The main cause of this damage is infection with bacteria called Helicobacter pylori Helicobacter pylori, previously known as Campylobacter pylori, is a Gram-negative, microaerophilic bacterium usually found in the stomach. It was identified in 1982 by Australian scientists Barry Marshall and Robin Warren, who found that it was present in a person with chronic gastritis and gastric ulcers, conditions not previously believed to have a microbial cause. It is also linked to the developme…Helicobacter pylori
Can you get an ulcer in your duodenum?
Your duodenum is the first part of your small intestine, the part of your digestive system that food travels through straight after it leaves your stomach. You can get an ulcer in your stomach as well as in your duodenum. Stomach ulcers and duodenal ulcers are both types of peptic ulcers.
Can stress cause a duodenal ulcer?
It's possible that you are more likely to get a duodenal ulcer if you smoke, drink a lot of alcohol or you are stressed, but these things are less important than infection with H. pylori. If you have a duodenal ulcer, you might: have pain in the stomach or abdomen (this might come and go and is relieved by eating or taking an antacid)
What are the symptoms of a duodenal ulcer?
Symptoms of a duodenal ulcer. If you have a duodenal ulcer, you might: have pain in the stomach or abdomen (this might come and go) have indigestion. feel very full and bloated after eating.
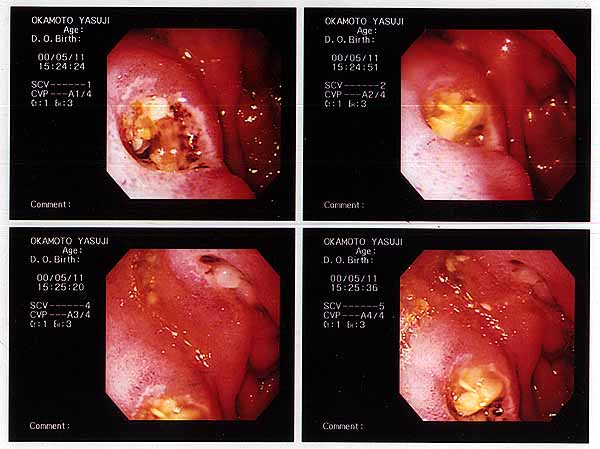
What is a giant duodenal ulcer?
Giant duodenal ulcer (GDU) is defined as a duodenal ulcer that is benign and measures at least 2 cm in diameter. The size of the ulcer makes it difficult to treat because the ulcer, by definition, involves the full circumference of the duodenal wall, leading to scarring and deformity of the duodenal bulb.
Why are duodenal ulcers more common than gastric ulcers?
Both ulcer types show an increase in incidence rate with increasing age. Duodenal ulcers occur in our population at a younger age than gastric ulcers. The incidence of duodenal ulcers starts to rise at approximately 20 years of age, in contrast with 50 years of age for gastric ulcers.
Where are duodenal ulcers most commonly found?
Gastric ulcers that occur on the inside of the stomach. Duodenal ulcers that occur on the inside of the upper portion of your small intestine (duodenum)
Which part of duodenum is highly susceptible to duodenal ulcer?
The ulcer goes right through (perforates) the wall of the first part of the small intestine (duodenum). Food and acid in the duodenum then leak into the abdominal cavity. This usually causes severe pain and is a medical emergency.
Are duodenal ulcers more common than gastric?
Duodenal ulcers are two to three times more common than gastric ulcers. Gastric ulcers are most frequent among those aged 40–70 years, whereas duodenal ulcers are most commonly seen between the age of 25 and 55 years.
What is pathophysiology of duodenal ulcer?
Although the pathophysiology of gastric ulcer and duodenal ulcer is similar, there are clearly differences between the two groups. Duodenal ulcer is typified by H. pylori infection and duodenitis and in many cases impaired duodenal bicarbonate secretion in the face of moderate increases in acid and peptic activity.
Why are duodenal ulcers relieved by food?
3:526:11Pain of Duodenal Ulcer Improves on eating…Ever Wonder Why?YouTubeStart of suggested clipEnd of suggested clipThe acid remains in the stomach. But there is no acid in your duodenum. And that's why the gastricMoreThe acid remains in the stomach. But there is no acid in your duodenum. And that's why the gastric ulcer pain will worsen when you eat because the food and the acid are in the stomach.
