Add-on codes have no global period assigned. They are instead “included” in the global surgical fee for the primary procedure. Add-on codes are “modifier 51 exempt,” and therefore are to be paid at full fee schedule value. Their assigned value accounts for the “additional” nature of the procedure.
What is the proper use of modifier 51?
Procedure Coding: When to Use the Modifier 51
- DEFINING MODIFIER 51. As mentioned earlier, modifier 51 is primarily put to work for physicians who bill surgical services.
- CLINICAL SCENARIOS. In order to better understand exactly when to use modifier 51, let’s take a look at some examples of modifier 51 correctly in use for multiple surgical procedures.
- A LESSENING NEED FOR MODIFIER 51. ...
- SUMMARY. ...
When to add 51 modifier?
CPT guidelines explain the 51 modifier should apply when “multiple procedures, other than E/M services, are performed at the same session by the same individual. The additional procedure (s) or service (s) may be identified by appending modifier 51 to the additional procedure or service code (s).”
What is the difference between a 51 and 59 modifier?
While modifier 51 and 59 both apply to additional procedures performed on the same date of service as the primary procedure, modifier 51 differs from modifier 59 in that it applies to procedures that may be more commonly expected to be performed during the same session. Like modifier 51, modifier 59 should not be applied to an E/M service.
When to use mod 51?
What is Modifier -51 anyway? Modifier -51, Multiple Procedures. This modifier is used when reporting multiple procedures performed by the same physician on the same day. Do not use this modifier for “add-on” codes (see appendix D of the CPT Code book). Do not use this modifier for codes with “modifier -51 exempt” symbol (see appendix E of the CPT Code book).
Does the change affect reimbursement?
Can you bill a code bilaterally?
About this website
Are add on codes modifier exempt?
These codes can't be billed without a primary code, and the fee is already discounted as it is a secondary procedure. This is why add-on codes are “modifier 51 exempt” and, most of the time, you won't need to use any modifiers with CPT add-on codes.
What type of code is modifier 51 exempt?
What Type Of CPT Code Is Modifier 51 Exempt? The Symbol circle with the slash “Ø” indicates that the CPT code is exempt from modifier 51, such as CPT codes 19084, 64462, etc. In addition, add-on CPT codes are exempt from 51, and they cannot append with these CPT codes.
When should modifier 51 not be used?
Modifier 51 comes into play only when two or more procedures are performed. It is not to be used when a procedure is performed along with an Evaluation and Management (E/M) service. There are instances where multiple procedures are performed but modifier 51 is not appropriate.
When verifying if a CPT code is modifier 51 exempt what appendix would you use?
CPT® specifically identifies 93451 as exempt from modifier 51 (Multiple procedures). Appendix E in the CPT® manual lists the CPT® codes that are exempt from the use of Modifier 51.
Which CPT symbol conveys codes which are modifier 51 exempt?
The prohibition sign symbol is used to report codes that are exempt from modifier -51, but have not been designated as add-on procedures or services.
Which code does modifier 51 go on?
DEFINING MODIFIER 51 The additional procedure(s) or service(s) may be identified by appending modifier 51 to the additional procedure or service code(s).” In other words, modifier 51 reports that a physician performed two or more surgical services during one treatment session.
Does Medicare recognize modifier 51?
Medicare does not recommend reporting Modifier 51 on your claim; the processing system has hard-coded logic to append the modifier to the correct procedure code.
What does the 51 modifier mean?
Appending the correct modifier increases the likelihood that the claim will be paid the first time, correctly. Modifier 51 indicates that a second procedure was performed, and it is not a component code of the first procedure, that is, there is no procedure-to-procedure bundling edit.
What is the difference between modifier 50 and 51?
Modifier 50 Bilateral procedure describes procedures or services that take place on identical, opposing structures (e.g., shoulder joints, breasts, eyes). Use modifier 51 Multiple procedures to show that the same provider performed multiple procedures (other than E/M services) during the same session.
