (DKA)?
Simply so, what is anion gap in diabetic ketoacidosis? Anion Gap . In patients with diabetic ketoacidosis , the anion gap is elevated ([Na + K] - [Cl + HCO 3 ] greater than 10 mEq/L in mild cases and greater than 12 mEq/L in moderate and severe cases).

Why does anion gap increased in DKA?
Diabetic ketoacidosis (DKA) is a serious life-threatening complication of diabetes mellitus characterized with high anion gap metabolic acidosis due to excessive production of ketoacids at an expense of reduced serum bicarbonate concentration [1].
How does DKA affect anion gap?
In mild DKA, anion gap is greater than 10 and in moderate or severe DKA the anion gap is greater than 12. These figures differentiate DKA from HHS where blood glucose is greater than 600 mg/dL but pH is greater than 7.3 and serum bicarbonate greater than 15 mEq/L.
Is anion gap elevated in DKA?
DKA is characterized by hyperglycemia, an elevated anion gap* metabolic acidosis, and ketonemia.
What does anion gap mean in DKA?
The anion gap is calculated by subtracting the serum concentrations of chloride and bicarbonate from the sodium concentration. A difference of greater than 12 mEq/L along with a lowered bicarbonate level (<15 mEq/L) shows the presence of an anion gap metabolic acidosis and is a defining feature of DKA.
How does diabetic ketoacidosis cause metabolic acidosis?
It can also occur when the kidneys cannot remove enough acid from the body. There are several types of metabolic acidosis: Diabetic acidosis (also called diabetic ketoacidosis and DKA) develops when substances called ketone bodies (which are acidic) build up during uncontrolled diabetes (usually type 1 diabetes).
How does diabetes affect the anion gap?
A high anion gap indicates acidosis. E.g. In uncontrolled diabetes, there is an increase in ketoacids due to metabolism of ketones. Ketoacids are unmeasured anions, so there is a resulting increase in the anion gap.
What labs are elevated in DKA?
Blood glucose (blood sugar) tests: High blood sugar (above 250 mg/dL) is a sign that you could have DKA.
What is the clinical significance of anion gap?
The serum anion gap is a helpful parameter in the clinical diagnosis of various conditions. The commonest application of the anion gap is to classify cases of metabolic acidosis into those that do and those that do not have unmeasured anions in the plasma (Table 1).
How does diabetes affect the anion gap?
A high anion gap indicates acidosis. E.g. In uncontrolled diabetes, there is an increase in ketoacids due to metabolism of ketones. Ketoacids are unmeasured anions, so there is a resulting increase in the anion gap.
Do you have to have an anion gap for DKA?
DKA is diagnosed by an arterial pH < 7.30 with an anion gap > 12 and serum ketones. Guidelines differ on specific levels of hyperglycemia to be included in the diagnostic criteria for DKA.
Can you be in DKA without anion gap?
DKA patients often develop a non-anion-gap, hyperchloremic metabolic acidosis. This may occur due to gradual development of DKA with urinary excretion of ketoacid (which then cannot be converted to bicarbonate) and/or initial resuscitation with NS.
What labs indicate DKA?
In the hospital, healthcare providers may use the following tests to diagnose DKA:Blood glucose test.Ketone testing (through a urine or blood test).Arterial blood gas.Basic metabolic panel.Blood pressure check.Osmolality blood test.
What is the best treatment for high anion gap?
In mild to moderate acidosis, treatment could be limited to supportive measures including intravenous fluids and respiratory support. Alkalization therapy should be reserved for those individuals with severe acidosis (pH less than 7.1). In the case of diabetic ketoacidosis (DKA), this value is even lower (pH less than 6.9). The most common alkalizing agent is sodium bicarbonate, but sodium and potassium citrate are alternative options. In the event of severe, recalcitrant acidosis, it may be appropriate to treat empirically with alcohol dehydrogenase inhibitors (fomepizole or ethanol) and prepare the patient for emergent hemodialysis. Fomepizole prevents the conversion of alcohols into toxic metabolites through competitive inhibition of alcohol dehydrogenase. Ethanol is not preferred, but it has a similar mechanism of action because alcohol dehydrogenase has a greater affinity for ethanol than for methanol or ethylene glycol. Importantly, fomepizole has the greatest impact on outcomes when given within six hours of presentation; however, given it is frequently in short supply and prohibitively expensive, universal treatment of all high anion gap metabolic acidosis with fomepizole is not advised.