Why is lesser curvature more prone to ulcers?
The lesser curvature does not appear to be an area of increased susceptibility to injury. The fact that this is the usual area for the development of chronic gastric ulceration could in part be explained by reflux of duodenal contents along the lesser curvature.
What causes duodenal ulcers to bleed?
When there's too much acid or not enough mucus, the acid erodes the surface of your stomach or small intestine. The result is an open sore that can bleed. Why this happens can't always be determined. The two most common causes are Helicobacter pylori and nonsteroidal anti-inflammatory drugs.
Why do duodenal ulcers hurt after eating?
Duodenal ulcers tend to cause consistent pain. A patient may feel no pain when he or she awakens, but by midmorning it is present. The pain can be relieved by eating, but it usually returns two to three hours later. Pain that wakes a patient at night is common for duodenal ulcers.
Who are more prone to peptic ulcer?
Peptic ulcer can occur at any age. Duodenal ulcers usually appear between ages 30 and 50 and are more common in men than women. Stomach ulcers tend to occur later in life, after age 60, and affect women more often than men.
What is the most reliable symptom of duodenal ulcer?
The most common complaint is a burning pain in the stomach. Duodenal ulcers may also cause abdominal pain a few hours after eating. This pain tends to respond well to medications or foods that reduce stomach acid, but as the effects of these wear off, the pain usually returns.
How can you tell if you have duodenal ulcer?
The most common ulcer symptom is a dull or burning pain in your belly between your breastbone and your belly button (navel). This pain often occurs around meal times and may wake you up at night. It can last from a few minutes to a few hours.
Are anterior or posterior duodenal ulcers more common?
Duodenal ulcers located on the posterior wall are more common than those found on the anterior wall. Posterior ulcers are more likely to erode through intestinal wall into branches of the GDA, resulting in massive bleeding.
Where is the duodenum located?
the small intestineThe duodenum is the first part of the small intestine. It is located between the stomach and the middle part of the small intestine, or jejunum. After foods mix with stomach acid, they move into the duodenum, where they mix with bile from the gallbladder and digestive juices from the pancreas.
Why do stomach ulcers hurt?
Stomach acids and other digestive juices help to make ulcers by burning the linings of these organs. Most ulcers are caused by infection from a bacteria or germ called H. pylori (Helicobacter pylori) or from using pain killers called NSAIDs. The most common symptom is a dull or burning pain in the belly between the breastbone and the belly button. ...
Why do ulcers burn?
Today we know that stomach acids and other digestive juices help create ulcers. These fluids burn the linings of your organs. Causes of peptic ulcers include: H. pylori bacteria (Helicobacter pylori). Most ulcers are caused by an infection from a bacteria or germ called H. pylori.
What is a peptic ulcer?
A peptic ulcer is a sore on the lining of your stomach or the first part of your small intestine (duodenum). If the ulcer is in your stomach, it is called a gastric ulcer. If the ulcer is in your duodenum, it is called a duodenal ulcer.
How are peptic ulcers treated?
Treatment will depend on the type of ulcer you have. Your healthcare provider will create a care plan for you based on what is causing your ulcer.
What is the best medicine for a pylori ulcer?
These include aspirin and ibuprofen. Medicines to treat ulcers may include: Antibiotics. These bacteria-fighting medicines are used to kill the H. pylori bacteria. Often a mix of antibiotics and other medicines is used to cure the ulcer and get rid of the infection. H2-blockers (histamine receptor blockers).
What tests are used to diagnose ulcers?
You may also have some tests. Imaging tests used to diagnose ulcers include: Upper GI (gastrointestinal) series or barium swallow. This test looks at the organs of the top part of your digestive system.
What is the name of the fluid that is swallowed by the stomach?
It checks your food pipe (esophagus), stomach, and the first part of the small intestine (the duodenum). You will swallow a metallic fluid called barium. Barium coats the organs so that they can be seen on an X-ray. Upper endoscopy or EGD (esophagogastroduodenoscopy).
Where are duodenal ulcers found?
