Nearly half of all VTEs occur during or after hospitalization, with pulmonary embolism accounting for 10% of inpatient mortality. Appropriate prophylaxis in high-risk medically ill patients has been shown to reduce risk of VTE and related mortality. Despite current evidence-based guidelines, VTE prophylaxis has been under-used.
Is 'bridging' necessary in patients with VTE?
This systematic review found that periprocedural bridging in patients with previous venous thromboembolism increases the risk of bleeding without reducing the risk of periprocedural venous thromboembolism. Most patients with venous thromboembolism do not benefit from periprocedural bridging.
What does VTE stand for in medical category?
What is Venous Thromboembolism (VTE)? Venous thromboembolism (VTE) refers to a blood clot that starts in a vein. It is the third leading vascular diagnosis after heart attack and stroke, affecting between 300,000 to 600,000 Americans each year. There are two types:
What is VTE in medical term?
- Unexplained shortness of breath
- Rapid breathing
- Chest pain anywhere under the rib cage (may be worse with deep breathing)
- Fast heart rate
- Light headedness or passing out
What are the causes of venous thromboembolism (VTE)?
What is Venous Thromboembolism?
- Complications of DVT. The most serious complication of DVT happens when a part of the clot breaks off and travels through the bloodstream to the lungs, causing a blockage called ...
- Risk Factors for DVT. Almost anyone can have a DVT. ...
- Preventing DVT. ...
- Symptoms. ...
- Diagnosis of DVT and PE. ...
- Treatments for DVT and PE. ...
Why do we need VTE prophylaxis?
Venous thromboembolism (VTE) prophylaxis consists of pharmacologic and nonpharmacologic measures to diminish the risk of deep vein thrombosis (DVT) and pulmonary embolism (PE).
When do we use VTE prophylaxis?
Hospitalized patients are at increased risk of VTE when compared to patients in the community. Therefore, it is imperative to consider DVT prophylaxis in every hospitalized patient. Full history and physical examination are warranted to assess the risk of VTE and bleeding.
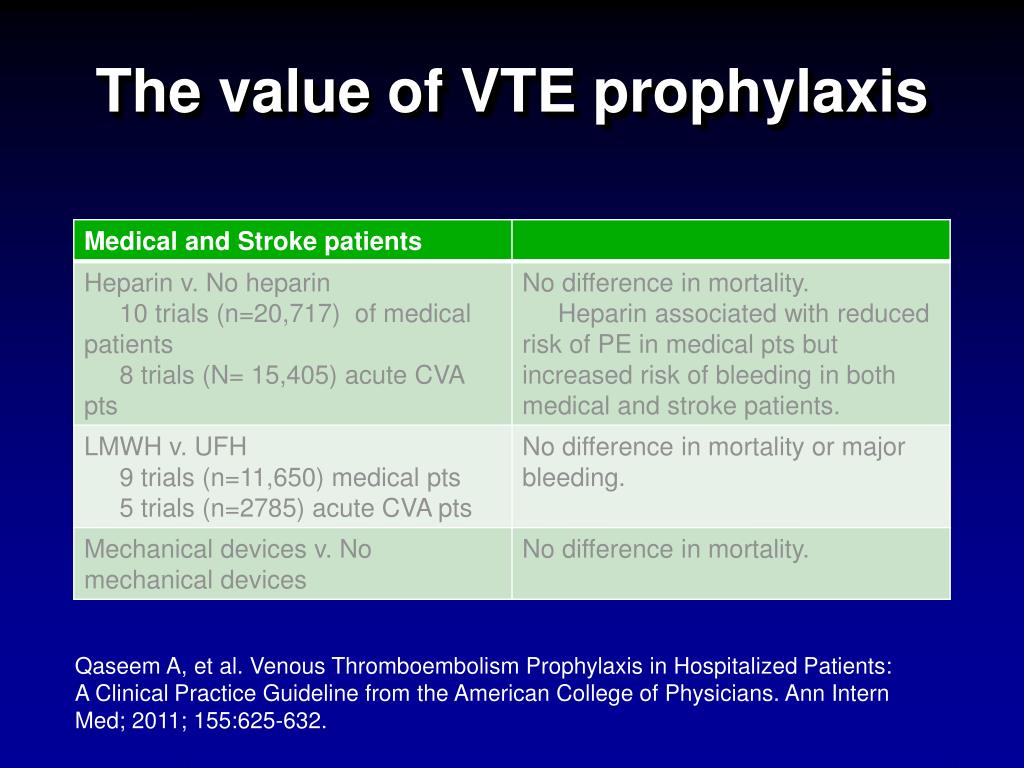
How effective is VTE prophylaxis?