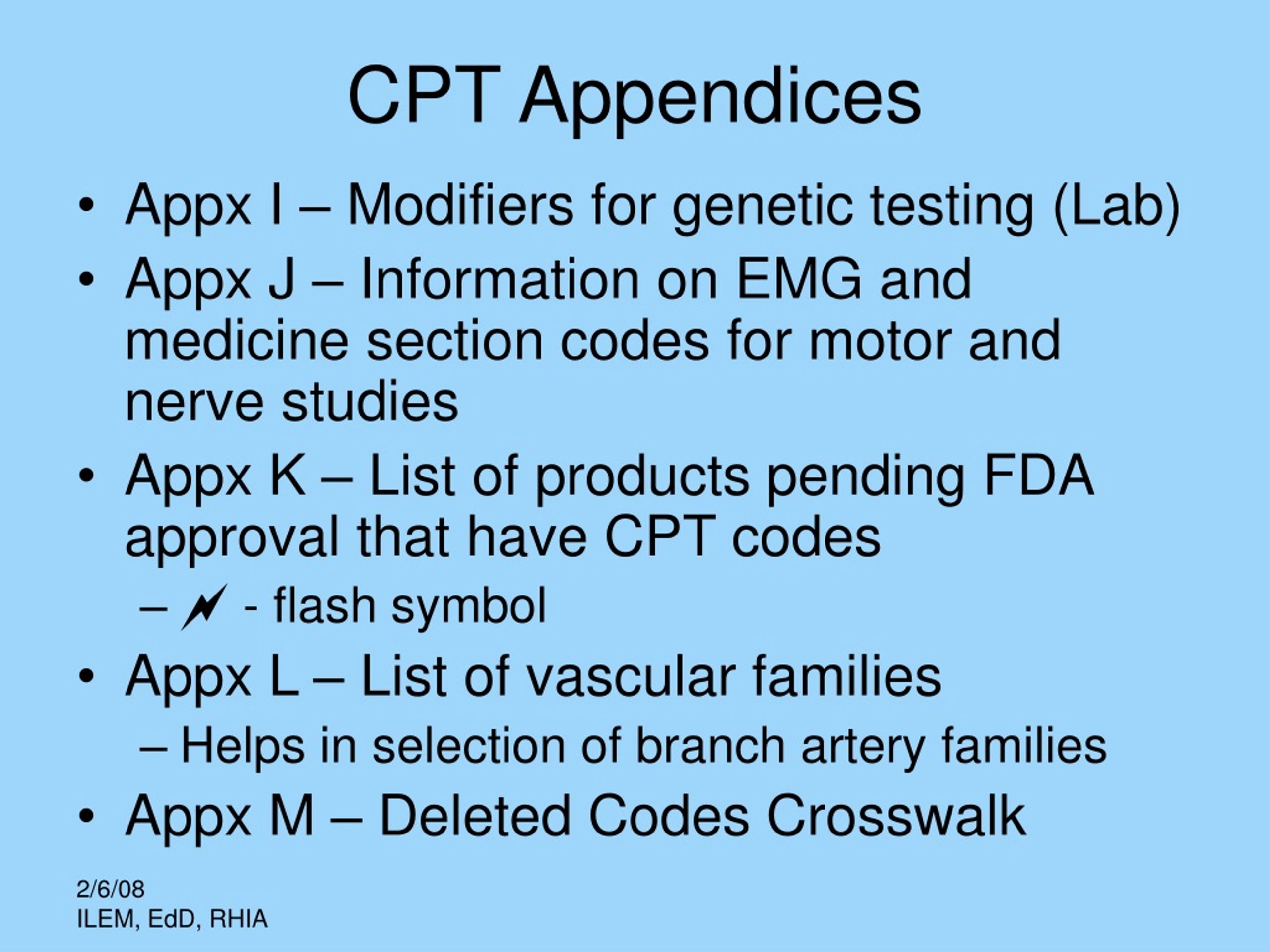
What appendix is codes exempt from modifier?
Appendix ERATIONALE: Codes exempt from modifier 51 are identified with the universal “forbidden” symbol. Add-on codes are also exempt from modifier 51. A list of modifier 51 exempt codes can be found in Appendix E of the CPT® codebook.
What does Resequenced code mean?
A resequenced code comes about when a new code is added to a family of codes but a sequential number is unavailable. A second exception to numerical code order involves evaluation and management (E/M) codes.
Which of the following codes allows the use of modifier 51 quizlet?
A. Modifier 51 must be used with procedure code 20974.
Does Medicare accept the 51 modifier?
Medicare does not recommend reporting Modifier 51 on your claim; the processing system has hard-coded logic to append the modifier to the correct procedure code.