Duodenal ulcer prevalence in Africa, south of the Sahara: Information from research conducted between 1970 and 1984 showed that duodenal ulcer prevalence is high in regions of high rainfall where the staple crops are yams, cassava, sweet potato, green bananas or where the staple diet is refined maize, wheat, or rice.
What is the difference between proximal and duodenal ulcers?
Acid secretion patterns differ with the location of the ulcer. Duodenal ulcers are associated with high-acid secretion while proximal gastric ulcers are associated with a low-acid output. Distal gastric ulcers can have a normal- or high-acid output. The difference in acid output is a reflection of the effects of inflammation on the underlying cell types. Inflammation of the antrum and the body is much more pronounced in gastric ulcer than in duodenal ulcer. In addition, there is usually a progression of inflammation in gastric ulcers. As a result, this could eventually lead to hyposecretion of acid from glands in the fundus.
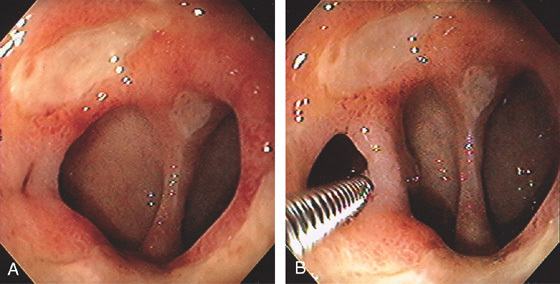
What is a postbulbar duodenal ulcer?
Postbulbar duodenal ulcer. Characteristic appearance with an ulcer crater (asterisk) in the middle of a stricture produced by spasm and oedema. †
How common are duodenal ulcers?
Duodenal ulcers are two to three times more common than gastric ulcers. Gastric ulcers are most frequent among those aged 40–70 years, whereas duodenal ulcers are most commonly seen between the age of 25 and 55 years. Thus, complications in gastric ulcers tend to be more severe because they tend to affect older individuals. Ulcer rates are declining rapidly for younger men and increasing for older individuals.
What is the treatment for gastric ulcers?
As with gastric ulceration, treatment options may include medical, endoscopic, and surgical approaches. Surgical options are based on the same operative indications (bleeding, perforation, obstruction, and intractability). In the case of perforation, a duodenal ulcer is oversewn and a well-vascularized Graham patch is used to cover the defect. Highly selective vagotomy is preferred, but truncal vagotomy and drainage procedures are within the standard of care. Duration of symptoms, previous treatments, medication usage (NSAIDs), and comorbidity assist in operative planning. Postgastrectomy syndromes are, again, a well-documented complication.
Where is duodenal ulcer disease most prevalent?
The distribution of duodenal ulcer disease in sub-Saharan Africa is not uniform, the distribution differing not only by country, but also within countries. Based on the data shown in Table 9.3, the highest rates of DU are found in Malawi, Cameroon, Kenya (Nairobi), and Nigeria, with a moderately high level being reported in Ghana. These findings are consistent with previous observations by Tovey et al. who reported Northern Tanzania, Ethiopia, the Nile/Congo watershed, the Cameroons, Nigeria, and Ghana to have the highest prevalence of DU [35].
Is Helicobacter pylori a secondary infection?
Evidence is presented suggesting that H. pylori infection is a secondary infection that prevents healing and leads to chronicity. Eradication of the infection allows the ulcer to heal. Increasing urbanization with the adoption of refined maize and wheat products, of rice or the Western type of food will have Implications for the present time and lead to an increasing incidence of duodenal ulceration in the black population. The protective phospholipids and phytosterols present in the staple foods of low duodenal ulcer prevalence areas may be of help in the management of recurrent duodenal ulceration despite H. pylori eradication and also in the prevention of peptic ulceration due to NSAIDs. While eradication of H. pylori infection is important in the treatment of duodenal ulceration, there is no justification for a policy of mass community eradication.
What causes a duodenal ulcer?
The two primary causes for duodenal ulcers are a history of recurrent or heavy NSAID use and a diagnosis of H. pylori.[1] The majority of patients carry a secondary diagnosis of H. pylori; however, as infection rates have declined, other previously uncommon etiologies are becoming more prevalent. Other causes of duodenal ulcers include etiologies that, in similar ways to NSAIDs and H. pylori, disrupt the lining of the duodenum. Some of these include Zollinger-Ellison syndrome, malignancy, vascular insufficiency, and history of chemotherapy.
