Precautions
The intravenous administration of furosemide is indicated when a rapid onset of diuresis is desired, e.g., in acute pulmonary edema. If gastrointestinal absorption is impaired or oral medication is not practical for any reason, furosemide is indicated by the intravenous or intramuscular route.
Can furosemide be given intravenously?
Each mL of Oral Solution for oral administration contains: Furosemide is a diuretic which is an anthranilic acid derivative. Chemically, it is 4-chloro- N -furfuryl-5-sulfamoylanthranilic acid. Furosemide is a white to slightly yellow, crystalline powder.
What is in furosemide oral solution?
For patients not receiving long-term loop diuretic agents, 40-80 mg IV BID of furosemide or the equivalent is a reasonable, empiric, starting dose. Due to post-dosing Na + retention, IV loop-diuretic agents should usually be given at least twice daily.
How many milligrams of Furosemide should I take for UTI?
How does furosemide affect kidney function?
How much furosemide is equivalent to bumetanide?
What are the symptoms of furosemide overdose?
What is the interprofessional team for hypervolemia?
How long does furosemide stay in your system?
What is furosemide used for?
What is the best diuretic for liver cirrhosis?
See 2 more
About this website
Furosemide Injection Description
Furosemide is a diuretic which is an anthranilic acid derivative. Chemically it is 4-chloro-N-furfuryl-5-sulfamoylanthranilic acid.Furosemide is a...
Furosemide Injection - Clinical Pharmacology
Investigations into the mode of action of furosemide have utilized micropuncture studies in rats, stop flow experiments in dogs and various clearan...
Indications and Usage For Furosemide Injection
Parenteral therapy should be reserved for patients unable to take oral medication or for patients in emergency clinical situations.
Furosemide Injection Dosage and Administration
AdultsParenteral therapy with Furosemide Injection, USP should be used only in patients unable to take oral medication or in emergency situations a...
How Is Furosemide Injection Supplied
Furosemide Injection, USP 10 mg/mL is supplied as follows:Store at 20 to 25°C (68 to 77°F). [See USP Controlled Room Temperature.]Do not use if sol...
Principal Display Panel - 10 Ml Syringe Label
Furosemide 100 mg/10 mL (10 mg/mL)10 mL Single-dose syringeNDC 0409-1639-21Rx onlyFurosemide Injection, USP100 mg/10 mL (10 mg/mL)For Intravenous o...
Principal Display Panel - 10 Ml Syringe Carton
NDC 0409-1639-21Rx only10 mLFurosemideInjection, USP100 mg/10 mL(10 mg/mL)PROTECT FROM LIGHTFor Intravenous orIntramuscular use.Ansyr™Single-dose S...
Principal Display Panel - 2 Ml Vial Label
2 mLNDC 0409-6102-19Rx onlyFurosemide Inj., USP20 mg/2 mL (10 mg/mL)RL-4988Hospira, Inc.Lake Forest, IL 60045 USAHospira
Principal Display Panel - 2 Ml Vial Tray
2 mL Single-use vials25 Units/NDC 0409-6102-02Rx onlyFurosemide Injection, USP20 mg/2 mL (10 mg/mL)For INTRAVENOUS or INTRAMUSCULAR use. Protect fr...
Principal Display Panel - 4 Ml Vial Label
4 mL Single-use vialRx onlyFurosemideInjection, USP40 mg/4 mL (10 mg/mL)FOR INTRAVENOUS ORINTRAMUSCULAR USE.Hospira, Inc.Lake Forest, IL 60045 USA
How does furosemide affect embryos?
The effects of furosemide on embryonic and fetal development and on pregnant dams were studied in mice, rats and rabbits. Furosemide caused unexplained maternal deaths and abortions in the rabbit at the lowest dose of 25 mg/kg (2 times the maximal recommended human oral dose of 600 mg/day).
How long does it take for furosemide to absorb?
