Does insulin glargine cross the placenta?
After perfusion with very high insulin glargine concentrations of 150, 225, and 300 nmol/l, the rate of transfer remained low at 0.079 0.01, 0.14, and 0.064 pmol min1 g tissue1, respectively. ConclusionsInsulin glargine, when used at therapeutic concentrations, is not likely to cross the placenta. Several new long-acting insu Continue reading >>
How does gestational diabetes affect the placenta?
Gestational diabetes produces changes in placenta secondary to change in the milieu of the mother and the fetus. To compensate the hyperglycemic blood from the mother, there is islets cell hypertrophy and beta cell hyperplasia of fetal pancreas with the release of excessive amounts of insulin in the fetal body.
What drugs do not cross the placenta?
Alcohol, for example, readily reaches the embryo in fairly high concentrations. On the other hand, high molecular-weight drugs like heparin (20,000 daltons) do not cross the placenta. It is therefore widely used to treat hypercoagulation during pregnancy.
How does insulin transport across the blood-brain barrier?
A saturable system transports insulin from blood across the blood-brain barrier (BBB) and into the central nervous system. Whether or not the classic or signalling-related insulin receptor plays a role in mediating this transport in vivo is controversial.
How does insulin affect my unborn baby?
Your doctor may prescribe it when your body doesn't make enough on its own to keep your blood sugar levels in a normal range. That will help prevent problems for you and your baby. Insulin doesn't cross the placenta, which means it can't get to your baby, so it's safe to use as prescribed.
Why does the placenta block insulin?
The placenta supplies a growing fetus with nutrients and water, and also produces a variety of hormones to maintain the pregnancy. Some of these hormones (estrogen, cortisol, and human placental lactogen) can have a blocking effect on insulin.
Is there maternal transfer of insulin during pregnancy?
Conclusions: Considerable amounts of antibody-bound insulin are transferred from mother to fetus during pregnancy in some women with insulin-dependent diabetes mellitus; the extent of transfer correlates with the maternal concentration of anti-insulin antibody.
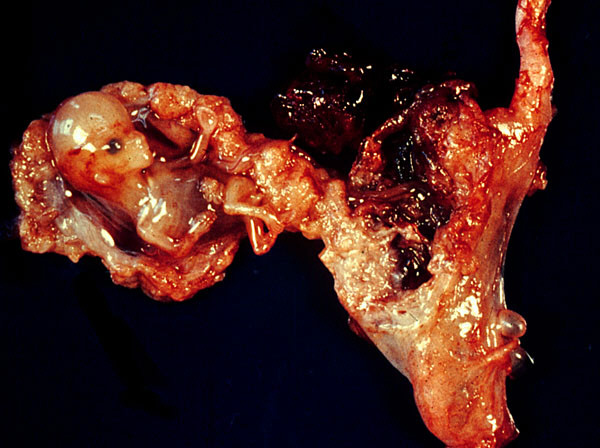
Does insulin deteriorate the placenta?
Insulin is directly toxic to early placenta and elevated levels can lead to pregnancy loss, according to new research. Metformin, a low-cost medication for diabetes management, as well as diet modifications in the form of reduced carbohydrates and sugar have shown promise in potentially preventing miscarriage.
How does insulin resistance affect pregnancy?
Women are insulin resistant when their bodies do not respond to insulin's action to handle sugar as they normally should. Because of this insulin resistance, when women with the polycystic ovary syndrome become pregnant, they are at a higher risk of developing gestational diabetes.
When is insulin resistance highest in pregnancy?
At 12–14 weeks' gestation, insulin sensitivity is slightly increased but then declines for the rest of the pregnancy, with insulin resistance being highest late in the third trimester.
How many units of insulin is safe during pregnancy?
In the first trimester, the total daily insulin requirement is 0.7 units/kg/day, in the second trimester it is 0.8 units/kg/day, and in the third trimester it is 0.9-1.0 units/kg/day.
Does metformin cross the placenta?
For more than 40 years, metformin has been used before and during pregnancy. However, it is important to note that metformin can cross the placenta and circulate in the developing foetus.
Which insulin is preferred in pregnancy?
Insulin detemir is preferred over insulin glargine because it has been studied more extensively in pregnancy and can be dosed twice per day more predictably than glargine, as previously mentioned. (See "General principles of insulin therapy in diabetes mellitus", section on 'Safety'.)
How does diabetes affect the placenta?
Diabetes-induced placental malformation decreases placental efficiency and fetal size. Hyperglycemia disrupts rat trophoblast stem cell differentiation into invasive trophoblast. Diabetes impairs intrauterine trophoblast invasion. Hyperglycemia adversely affects placental adaptations to hypoxia.
Why does the placenta cause gestational diabetes?
As the placenta grows, it makes more of the hormones. The risk for insulin resistance becomes greater. Normally your pancreas is able to make more insulin to overcome insulin resistance. But if it can't make enough to overcome the effects of the placenta's hormones, you can develop gestational diabetes.
What are the signs of placental insufficiency?
Placental insufficiency has no symptoms. Sometimes it's diagnosed when women realise their baby isn't moving as much. Other signs the baby may not be developing properly are that your abdomen is smaller than in previous pregnancies.