How common are duodenal ulcers?
According to multiple studies that have evaluated the prevalence of duodenal ulcers, they are estimated to occur in about 5 to 15% of the Western population .[2] Previously, the recurrence and prevalence rates were extremely high due to a lack of identification and effective treatment of H. pylori. Most recently, a systematic review of seven studies discovered the rates to be significantly lower. However, the variability was thought to be due to the prevalence of H. pyloriin the population studied and the guidelines for diagnosis utilized, including endoscopic guidelines. In areas with a higher incidence of H. pylori, however, the rates were noted to be the highest, which supports the previously established notion that H. pyloriinfection presents significant comorbidity for the development of duodenal ulcers.[3] The overall decline in rates of diagnosis of duodenal ulcers is also attributable to developing physician and patient awareness regarding the use of NSAIDs and potential complications that can be associated with misuse as well as the slowly declining rates of smoking amongst younger individuals as research has also been found this to be another confounding comorbidity.
What is the treatment for H pylori?
The majority of patients, however, do not require long-term antisecretory therapy following H. pyloritreatment, upon confirmation of eradication and if they remain asymptomatic. Patients diagnosed with H. pylorimust receive triple therapy (two antibiotics and a proton pump inhibitors), and elimination must be confirmed.[9] A meta-analysis of 24 randomized trials helped show that eradication of H. pyloriwas associated with significantly lower rates of both gastric and duodenal ulcers. Patients with complications at the time of presentation will need to follow postoperative recommendations made by their general surgeon. They will likely require treatment for more extended periods (8 to 12 weeks) or until confirmed ulcer resolution by repeat endoscopy. From a surgical standpoint, patients may require laparoscopic repair for perforated ulcers or bleeding ulcers that are not responsive to endoscopic intervention.
What should be included in education for ulcer patients?
Education for patients treated for ulcers should include the primary causes associated with ulcers, practices to avoid such as NSAID use, and the risk of interventions offered . Individuals should also be advised regarding long-term use of proton pump inhibitors (PPIs) if this is the therapy of choice for symptomatic management.
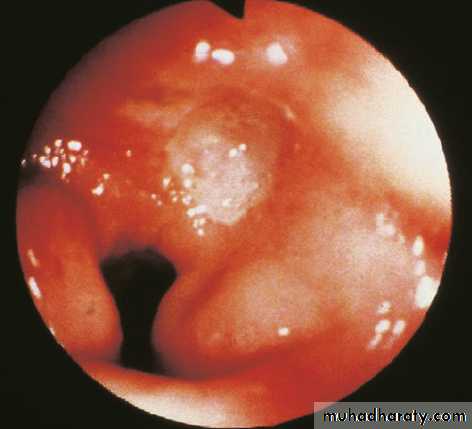
Can H pylori be detected in hematoxylin?
In cases of H. pyloridriven duodenal ulcers, biopsy with histopathological studies can assist in the diagnosis. H. pylori, a spiral-shaped bacterium, can be seen in hematoxylin and eosin (H&E) staining. Reports show the sensitivity and specificity of H&E stain to be 69% to 93% and 87% to 90%, respectively.[6] However, specificity can improve 90% to 100% by using special stains such as modified Giemsa stain, Warthin-Starry silver stain, Genta stain, and immunohistochemical (IHC) stain. As Giemsa stain is straightforward to use, inexpensive and provides consistent results, it is preferred in many laboratories. [6]
Is duodenal ulcer a peptic ulcer?