What is high anion gap?
High anion gap metabolic acidosis is one of the most common metabolic derangements seen in critical care patients. Exact numbers are not readily available.
How to calculate anion gap?
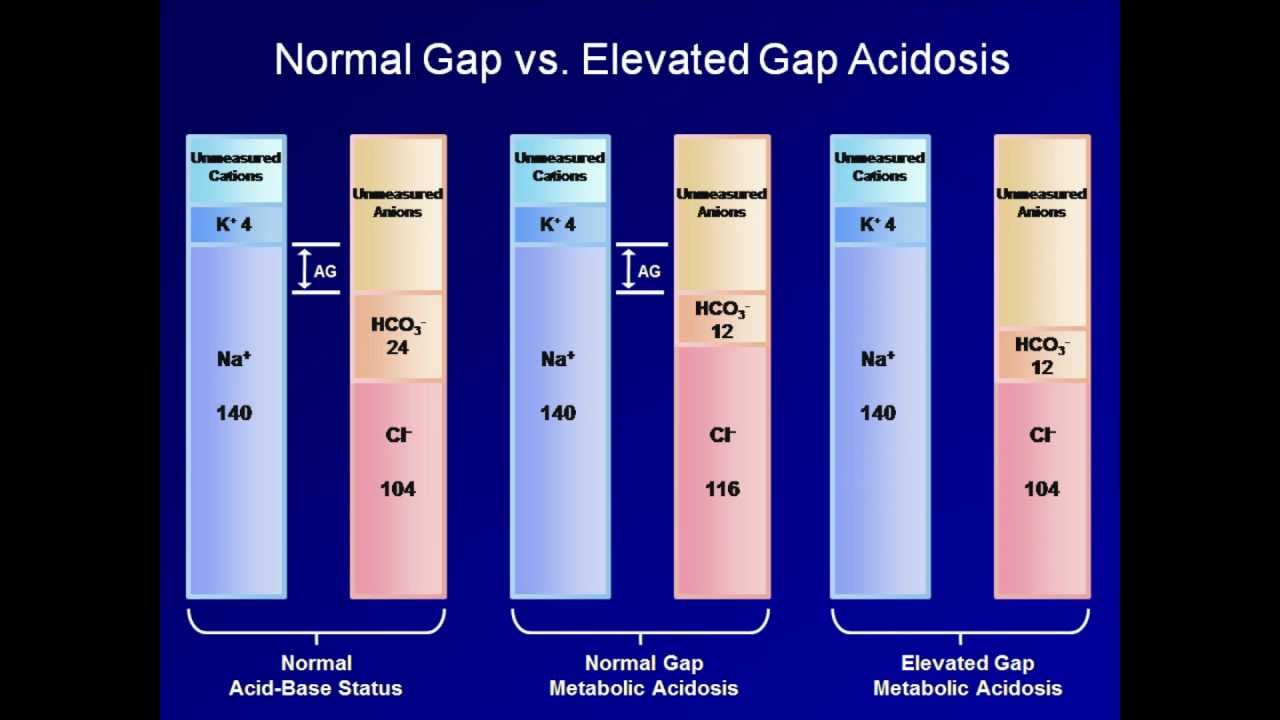
Starting with a basic metabolic panel (BMP) or serum electrolyte panel, the anion gap (AG) should be calculated by subtracting the major anions (chloride & bicarbonate) from the major cation (sodium). Some sources argue for the use of potassium, but it has traditionally been omitted. Consider integrating it in patients with grossly abnormal potassium values. The single largest source of unmeasured anions in the healthy population is albumin, which is why evaluation of, and correction for, hypo/hyperalbuminemia will improve the accuracy of the high anion gap Metabolic Acidosis evaluation. The correction factor of +2.5 mEq per 1 g/dL of albumin below the baseline of four is standard. Therefore, failure to correct for a low albumin would falsely depress the AG, potentially masking the presence of high anion gap Metabolic Acidosis.