How do you know if your placenta is failing with gestational diabetes?
A sudden drop in blood sugar levels – levels dropping much lower than usual for you to very low levels (2.0's – 3.0's mmol/L) consistently can be a sign that there are issues with the function of the placenta. It is best to consult a medical professional if you see a drop in levels like this.
How do I fight insulin resistance during pregnancy?
A low-glycemic diet combined with a low-volume exercise regimen during pregnancy decreases the glucose and insulin response to both mixed caloric intake and exercise, and probably lowers both 24-h blood glucose concentrations and the maternal substrate utilization ratio of carbohydrate/fat.
Can Bacteria Cross Through The Placenta From Yhe Mother To The Fetus?
Yes it is possible. This happens in a number of scenarios where A mother's immunity is compromised The placenta barriers have been compromised as in the case of an accident which might allow for its damager Please refer to the link below. I found it helpful Ask New Question Continue reading >>
Does Insulin Cross The Placenta?
Doctor: Insulin crosses the placenta in very small amounts, insufficient to cause any harm to the unborn baby. On the other hand , increased sugar levels may affect your baby with macrosomia (large baby), birth defects, hypoglycemia after birth, increased chances of C-section due to large baby etc. Thus you need not be concerned about the increased amounts of insulin, but need to keep your sugar levels in control to avoid any harmful effects on your baby. Continue reading >>
How does gestational diabetes affect the placenta?
Gestational diabetes produces changes in placenta secondary to change in the milieu of the mother and the fetus. To compensate the hyperglycemic blood from the mother, there is islets cell hypertrophy and beta cell hyperplasia of fetal pancreas with the release of excessive amounts of insulin in the fetal body. This results in a hyper-insulinemic state in the fetus with the up regulation of many genes expression, inflammatory mediators and leptin in placental tissues. This whole process probably produces excessive growth and increase in placental weight. Increased placental volume compensates the need of growing babies to an extent and after that hypoxic state generates leading to adverse fetal and maternal outcomes even unexplained termed intrauterine deaths. Placental tissues are liable to change with maternal metabolic issues. Our results have shown increase in placental weight in both the groups but a significant increase in placental weight is observed when glycemic control was done with diet control plus injectable insulin as compared to diabetics controlled on diet and exercise only. This indicates that exogenous insulin has exerted more effects on the placenta than the other group. According to Boyd, placental parenchymal tissues of insulin treated patients were much heavier in volume.15Mayhew and Chowdhury worked on insulin treated diabetic pregnancies and found that GDM placental weights were significantly increased. The results of both these studies are in favor of our findings.16,17Placental cord length, membrane completeness, placental shape, consistency, cord insertion, cord color and gross pathologies showed non-significant results between the two groups but with more propensities in the insulin treated group. Verma has discussed that on major gross examination of placentae, there were non-significant differences which is just similar to our results.18It has been documented in literature that acute pulsatile rise and fall in the mother’s blood sugars as after food intake (hyperglycemia) and insulin treatment (hypoglycemia) might be unnoticed and account for increased fetal release of endogenous insulin resulting in big placenta and babies as compared to females on diet restricted therapy which is again in favor of our study.19
Why is the cord thicker in diabetic placentae?
The relevance of these factors with the diabetic environment is yet to be evaluated but the probable reason of excessive growth of the cord tissue which makes it thicker is the effect of fetal insulin. Although non-significant statistically but more fibronoid necrosis was seen in insulin treated placentae. As per literature this type of necrosis is indication of placental compromise and therefore decreased supply of nutrients and oxygen to the growing fetus leading to hypoxia.20
Why are GDM babies heavier than diet control?
Persson stated that babies of GDM mothers on insulin treatment and on diet control are similar in the weight.23But a recent study by Wong has proven the fact that the babies of insulin treated GDM were heavier than diet control GDM mothers, so more GDM mothers on insulin treatment delivered through cesarean section due to fetal overgrowth and heavy term babies24and is coinciding with our findings. We observed more intrauterine deaths in insulin treated group and the probable reason is the excessive growth of fetus which increases the oxygen demands. Placenta tries to compensate this to an extent but when the baby is grown enough and is near term, it cannot fulfill the requirements of fetus resulting in unexplained term intrauterine death in these patients.25Our findings suggest that exogenous insulin probably improves the glycemic values but is unable to control the related problems completely as is evident from statistics. This point towards the presence of unknown areas in GDM pathology and need of alternative pharmacotherapy for GDM patients.
Why are babies heavier in GDM?
When fetal outcomes were compared , it was seen that babies were much heavier in patients in insulin treated GDM group as compared to diet controlled group. Odar has stated that increased fetal weights leads to bad maternal and fetal outcomes, which is again similar to our study and the reason behind is the hyper-insulinemic state of the fetus affecting both the placental and fetal growth.21Jansson described that probably excessive fetal growth is the result of increase in substrate availability which stimulates fetal insulin secretion and fetal growth. However, despite of strict glycemic control in modern clinical management of the pregnant woman with significant hyperglycemia, fetal overgrowth remains an important clinical problem. Recent studies have provided enough evidence for increased delivery of amino acids to the fetus in gestational diabetes (GDM), even when metabolic control is strict. So might be for this reason even when truly normal maternal substrate levels are achieved in diabetic pregnancies, the defect lies in altered placental nutrient transport and metabolism.22
How to control blood glucose levels in the mother?