Duodenal ulcers are part of a broader disease state categorized as peptic ulcer disease. Peptic ulcer disease refers to the clinical presentation and disease state that occurs when there is a disruption in the mucosal surface at the level of the stomach or first part of the small intestine, the duodenum. Anatomically, both the gastric and duodenal surfaces contain a defense system that includes pre-epithelial, epithelial, and subepithelial elements. Ulceration occurs from damage to the mucosal surface that extends beyond the superficial layer. While most duodenal ulcers present with dyspepsia as the primary associated symptom, the presentation can range in severity levels, including gastrointestinal bleeding, gastric outlet obstruction, perforation, or fistula development. Therefore, the management is highly dependent on the patient's presentation at the time of diagnosis or progression of the disease. The diagnosis of duodenal vs. gastric ulcer merits consideration in patients with dyspepsia/upper abdominal pain symptoms who also report a history of NSAID use or previous Helicobacter pylori diagnosis. Any patient diagnosed with peptic ulcer disease and, most specifically, the duodenal ulcer should undergo testing for H. pylori as this is a common cause.
What is the duodenal ulcer?
Duodenal ulcer occurs in subjects who are infected by H. pylori and who also have gastric metaplasia in the duodenal bulb, which will be colonized with H. pylori. Hyperproduction of acid following a decrease in somatostatin and an increase in gastrin production are observed. Antral gastritis is the usual pattern of histological lesions. Smoking and infection with cag -positive H. pylori strains are important risk factors. The incidence of duodenal ulcers is decreasing following the decrease in H. pylori prevalence.
Where are duodenal ulcers found?
Duodenal ulcer prevalence in Africa, south of the Sahara: Information from research conducted between 1970 and 1984 showed that duodenal ulcer prevalence is high in regions of high rainfall where the staple crops are yams, cassava, sweet potato, green bananas or where the staple diet is refined maize, wheat, or rice. Duodenal ulcer prevalence is low in regions of lower rainfall where the staple crops are maize, millets, soya, or wheat and where the maize is home-pounded or the wheat is not refined.
What is the difference between peptic ulcer and gastric ulcer?
Peptic ulcer disease is a chronic, relapsing disease that causes significant morbidity and mortality due to pain, bleeding and perforation of the gastric mucosa. Nearly 70% of all gastric ulcers and 95% of duodenal ulcers are attributable to H. pylori infection. However, eradication of H. pylori allows most peptic ulcers to heal and prevents further relapse.
What is the relationship between H. pylori and the gastric epithelium?
Mechanistically, gastric ulcers originate from prolonged, intimate contact between H. pylori and the gastric epithelium. This interaction leads to continuous inflammation in the gastric antrum, thereby perpetuating mucosal breakdown, erosive gastritis, and eventually gastric ulceration.
Where is duodenal ulcer disease most prevalent?
The distribution of duodenal ulcer disease in sub-Saharan Africa is not uniform, the distribution differing not only by country, but also within countries. Based on the data shown in Table 9.3, the highest rates of DU are found in Malawi, Cameroon, Kenya (Nairobi), and Nigeria, with a moderately high level being reported in Ghana. These findings are consistent with previous observations by Tovey et al. who reported Northern Tanzania, Ethiopia, the Nile/Congo watershed, the Cameroons, Nigeria, and Ghana to have the highest prevalence of DU [35].
Where are gastric ulcers located?
Gastric ulcers are subdivided into proximal ulcers, located in the body of the stomach, and distal ulcers, located in the antrum and angulus of the stomach. Gastric ulcers are located mainly along the lesser curvature, in particular at the transitional zone of corpus- to antral-type mucosa.
Where do ulcers occur?
Duodenum. Duodenal ulcers usually occur at the duodenal cap , where the acidic chyme meets the duodenal mucosa, before it mixes with the alkaline secretions of the duodenum. The duodenum does not have the same protective mechanisms as the stomach mucosa.
What causes gastric and duodenal ulcers?
pylori). the bacterium produces substances that weaken the stomach's protective mucus and make it more susceptible to the damaging effects of acid and pepsin.
What is a stomach ulcer?
What is a stomach or duodenal ulcer? An ulcer is an open sore, or lesion, usually found on the skin or mucous membrane areas of the body. An ulcer in the lining of the stomach or duodenum, where hydrochloric acid and pepsin are present, is referred to as a peptic ulcer.
What are some complications from ulcers?
bleeding- As the lining of the stomach or duodenal wall is eroded, blood vessels may also be damaged, causing bleeding.
Which acid contributes to ulcer formation?
acid and pepsin- hydrochloric acid and pepsin, contributes to ulcer formation.