What is the toxic metabolite of acetaminophen?
Oxoproline (pyr oglutamic acid, the toxic metabolite of excessive acetaminophen or paracetamol)
What is the treatment for DKA?
Treatment of the underlying disorder may require glucose and insulin in the case of DKA, antibiotics and goal-directed fluid administration in the case of sepsis or administration of specific antitoxins (e.g., fomepizole or n-acetylcysteine) in the case of toxic ingestions.
What is the Creative Commons 4.0 license?
This book is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, duplication, adaptation, distribution, and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, a link is provided to the Creative Commons license, and any changes made are indicated.
What is NCBI bookshelf?
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
What is the term for the concentration of cations and anions in the blood?
Although the term anion gap usually refers to the concentrations of cations and anions in the blood, it can also refer to their concentrations in the urine, which is also clinically useful [ 3 ].
How many patients have low anion gap?
In a study of over 67,000 calculations of the anion gap, the prevalence of a low anion gap value was found in only 304 (0.8%) out of the 39,360 patients whose electrolyte blood levels were studied, and only 19 of them had a repeatedly low anion gap [ 37 ].
Why repeat electrolyte blood test?
It is worthwhile to repeat the electrolyte blood test and recalculate the anion gap value to ensure that the low anion gap value is not an outcome of a laboratory error in measurement .
What is the anion gap?
The anion gap is a value that represents the difference between positively charged ions (cations) and negatively charged ions (anions) in the blood. The anion gap cannot be directly measured, instead, it is calculated from the results of an electrolyte panel, another type of blood test. The anion gap is calculated using the concentrations ...
What is the purpose of anion gap?
The anion gap is primarily used to determine the cause of metabolic acidosis, a condition where the body is producing too much acid or not enough acid is being removed from the body.
What should the total positive charge from cations equal?
In the body, the total positive charge from cations should equal the total negative charge from anions in the blood to maintain overall neutrality.
How to treat metabolic acidosis?
Some possible treatments for metabolic acidosis include detoxification if caused by drugs or toxins and insulin if the condition is caused by diabetes [ 9 ].
What causes DKA in a patient?
However, DKA can be caused by any source of physiologic stress. Occasionally, DKA is the presentation of a serious underlying problem, such as occult sepsis. Common causes of DKA include: Insulin non-adherence, inadequate dosing, or insulin pump failure.
Why is DKA so depleted?
DKA patients are often profoundly volume depleted (e.g., due to vomiting, reduced oral intake, and osmotic diuresis). Hypovolemia triggers the release of stress hormones (e.g., catecholamines, cortisol) which cause insulin resistance and thereby exacerbate the DKA. So prompt reversal of hypovolemia is important.
How many units of insulin can be given in a bolus?
The main advantage of an insulin bolus is that this can usually be given immediately (most units have 10-unit insulin vials immediately available, whereas an insulin infusion needs to be mixed up in pharmacy). Insulin infusion is usually started at 0.1 U/kg/hour (up to a max of 15 units/hour in morbid obesity).
How long does a pneumothorax line last?
Patients may be delirious and unable to stay still enough to facilitate safe placement of a jugular/subclavian line. The line will only be needed for 24-48 hours (until DKA resolves), so infection risk is minimal.
What is the gold standard for defining the presence and extent of ketoacidosis in DKA?
Beta-hydroxybutyrate level is the gold standard for defining the presence and extent of ketoacidosis in DKA.
Why is hypokalemia so bad?
Hypokalemia is extremely problematic, because insulin cannot be given to patients with significant hypokalemia ( since insulin will exacerbate the hypokalemia). Thus, hypokalemia impairs our ability to treat DKA.
How much fluid is needed for DKA?
Most patients will require ~2-4 liters of crystalloid up front. For young DKA patients with normal cardiorenal function, if the patient's heart rate is >100 b/m then they probably need more fluid.
What is the diagnosis of DKA?
DKA is diagnosed by detection of hyperketonemia and anion gap metabolic acidosis in the presence of hyperglycemia. Treatment involves volume expansion, insulin replacement, and prevention of hypokalemia.
What is normal pH of 7.42?