Blood glucose levels in the mother can be controlled by nutritional therapy (diet control) and exercise but in uncontrolled cases, where target glycemic levels could not be achieved medication are also required. Subcutaneous insulin is the traditional therapy and gold standard under such circumstances.9Even with this pharmacotherapy, fetal and maternal morbidity and mortality are well documented in the literature.10Morphological study of placenta which occupies central position between the mother and fetus might be helpful in elucidating these adverse fetal and maternal outcomes in gestational diabetes. With this background present study was designed to observe the effect of exogenous insulin on the gross morphology of placenta, fetal and maternal outcomes in gestational diabetics in our setting.
Does insulin affect placental outcomes?
Insulin has produced significant effects on the placental, fetal and maternal outcomes in patients having gestational diabetes mellitus in comparison to GDMs controlled on diet and exercise.
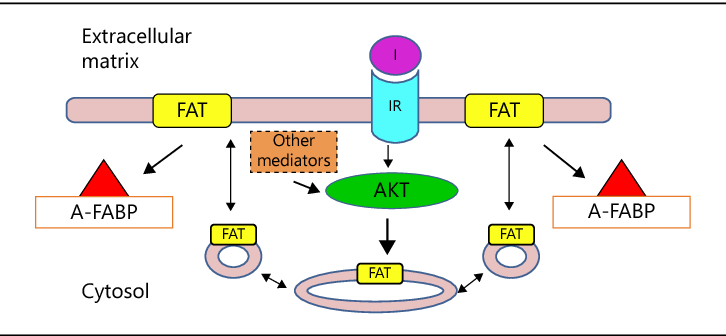
How does insulin enter the brain?
Key points: Insulin enters the brain from the blood via a saturable transport system. It is unclear how insulin is transported across the blood-brain barrier (BBB). Using two models of the signalling-related insulin receptor loss or inhibition, we show insulin transport can occur in vivo without the signalling-related insulin receptor. Insulin in the brain has multiple roles including acting as a metabolic regulator and improving memory. Understanding how insulin is transported across the BBB will aid in developing therapeutics to further increase CNS concentrations.
Which system transports insulin from blood to the central nervous system?
A saturable system transports insulin from blood across the blood-brain barrier (BBB) and into the central nervous system. Whether or not the classic or signalling-related insulin receptor plays a role in mediating this transport in vivo is controversial. Here, we employed kinetics methods that dist …
What factors determine what drugs cross the placental barrier?
The primary determining factors of what type of drugs will cross the placental barrier are molecular weight, lipid (fat or fat-like) solubility, polarity (molecular charge), protein binding, and receptor mediation. Drugs that have low molecular weight, lipid (fat) solubility, nonpolarity, and no protein binding properties will quickly ...
Does alcohol cross the placenta?
Drugs that have low molecular weight, lipid (fat) solubility, nonpolarity, and no protein binding properties will quickly and easily cross the placenta. Alcohol, for example, readily reaches the embryo in fairly high concentrations. On the other hand, high molecular-weight drugs like heparin (20,000 daltons) do not cross the placenta.
Can Zofran be taken while pregnant?
Beware of Zofran While Pregnant. Zofran (ondansetron) has properties that cause it to easily cross the placenta in substantial amounts. Just for example, it has great lipid solubility, low molecular weight (365.9 daltons), and a measured in vitro plasma protein binding of 70% to 76%.
Does Zofran cause birth defects?
Zofran has now been shown to significantly increase the risk of birth defects in pregnant mothers who take it during the first trimester.
Do drugs cross the placenta?
While there is no true “barrier” between the mother and her fetus, there is a semipermeable membrane made up of placental tissues that limit the kind and amount of material that can be passed along from the mother. The fact is that most drugs do cross the placenta in some amount.
RESEARCH DESIGN AND METHODS
The eight human placentae were obtained after vaginal or cesarean section delivery from uncomplicated term pregnancies and transported to the laboratory in heparinized ice-cold PBS.
RESULTS
The mean mass of the perfused cotyledons was 11.8 ± 3.4 g. Placental glucose and oxygen consumption and oxygen delivery and transfer as indicators of metabolic viability of the placental tissue did not change significantly throughout the perfusion experiment ( Table 1 ).
CONCLUSIONS
The placental perfusion model enables the noninvasive collection of information regarding human placental transfer of molecules ( 15 ). Because transfer is measured in intact tissue, the model approximates the in vivo situation more closely than subcellular or cell culture systems.
Article Information
This study was supported by grants from the Canadian Institute of Health Research (CIHR), by Eli Lilly Canada, and by the Research Leadership for Pharmacotherapy During Pregnancy and Lactation. G.K. is a senior scientist of CIHR. R.B. is supported by a Fellowship from the Canadian Society for Clinical Pharmacology.