Although furosemide is more rapidly absorbed from the oral solution (50 minutes) than from the tablet (87 minutes), peak plasma levels and area under the plasma concentration-time curves do not differ significantly. Peak plasma concentrations increase with increasing dose but times-to-peak do not differ among doses.
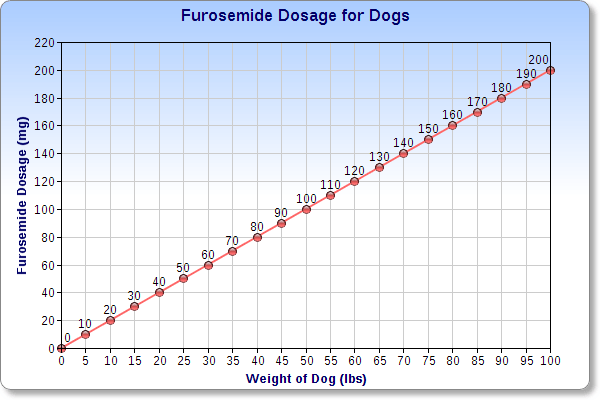
How much furosemide is toxic to dogs?
In all three, the oral LD 50 exceeded 1000 mg/kg body weight, while the intravenous LD 50 ranged from 300 to 680 mg/kg. The acute intragastric toxicity in neonatal rats is 7 to 10 times that of adult rats.
How long does furosemide stay in your system?
The terminal half-life of furosemide is approximately 2 hours. Significantly more furosemide is excreted in urine following the intravenous injection than after the tablet or oral solution. There are no significant differences between the two oral formulations in the amount of unchanged drug excreted in urine.
What are the symptoms of furosemide?
All patients receiving furosemide therapy should be observed for these signs or symptoms of fluid or electrolyte imbalance (hyponatremia, hypochloremic alkalosis, hypokalemia, hypomagnesemia or hypocalcemia): dryness of mouth, thirst, weakness, lethargy, drowsiness, restlessness, muscle pains or cramps, muscular fatigue, hypotension, oliguria, tachycardia, arrhythmia or gastrointestinal disturbances such as nausea and vomiting.
What is the chemical name for furosemide?
Chemically, it is 4-chloro- N -furfuryl-5-sulfamoylanthranilic acid. Furosemide Injection, USP 10 mg/mL is a sterile, non-pyrogenic solution in vials for intravenous and intramuscular injection. Furosemide USP is a white to slightly yellowish, odorless crystalline powder.
When should furosemide be reduced?
Whenever adverse reactions are moderate or severe, furosemide dosage should be reduced or therapy withdrawn.
What is furosemide used for?
Furosemide is particularly useful when an agent with greater diuretic potential is desired.
How long does it take for furosemide to absorb?
Although furosemide is more rapidly absorbed from the oral solution (50 minutes) than from the tablet (87 minutes), peak plasma levels and area under the plasma concentration-time curves do not differ significantly. Peak plasma concentrations increase with increasing dose but times-to-peak do not differ among doses.
What are the symptoms of overdose on furosemide?
The principal signs and symptoms of overdose with furosemide are dehydration, blood volume reduction, hypotension, electrolyte imbalance, hypokalemia and hypochloremic alkalosis, and are extensions of its diuretic action. The acute toxicity of furosemide has been determined in mice, rats and dogs.
How long does furosemide last?
The duration of diuretic effect is 6 to 8 hours. In fasted normal men, the mean bioavailability of furosemide from Furosemide Tablets and Furosemide Oral Solution is 64% and 60%, respectively, of that from an intravenous injection of the drug.
How much furosemide is toxic to dogs?
In all three, the oral LD 50 exceeded 1000 mg/kg body weight, while the intravenous LD 50 ranged from 300 to 680 mg/kg. The acute intragastric toxicity in neonatal rats is 7 to 10 times that of adult rats.
Does furosemide cause muscle pain?