Normal Values pH = 7.38 - 7.42 [H+] = 40 nM/L for a pH of 7.4 PaCO2 = 40 mm Hg [HCO3] = 24 meq/L Acid base definitions Acid base disorder is considered present when there is abnormality in HCO3 or PaCO2 or pH. Acidosis and alkalosis refer to in-vivo derangement's and not to any change in pH. Acidemia (pH < 7.38) and Alkalemia (pH >7.42) refer to derangement's of blood pH. Kidney and Respiratory system play a key roles in maintaining the acid base status. Primary Acid base disorders Metabolic acidosis loss of [HCO3] 0r addition of [H+] Metabolic alkalosis loss of [H+] or addition of [HCO3] Respiratory acidosis increase in pCO2 Respiratory alkalosis decrease in pCO2 Recquired lab values/information Arterial blood gases: pH, PaCO2,PaO2,Sat,CO BUN, Glucose, Creatinine FIO2 and Clinical history Anion and Cations ANIONS CATIONS Chloride Sodium Bicarbonate (Total CO2) Potassium Proteins Calcium Organic acids Magnesium Phosphates Sulfates Electrochemical balance means that the total anions are the same as total Cations. For practical purposes anion gap is calculated using only Sodium, Chlorides and Total CO2. ( (140- (104+24)) = 12. Compensatory measures Buffering---occurs immediately Respiratory regulation of pCO2 is intermediate (12-24 hours) Renal regulation of [H] and [HCO3] occurs more slowly (several days) Extracellular almost entirely through bicarbonate whose concentration highest of all buffers small contribution from phosphate Intracellular Hemoglobin can directly buffer protons H+ entry into RBC matched by exit of Na and K+ Hemoglobin can directly buffer dissolved intracellular conversion of Buffer systems Hemoglobin can directly buffer protons H+ entry into RBC matched by exit of Na and K+ Hemoglobin can directly buffer dissolved intracellular conversion of Bicarbonate Continue reading >>
What is the pH of diabetic ketoacidosis?
Approach Considerations Diabetic ketoacidosis is typically characterized by hyperglycemia over 250 mg/dL, a bicarbonate level less than 18 mEq/L, and a pH less than 7.30, with ketonemia and ketonuria. While definitions vary, mild DKA can be categorized by a pH level of 7.25-7.3 and a serum bicarbonate level between 15-18 mEq/L; moderate DKA can be categorized by a pH between 7.0-7.24 and a serum bicarbonate level of 10 to less than 15 mEq/L; and severe DKA has a pH less than 7.0 and bicarbonate less than 10 mEq/L. [17] In mild DKA, anion gap is greater than 10 and in moderate or severe DKA the anion gap is greater than 12. These figures differentiate DKA from HHS where blood glucose is greater than 600 mg/dL but pH is greater than 7.3 and serum bicarbonate greater than 15 mEq/L. Laboratory studies for diabetic ketoacidosis (DKA) should be scheduled as follows: Repeat laboratory tests are critical, including potassium, glucose, electrolytes, and, if necessary, phosphorus. Initial workup should include aggressive volume, glucose, and electrolyte management. It is important to be aware that high serum glucose levels may lead to dilutional hyponatremia; high triglyceride levels may lead to factitious low glucose levels; and high levels of ketone bodies may lead to factitious elevation of creatinine levels. Continue reading >>
What is the urine anion gap?
Healthy subjects typically have a gap of 0 to slightly normal (< 10 mEq/L). A urine anion gap of more than 20 mEq/L is seen in metabolic acidosis when the kidneys are unable to excrete ammonia (such as in renal tubular acidosis).
What is the formula for SAG?