What causes a stomach to narrow?
narrowing and obstruction- Ulcers located at the end of the stomach can cause swelling and scarring, which can narrow or close the intestinal opening. This obstruction can prevent food from leaving the stomach and entering the small intestine, resulting in vomiting the contents of the stomach.
What is upper GI?
upper GI (gastrointestinal) series- Examination of the esophagus, stomach, and duodenum with an endoscope. endoscopy- A test that uses a small, flexible tube with a light and a camera lens at the end (endoscope) to examine the inside of part of the digestive tract. blood, stool, breath, and stomach tissue test- Performed to detect the presence ...
Does smoking cause ulcers to recur?
smoking- studies show smoking increases the chances of getting an ulcer, slows the healing process of existing ulcers, and contributes to ulcer recurrence. caffeine- stimulates the acid secretion in the stomach, which can aggravate the pain of an existing ulcer.
What causes a duodenal ulcer and who is more at risk?
Our stomach is lined with a mucus-producing inner layer known as the mucosa. This layer is delicate, and its integrity depends on a careful balance of protective factors (such as the production of mucus) and destructive factors (such as acid production).
How to treat duodenal ulcers?
Treatment for duodenal ulcers usually involves a combination of medications that reduce acid secretion, protect the mucosa, and kill H. pylori bacteria (if present).
What are the symptoms of a duodenal ulcer?
Symptoms vary from person to person, and some people may have no symptoms at all. Abdominal pain is common, and that associated with duodenal ulcers is more likely to worsen on an empty stomach.
How is a duodenal ulcer diagnosed?
To help diagnose a duodenal ulcer, your doctor will ask you what medications you take or have been taking, and if you have had peptic ulcers or any other relevant condition in the past. Make sure you mention all the medications you are taking, especially NSAIDs such as aspirin , ibuprofen, diclofenac, or ketorolac.
What is the other type of peptic ulcer?
The other type of peptic ulcer is a stomach (gastric) ulcer and this occurs in your stomach.
Where do ulcers occur?
Most ulcers occur in the first layer of the inner mucosal lining. A hole that goes all the way through is called a perforation and this will cause severe pain and bleeding. A perforation is a medical emergency.
Can NSAIDs cause duodenal ulcers?
If NSAIDs have caused your duodenal ulcer, your doctor may advise you to stop taking them, reduce their dosage, or switch to an alternative medicine. Follow his/her advice. Talk to your doctor before taking antacids as these may reduce the absorption of some other medications.
What is a gastric ulcer?
What are gastric and duodenal ulcers? Gastric and duodenal ulcers are two kinds of peptic ulcers. A peptic ulcer is a sore that’s on the inside of the stomach lining — a gastric ulcer — or the upper part of the small intestine — a duodenal ulcer. A person can have one or both types of ulcers at the same time.
What are the symptoms of ulcers?
This means that a person may have pain in a location away from the actual ulcer. Other symptoms can include: nausea. vomiting. bloating.
What is the treatment for gastric ulcers?
For example, your doctor may prescribe histamine receptor blockers (H2 blockers) or proton pump inhibitors (PPIs) to reduce the amount of acid and protect your stomach lining . For H. pylori infections, your doctor will prescribe antibiotics, PPIs, ...
How do you know if you have a gastric ulcer?
One way of telling if you may have a gastric or duodenal ulcer is to figure out where and when your symptoms occur. For some, the time between meals aggravates an ulcer. For others, eating may be a trigger for the pain.
What to do if a stomach ulcer is too deep?
In cases that medication or endoscopic therapy doesn’t work, your doctor may recommend surgery. If the ulcer becomes deep enough to cause a hole through the wall of your stomach or duodenum, this is a medical emergency and surgery is most often required to fix the problem.
What causes food to leak through the stomach?
ulcer breaks through the lining and stomach wall, causing bacteria, acid, and food to leak through. peritonitis. inflammation and infection of the abdominal cavity due to perforation. blockage. scar tissue can form as a result of the ulcers and keep food from leaving the stomach or duodenum.
How does H pylori affect the stomach?
This bacterium affects the mucus that protects your stomach and small intestine, allowing for stomach acid to damage the lining. An estimated 30 to 40 percent of U.S. people are infected with H. pylori.