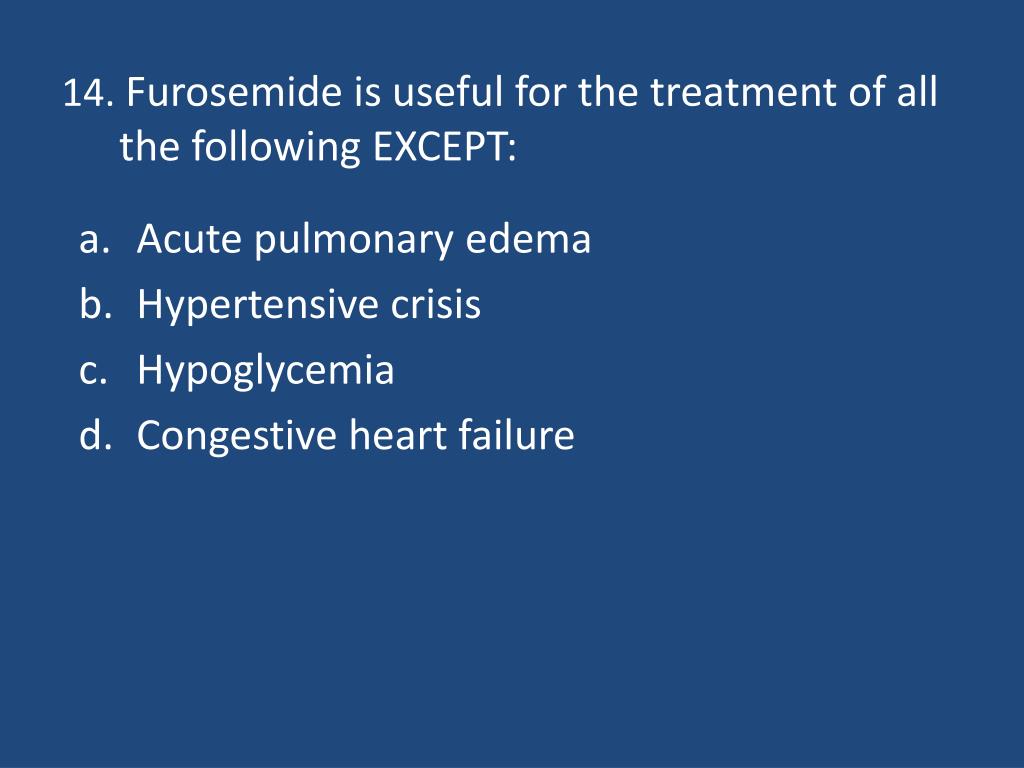
All patients receiving furosemide therapy should be observed for these signs or symptoms of fluid or electrolyte imbalance (hyponatremia, hypochloremic alkalosis, hypokalemia, hypomagnesemia or hypocalcemia): dryness of mouth, thirst, weakness, lethargy, drowsiness, restlessness, muscle pains or cramps, muscular fatigue, hypotension, oliguria, tachycardia, arrhythmia, or gastrointestinal disturbances such as nausea and vomiting. Increases in blood glucose and alterations in glucose tolerance tests (with abnormalities of the fasting and 2-hour postprandial sugar) have been observed, and rarely, precipitation of diabetes mellitus has been reported.
Can furosemide cause dehydration?
Excessive diuresis may cause dehydration and blood volume reduction with circulatory collapse and possibly vascular thrombosis and embolism, particularly in elderly patients. As with any effective diuretic, electrolyte depletion may occur during furosemide therapy, especially in patients receiving higher doses and a restricted salt intake. Hypokalemia may develop with furosemide, especially with brisk diuresis, inadequate oral electrolyte intake, when cirrhosis is present, or during concomitant use of corticosteroids, ACTH, licorice in large amounts, or prolonged use of laxatives. Digitalis therapy may exaggerate metabolic effects of hypokalemia, especially myocardial effects.