Formula: SAG = (Na+ + K+) (Cl + HCO3) When Used? To differentiate between the causes of Metabolic Acidosis. Interpretation: If SAG is >12 then the metabolic acidosis is Increased Anion Gap Metabolic Acidosis. Remember the mnemonic MUDPILES for Increased Anion Gap Metabolic Acidosis: Methanol, Uremia, DKA, Propylene Glycol, Iron Poisoning/Isoniazid, Lactic Acidosis, Ethylene Glycol, Salicylates. Formula: OG = Measured Serum Osmolality Calculated Serum Osmolality When Used? To diagnose poisoning by certain alcohols. Interpretation: If >10, consider Ethanol, Methanol, Ethylene Glycol, Isopropyl Alcohol and Propylene Glycol Intoxication. (Remember Isopropyl Alcohol has Increased OG but not Increased SAG! (i.e. doesnt cause AG Metabolic Acidosis)) When Used? To differentiate between causes of Normal AG Metabolic Acidosis i.e. to differentiate between RTA vs Diarrhea as cause of the Normal AG Metabolic Acidosis Interpretation: Remember by (Na+ + K+ Cl) we are actually measuring (Urine Cations Urine Anions), the major Cation in Urine that is not usually measured is NH4+, so if UAG is negative that means Increased NH4+ (i.e. acid) excretion in the Urine which should be the case in any acidosis INCLUDING Diarrhea! But, if renal function is not normal as in RTA, NH4+ is not excreted in Urine and so UAG will be 0 or Positive. So, in Normal Anion Gap Metabolic Acidosis, if: UAG = Negative value > Diarrhea (Remember NeGUTive) Formula: Stool Osmolality (usually not measured and replaced by 290 for ease of calculation) 2 (stool Na+ + stool K+) When Used? To differentiate Secretory vs Osmotic Diarrhea SOG >100 = Osmotic Diarrhea (e.g. Lactose Intolerance) Continue reading >>
What is acid base disorder?
Content currently under development Acid-base disorders are a group of conditions characterized by changes in the concentration of hydrogen ions (H+) or bicarbonate (HCO3-), which lead to changes in the arterial blood pH. These conditions can be categorized as acidoses or alkaloses and have a respiratory or metabolic origin, depending on the cause of the imbalance. Diagnosis is made by arterial blood gas (ABG) interpretation. In the setting of metabolic acidosis, calculation of the anion gap is an important resource to narrow down the possible causes and reach a precise diagnosis. Treatment is based on identifying the underlying cause. Continue reading >>
What is a dka?
Diabetic Ketoacidosis (dka) Diabetic ketoacidosis is an acute metabolic complication of diabetes characterized by hyperglycemia, hyperketonemia, and metabolic acidosis. Hyperglycemia causes an osmotic diuresis with significant fluid and electrolyte loss. DKA occurs mostly in type 1 diabetes mellitus (DM).
What is mild DKA?
Mild DKA is defined by a serum bicarbonate just below 18 or pH slightly less than 7.
How often should you monitor glucose levels?
Monitoring of serum glucose every hour is recommended. If the patient is on a long-acting insulin, this can be utilized. Ensure the patient has adequate insulin for home. After several hours of monitoring with insulin and fluids, recheck labs, including bicarbonate and anion gap.
What is the sensitivity of end tidal CO2?
Interestingly, you can use end tidal CO2 (ETCO2) to assist. An ETCO2 > 35 mm Hg can rule out DKA with 100% sensitivity , while a level < 21 mm Hg is 100% specific for diagnosis. [ 11,12] Along with diagnosis, determining the etiology is vital. The most common triggers include infection and medication/insulin noncompliance, but other stressors include pregnancy, alcohol/other substance use, surgery, trauma, pancreatitis, infarction/ischemia, and many others. [ 1,8,13-17]
How to diagnose DKA?
An easier way to diagnose DKA is to use a venous blood gas (chemistry, anion gap), and serum ketones, preferably beta-hydroxybutyrate. Utilizing urine ketones can be challenging, as this test mainly assesses the presence of acetoacetate, which may not be necessarily present. [ 5,6,10] Beta-hydroxybutyrate is the predominant ketone in DKA, which is converted to acetoacetate. Urine ketone assays measure acetoacetate, and thus patients presenting early in the disease may have negative urine ketone levels. [ 1,5,6]
What to do if you have DKA?
The diagnosis and management of DKA seem simple… Metabolic acidosis, low bicarbonate, high glucose for the diagnosis, and ketones… Replenish intravascular volume, replace potassium, and start insulin. Unfortunately, this is not always the case.
What is HFNC in respiratory?