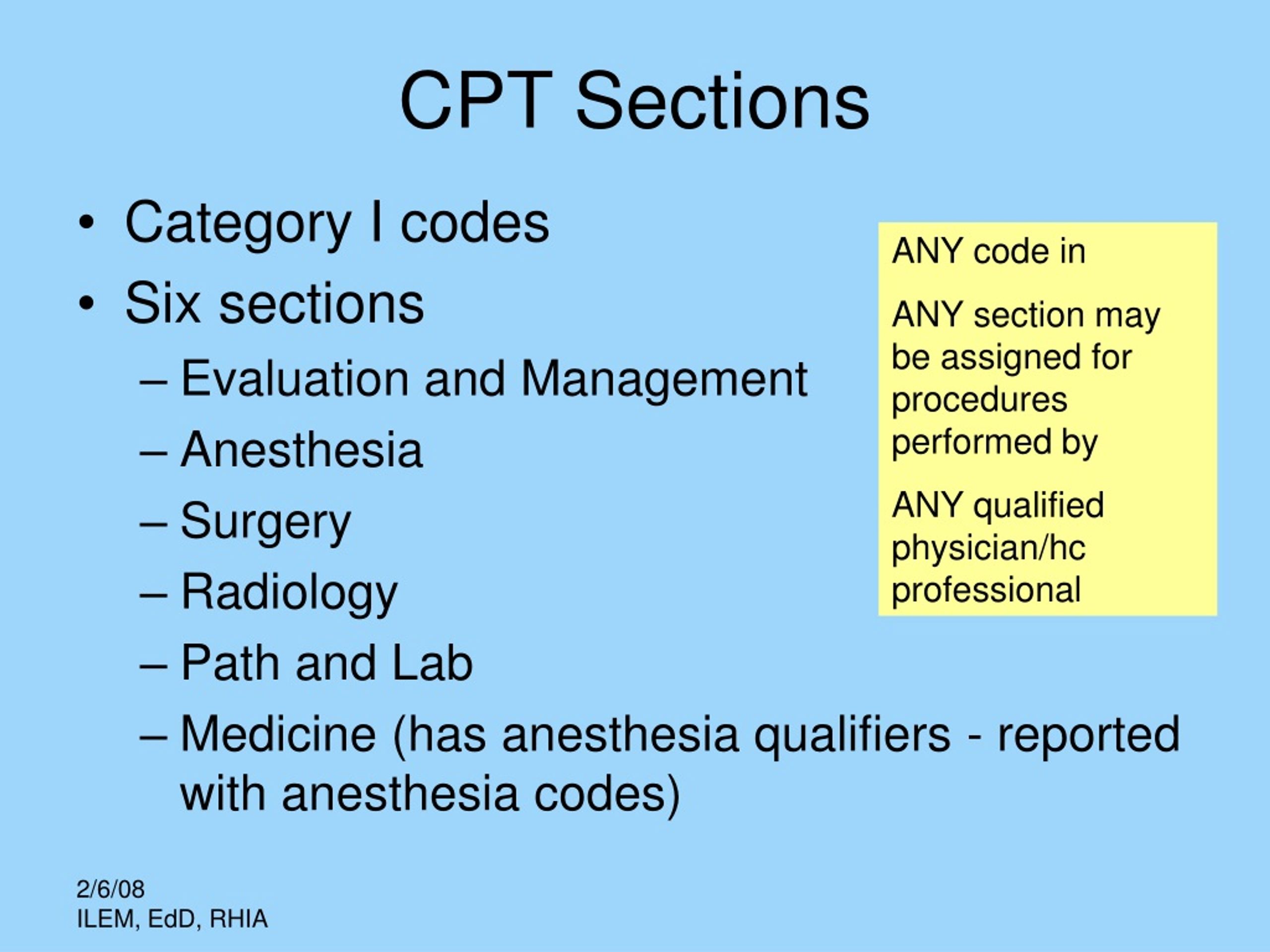
What are the three categories of CPT codes?
Types of CPTCategory I: These codes have descriptors that correspond to a procedure or service. ... Category II: These alphanumeric tracking codes are supplemental codes used for performance measurement. ... Category III: These are temporary alphanumeric codes for new and developing technology, procedures and services.More items...
Modifier 51 Fact Sheet - Novitas Solutions
Note: Medicare doesn’t recommend reporting Modifier 51 on your claim; our processing system will append the modifier to the correct procedure code as appropriate. Appropriate System Usage
New CPT Modifier Rule: Add-on Codes - Bilateral (50) -vs- Right (RT ...
New CPT Modifier Rule: Add-on Codes - Bilateral (50) -vs- Right (RT) and Left (LT) Published on February 18, 2020. As if pain management billing wasn’t complex enough, now the AMA has changed the guidelines for bilateral procedures.
Modifier 51 Code- The Secrets Revealed! (2022) - Medical Billing RCM
What is modifier 51? Modifier 51 can be defined as a is used frequently when the provider performs surgical services. According to the CPT guidelines, mod 51 should be applied when various procedures besides the E/M services are performed in a similar situation by the same person.
Modifier 50 Fact Sheet - Novitas Solutions
Modifier 50 fact sheet. Effective for claims received on and after August 16, 2019, services will be rejected as unprocessable when the procedure code reported is inconsistent with the modifier used.. The modifier 50 is defined as a bilateral procedure performed on both sides of the body.