How long does furosemide take to absorb?
Diuresis generally begins 30 to 60 minutes after oral administration. Intravenous Route. Diuresis generally begins about 5 minutes after IV administration of furosemide.
What is furosemide used for?
Furosemide is a loop diuretic that inhibits sodium and chloride resorption by competing with chloride for the Na+/K+/2Cl- co-transporter in the ascending limb of the loop of Henle. The manufacturer also states that furosemide inhibits the absorption of sodium and chloride in the proximal and distal tubules.
What is the difference between etomidate and exenatide?
Etomidate: (Moderate) General anesthetics can potentiate the hypotensive effects of antihypertensive agents. Ex enatide: (Minor) Loop diuretics, such as bu metanide, furosemide, and torsemide, may cause hyperglycemia and glycosuria in patients with diabetes mellitus, probably due to diuretic-induced hypokalemia.
How long does it take for furosemide to be excreted?
Furosemide undergoes minimal metabolism in the liver, with 50—80% of a dose excreted in the urine within 24 hours. The remainder of the drug is eliminated through nonrenal mechanisms including excretion in the feces. In patients with significant renal impairment, nonrenal elimination can increase to 98%.
How to administer furosemide to a child?
When administering furosemide to an infant or child using a medicine dropper or oral syringe, slowly squirt the solution into the side of the child's mouth so that he or she will swallow the liquid naturally. Do not squirt onto the back of the throat because this may cause gagging. Rinse the dropper or syringe in warm water after each use.
Can you give furosemide to a breastfeeding mother?
Use caution when administering furosemide to a breast-feeding mother. Furosemide is excreted in human breast milk. In addition, furosemide may suppress lactation as a result of intense diuresis. Previous American Academy of Pediatrics (AAP) recommendations considered chlorthalidone, chlorothiazide, and hydrochlorothiazide as usually compatible with breast-feeding.
Can furosemide cause ototoxicity?
High doses and accumulation of furosemide may cause ototoxicity. Use furosemide with caution in patients with hearing impairment. Do not exceed the recommended rate of infusion when IV doses are administered.
What are the symptoms of overdose on furosemide?
The principal signs and symptoms of overdose with furosemide are dehydration, blood volume reduction, hypotension, electroly te imbalance, hypokalemia and hypochloremic alkalosis, and are extensions of its diuretic action.The acute toxicity of furosemide has been determined in mice, rats and dogs. In all three, the oral LD50 exceeded1000 mg/kg body weight, while the intravenous LD50 ranged from 300 to 680 mg/kg. The acute intragastric toxicity inneonatal rats is 7 to 10 times that of adult rats.
Is furosemide carcinogenic?
Carcinogenesis, Mutagenesis, Impairment of Fertility: Furosemide was tested for carcinogenicity by oral administrationin one strain of mice and one strain of rats. A small but significantly increased incidence of mammary gland carcinomasoccurred in female mice at a dose 17.5 times the maximum human dose of 600 mg. There were marginal increases inuncommon tumors in male rats at a dose of 15 mg/kg (slightly greater than the maximum human dose) but not at
Can furosemide cause dehydration?
General: Excessive diuresis may cause dehydration and blood volume reduction with circulatory collapse and possiblyvascular thrombosis and embolism, particularly in elderly patients. As with any effective diuretic, electrolyte depletion mayoccur during furosemide therapy, especially in patients receiving higher doses and a restricted salt intake. Hypokalemiamay develop with furosemide, especially with brisk diuresis, inadequate oral electrolyte intake, when cirrhosis is present,or during concomitant use of corticosteroids, ACTH, licorice in large amounts, or prolonged use of laxatives. Digitalistherapy may exaggerate metabolic effects of hypokalemia, especially myocardial effects.
Does furosemide affect albumin?