If the patient has increased work of breathing, or for severe metabolic acidosis, attempt high-flow nasal cannula (HFNC). This supports the work of breathing and improves compensation for metabolic acidosis. Set the FiO2 to over 90%, and increase the flow rate to 60 L/min, which blows off more CO2 by reducing dead space. [ 20,43] While we often rely on noninvasive positive pressure ventilation with a full face mask, this can be dangerous in patients with severe nausea/vomiting, resulting in aspiration. [ 7]
Is DKA associated with diabetes?
Recent literature has questioned our approach to DKA. Many patients will have obvious DKA with known diabetes, large anion gap and ketones, and a history and exam suggesting DKA. While DKA is associated with hyperglycemia, acidosis, and low bicarbonate, patients can have normal glucose (euglycemic DKA) and normal pH and normal bicarbonate (ketoacidosis with metabolic alkalosis from fluid depletion and vomiting). [ 1-6]
What is the result of DKA?
The hyperketonemia in DKA is the result of insulin deficiency and unregulated glucagon secretion from α-cells of the pancreas.
What is the most severe complication of poorly controlled type 1 diabetes?
The most severe and life threatening complication of poorly controlled type 1 diabetes is diabetic ketoacidosis (DKA). DKA is characterized by metabolic acidosis (low pH of the blood), hyperglycemia and hyperketonemia (elevated ketones in the blood). Diagnosis of DKA is accomplished by detection of hyperketonemia and metabolic acidosis ...
What causes an elevated anion gap?
In the context of DKA the anion gap will be elevated. In addition to lactic acidosis, DKA is one of the most common causes of an elevated anion gap. The anion gap refers to the difference between the concentration of cations other than sodium and the concentration of anions other than chloride and bicarbonate.
What is the normal anion gap?
As indicated, the normal anion gap is between 5 mEq/L and 15 mEq/L and a higher number is diagnostic of metabolic acidosis. Rapid and aggressive treatment is necessary as the metabolic acidosis will result in cerebral edema and coma, eventually leading to death.
Why does acetone smell sweet?
Acetone is volatile and is released from the lungs giving the characteristic sweet smell to the breath of someone with hyperketonemia. The ketones are released into the circulation and because they are acidic lower the pH of the blood resulting in metabolic acidosis.
Which fatty acid is most abundant in the ketogenesis pathway?
The ketones (ketone bodies) are β-hydroxybutyrate and acetoacetate with β-hydroxybutyrate being the most abundant.
Where do free fatty acids enter the body?
The free fatty acids enter the circulation and are taken up primarily by the liver where they undergo fatty acid oxidation to acetyl-CoA. Normally, acetyl CoA is completely oxidized to CO 2 and water in the TCA cycle.
What is the BICAR ICU trial?
The BICAR-ICU trial supported the concept of using bicarbonate in uremic metabolic acidosis (with a goal of reducing the requirement for dialysis).
How long does it take for lactate to clear after a seizure?
Don't panic in response to an elevated lactate value following a generalized seizure. This is generally benign and should clear within about an hour – follow closely to ensure that the patient is improving.
What is the most important treatment for anion gap metabolic acidosis?
The most important treatment of anion-gap metabolic acidosis is the reversal of its cause. This will vary depending on the etiology.
What electrolytes are used to make sure that anion gap is elevated?
Repeat electrolytes including Ca/Mg/Phos (to make sure that anion gap is truly elevated).
Is an elevated anion gap a life threatening abnormality?
Elevated anion gap should be regarded as reflecting a life-threatening abnormality until proven otherwise. In an ill patient, seriously consider whether elevated anion gap may reflect hyperlactatemia and consider initiating the evaluation for hyperlactatemia (even before the lactate level returns).
Can hyperlactatemia be caused by shock?
Consider the causes of hyperlactatemia (listed above) within the patient's clinical context. Hyperlactatemia may occur in shock due to any etiology, so if there are features of shock then resuscitation should begin without delay (more on the evaluation of undifferentiated shock here ).
Is epinephrine harmful to the body?
One potential exception here is hyperlactatemia due to epinephrine. This is not necessarily harmful, in fact some evidence suggests that it may be beneficial. ( 20016405 ) Unless the lactate elevation due to epinephrine is substantial (e.g. >10 mM), it may be best to continue epinephrine regardless of an elevated lactate level.