Article - Billing and Coding: Facet Joint Interventions for Pain ...
Group 2 Paragraph. The following CPT/HCPCS codes are non-covered*: * this is not an inclusive list of non-covered codes *Note: 64492 or 64495 describes a third and additional levels and should be listed separately in addition to the code for the primary procedure and the second level procedure and cannot be reported more than once per day. 64492 should be reported in conjunction with 64490/ ...
Does the change affect reimbursement?
The change does not affect your reimbursement, only how it gets broken down.
Can you bill a code bilaterally?
Also remember that not all codes (whether add on or otherwise), qualify to be billed bilaterally.
What is a multiple procedure?
Multiple Procedures. When multiple procedures, other than Evaluation and Management (E/M), Physical Medicine and Rehabilitation services or provisions of supplies (e.g., vaccines) are performed at the same session by the same individual, the primary procedure or service may be reported as listed. Multiple procedure rules apply to the secondary procedure or service.
Can you append modifier 51 to procedure code?
Do not append modifier 51 to the additional procedure code. The Medicare claim processing system has a hard coded logic to append it to the correct procedure code. CPT also lists codes that are modifier 51 exempt.
What is modifier 51?from carecloud.com
Modifier 51 is a modifier you probably use frequently if your provider performs surgical services. However, this particular modifier is exceptional in regards to where and how it should be appended. This is because for modifier 51, appropriate coding must take into consideration the RVU (relative value units) of the performed CPTs in order ...
Does Medicare pay for multiple surgeries?from novitas-solutions.com
Additional Information. Medicare pays for multiple surgeries by ranking from the highest physician fee schedule amount to the lowest physician fee schedule amount. Medicare will forward the claim information showing Modifier 51 to the secondary insurance.
What is modifier 51?from medicalbillingrcm.com
Modifier 51 can be defined as a is used frequently when the provider performs surgical services.
What is a multiple procedure?from med.noridianmedicare.com
Multiple Procedures. When multiple procedures, other than Evaluation and Management (E/M), Physical Medicine and Rehabilitation services or provisions of supplies (e.g., vaccines) are performed at the same session by the same individual, the primary procedure or service may be reported as listed. Multiple procedure rules apply to the secondary procedure or service.
Does Medicare pay for multiple surgeries?from novitas-solutions.com
Additional Information. Medicare pays for multiple surgeries by ranking from the highest physician fee schedule amount to the lowest physician fee schedule amount. Medicare will forward the claim information showing Modifier 51 to the secondary insurance.
What is the correct modifier for multiple procedures?
Modifier 51 is considered valid for procedures with a multiple procedure indicator of 2, 3, 4, 5, 6, or 7.
What modifier should be added to a secondary procedure code?
The secondary, additional, or lesser procedure (s) may be listed and identified by adding the modifier 51 to the secondary procedure code (s). This modifier should not be appended to designated “addon” codes.
How much is reimbursed for single surgical field?
Single surgical field or single surgical incision – Multiple procedures performed by one or two surgeons, regardless of how many organ systems are involved, will be reimbursed at 100 percent for the procedure commanding the greatest value and 50 percent for the second or subsequent procedures .
What is the standard payment adjustment rule for multiple procedures?
2 = Standard payment adjustment rules for multiple procedures apply. If the procedure is reported on thesame day as another procedure with an indicator of 1, 2, or 3, rank the procedures by fee schedule amount and apply the appropriate reduction to this code (100 percent, 50 percent, 50 percent, 50 percent, 50 percent, and by report). Base payment on the lower of: (a) the actual charge or (b) the fee schedule amount reduced by the appropriate percentage.
When to apply multiple endoscopy rules?
Apply the multiple endoscopy rules to a family before ranking the family with other procedures performed on the same day (for example, if multiple endoscopies in the same family are reported on the same day as endoscopies in another family or on the same day as a non-endoscopic procedure).
Does Medicare require a modifier 51?
Medicare does not recommend reporting Modifier 51 on your claim; the processing system has hard-coded logic to append the modifier to the correct procedure code. Definition: • Multiple surgeries performed on the same day, during the same surgical session.
Can you append modifier 51 to a secondary procedure?
Multiple procedure rules apply to the secondary procedure or service. Instructions. Do not append modifier 51 to the additional procedure code. The Medicare claim processing system has a hard coded logic to append it to the correct procedure code. CPT also lists codes that are modifier 51 exempt.
Does the change affect reimbursement?
The change does not affect your reimbursement, only how it gets broken down.
Can you bill a code bilaterally?
Also remember that not all codes (whether add on or otherwise), qualify to be billed bilaterally.