Pharmacological VTE prophylaxis was independently associated with lower rates of major bleeding (OR = 0.42, 95%CI: 0.25-0.68, P = 0.0005), but was not significantly associated with a difference in rate of incident VTE (OR = 0.99, 95%CI: 0.48-2.06, P = 0.97).
Why is VTE important?
Without treatment, VTE can restrict or block blood flow and oxygen, which can damage the body's tissue or organs. This can be especially serious in the case of a pulmonary embolism, which blocks blood flow to the lungs. If a blood clot is large or there are many clots, a pulmonary embolism can cause death.
Who needs VTE prophylaxis?
Most hospitalized patients have at least one risk factor for venous thromboembolism (VTE), such as pulmonary embolism or deep venous thrombosis. The American College of Physicians (ACP) has released guidelines on VTE prophylaxis in hospitalized, nonsurgical patients, including those with acute stroke.
When is VTE prophylaxis contraindicated?
Some of the absolute contraindications for using pharmacologic VTE prophylaxis are known hypersensitivity to the drugs, current or previous heparin-induced thrombocytopenia and active bleeding, or risk of clinically significant bleeding.
What is VTE prevention?
VTEs often are preventable, with strategies that stop the development of clots in people "at-risk." Healthcare professionals discern risk by gathering information about a patient's age, weight, medical history, medications and lifestyle factors.
What is VTE prophylaxis in medical terms?
Definition. Venous thromboembolism (VTE) prophylaxis consists of pharmacological and non-pharmacological measures to diminish the risk of deep vein thrombosis (DVT) and pulmonary embolism (PE).
What is a DVT prophylaxis?
DVT prophylaxis can be primary or secondary. Primary prophylaxis is the preferred method with the use of medications and mechanical methods to prevent DVT. Secondary prophylaxis is a less commonly used method that includes early detection with screening methods and the treatment of subclinical DVT.
Why You Need To Understand VTE Prophylaxis
If a sick patient is sitting in bed for days, they can get a clot in their legs. Then, you get them up with PT/OT all of a sudden, and BOOM it moves to their lungs and now you have a PE (pulmonary embolism) on your hands, which can be fatal. The clot can also move to the brain and cause a stroke, which can also be fatal.
Order For VTE Prevention
With every admission you get, you should have an order for some sort of VTE prevention. It’s now part of most admission order sets and/or admission protocols. Typically, the only time nurses need to alert an MD about getting some sort of prophylaxis is if they didn’t use an admission order set, used a few general orders, and just forgot.
How To Prevent VTE Prophylaxis
There are a few different ways we prevent VTE’s.. below is a list of the least to most aggressive form.
Educate Patients About Using Them
Things to remember with your mechanical prevention (SCD’s, TED’s, ambulating, range of motion).. these are only effective if they’re being use or done. So if your patient that can’t sleep with SCD’s on refuses to wear them, make sure they understand the risk of not wearing them if subcut heparin isn’t also ordered.
What is a VTE?
Definition. Venous thromboembolism (VTE) prophylaxis consists of pharmacologic and nonpharmacologic measures to diminish the risk of deep vein thrombosis (DVT) and pulmonary embolism (PE). DVT of the leg is the development of a blood clot in one of the major deep veins in the leg or thigh, which leads to impaired venous blood flow, ...
What are the factors that affect the diagnosis of VTE?
chronic medical conditions, paresis, increasing age, obesity, estrogen-containing birth control pills and hormone replacement therapy, varicose veins, pregnancy and up to 6 week postpartum, first-degree relative with a history of VTE, extended travel, and admission to intensive care. More key diagnostic factors.
Why is thromboprophylaxis important?
Thromboprophylaxis is the most important patient safety strategy in patients admitted to the hospital. Pulmonary embolism remains the leading cause of preventable in-hospital death.
How many patients receive thromboprophylaxis?
Although national and international thromboprophylaxis guidelines have repeatedly recommended thromboprophylaxis of patients admitted to the hospital, only 40% to 50% of medical patients and 60% to 75% of surgical patients receive adequate thromboprophylaxis.
What is PE in pulmonary veins?
PE is a consequence of thrombus formation in distal veins, most commonly those of the deep venous system of the lower extremities . Thrombus formation in the venous system occurs as a result of venous stasis, trauma, and hypercoagulability. About 51% of deep venous thrombi will embolize to the pulmonary vasculature, resulting in a PE.