Furosemide binding to albumin may be reduced in elderly patients. Furosemide is predominantly excreted unchanged in the urine. The renal clearance of furosemide after intravenous administration in older healthy male subjects (6070 years of age) is statistically significantly smaller than in younger healthy male subjects (2035 years of age). The initial diuretic effect of furosemide in older subjects is decreased relative to younger subjects. (See PRECAUTIONS: Geriatric Use.)
Does furosemide inhibit sodium?
Investigations into the mode of action of furosemide have utilized micropuncture studies in rats, stop flow experiments in dogs and various clearance studies in both humans and experimental animals. It has been demonstrated that furosemide inhibits primarily the reabsorption of sodium and chloride not only in the proximal and distal tubules but also in the loop of Henle. The high degree of efficacy is largely due to this unique site of action. The action on the distal tubule is independent of any inhibitory effect on carbonic anhydrase and aldosterone.
Why is digoxin dangerous?
Patients taking digoxin are at increased risk of digoxin toxicity because of the potassium-depleting effect of the diuretic.
What causes edema in the heart?
Edema due to heart failure, hepatic impairment, or renal disease.
How much pedi should I take?
Rate: Administer at a rate not to exceed 4 mg/min (for doses >120 mg) in adults to prevent ototoxicity. Pedi: not to exceed 1 mg/kg/min with infusion not exceeding 10 min. Use an infusion pump to ensure accurate dose.
What is the purpose of monitoring BP and pulse?
Monitor BP and pulse before and during administration. Monitor frequency of prescription refills to determine compliance in patients treated for hypertension.
What is the term for mobilization of excess fluid?
Diuresis and subsequent mobilization of excess fluid (edema, pleural effusions).
Does hypokalemia cause digoxin toxicity?
Hypokalemia may ↑ risk of digoxin toxicity and ↑ risk of arrhythmia in patients taking drugs that prolong the QT interval.
Which is preferred over IM route for parenteral administration?
IV route is preferred over IM route for parenteral administration.
Does furosemide cause hearing loss?
Hearing loss in neonates has been associated with the use of furosemide injection
When should parenteral therapy be used?
Pediatric Patients - Parenteral therapy should be used only in patients unable to take oral medication or in emergency situations and should be replaced with oral therapy as soon as practical.
Can furosemide cause PDA?
WARNINGS: Pediatric Use: In premature neonates with respiratory distress syndrome, diuretic treatment with furosemide in the first few weeks of life may increase the risk of persistent patent ductus arteriosus (PDA), possibly through a prostaglandin-E-mediated process.
Is Furosemide a substitute for clinical judgment?
Furosemide (Lasix ® ) The authors make no claims of the accuracy of the information contained herein; and these suggested doses and/or guidelines are not a substitute for clinical judgment.
Can you use a precipitate injection if it is discolored?
Do not use the injection if it is discolored or contains a precipitate.
What is diuretic resistance?
Qualitatively, diuretic resistance can be described as an inadequate rate/quantity of natriuresis despite an adequate diuretic regimen. A major problem in transitioning from a qualitative to a useful quantitative definition is that an adequate diuretic regimen is subjective and varies with the clinical context. Chronic diuretic treatment greatly increases the capacity of the distal nephron to reabsorb delivered sodium chloride (NaCl), leading to the secondary decline in natriuresis (the “braking phenomenon”). This process occurs in every patient given a diuretic agent, as net NaCl excretion returns to equal NaCl intake at steady state; when this occurs despite persistent congestion, these same mechanisms contribute to diuretic resistance.
Why is a Na+ monitoring important?
Because the dose-response curve to loop diuretic agents is logarithmic, substantial increases in dose (i.e., doubling) are usually required for improved diuretic response. Urine Na + monitoring may also be an effective strategy to guide diuretic dosing, although not yet tested in large studies.
How long does it take for a loop diuretic to increase?
For a sufficient dose of loop diuretic agent, urine output should measurably increase within 2 hours. If there is not an adequate response to initial dose, there is no need to wait until the next scheduled dose to increase dosing.
How many steps are involved in the action of diuretics?
Effective diuretic action requires four discrete steps: 1) ingestion and gastrointestinal absorption (if given orally), 2) delivery to the kidney, 3) secretion into the tubule lumen; and 4) binding to the transport protein—each one of these steps is discussed in this review. Initial loop diuretic dosing in patients hospitalized with HF ...
What are the steps of HF?
Effective diuretic action requires four discrete steps: 1) ingestion and gastrointestinal absorption (if given orally), 2) delivery to the kidney, 3) secretion into the tubule lumen; and 4) binding to the transport protein —each one of these steps is discussed in this review.
What is the effect of chronic kidney disease on HF?
Chronic kidney disease (CKD) is a strong predictor of adverse outcome in HF, and CKD impairs the “reserve” available for the kidneys to respond to the insult posed by congestion. In normal circumstances, renal blood flow (RBF) is around 20% of cardiac output and mainly determined by differences in renal arterial and venous pressure.
Can HF patients be treated without a loop diuretic?
Withdrawal of diuretics: Observational data suggest that HF patients who can be managed chronically without a loop diuretic agent generally have a good prognosis. One question that arises clinically, but for which there are very little data, is whether oral diuretic agents can be withdrawn in patients with HF who are clinically stable.
How does furosemide affect kidney function?
Breaking phenomenon and ceiling effect: Normally, when an individual receives furosemide either orally or intravenously, it increases sodium excretion in urine. In a patient with extracellular volume expansion who has never had exposure to furosemide, the first dose of the drug causes significant sodium excretion and diuresis within the first 3 to 6 hours. After that effect of furosemide weans off, the kidney starts retaining sodium and chloride; this is called "post-diuretic sodium retention." It is imperative to repeat the furosemide dose at 6 to 8-hour intervals to avoid post diuretic sodium retention and achieve significant diuresis. When furosemide is prescribed chronically, the patient's weight loss correlates with urine volume. A discrepancy in weight loss and diuresis indicates excessive sodium intake by the patient, which can be detected by 24-hour urine sodium collection.
How much furosemide is equivalent to bumetanide?
In patients with normal renal function, the oral dose equivalence of furosemide relative to other oral diuretics is as follows[7]: 40 mg of furosemide = 20 mg of torsemide = 1 mg of bumetanide.
What are the symptoms of furosemide overdose?
Signs and symptoms of overdose or toxicity include dehydration, reduced blood volume, and electrolyte imbalances. [11]
What is the interprofessional team for hypervolemia?
For symptomatic patients with hypervolemia secondary to any of the following conditions; heart failure, liver cirrhosis, or nephrotic syndrome/chronic kidney disease, patients usually need aggressive diuresis. Hospitalized patients requiring aggressive diuretics need care by an interprofessional team that includes a nurse, laboratory technologists, pharmacists, and physicians .
How long does furosemide stay in your system?
Only 2.3% to 4.1% of furosemide is existent in an unbound form in therapeutic concentrations. The terminal half-life of furos emide is approximately 2 hours, and the total time of therapeutic effect is 6 to 8 hours.
What is furosemide used for?
The Food and Drug Administration (FDA) has approved furosemide to treat conditions with volume overload and edema secondary to congestive heart failure exacerbation, liver failure, or renal failure, including nephrotic syndrome.
What is the best diuretic for liver cirrhosis?
The recommended diuretics are a combination of spironolactone and furosemide, starting at a ratio of 100 mg of spironolactone and 40 mg of furosemide. [5] They are titrated up to the dose of diuretics in an increment of the same ratio until achieving an adequate response to diuretic therapy or reaching a maximum dose of 400 mg of spironolactone plus 160 mg of furosemide.[5] However, in cases of intolerance to diuretics secondary to borderline blood pressure, the diuretics can be started at relatively lower doses of 50 mg of spironolactone with 20 mg of furosemide.
