Is keratoconus noticeable?
Keratoconus is not usually visible to the naked eye until the later stages of the disease. In severe cases, the cone shape is visible to an observer when the patient looks down while the upper lid is lifted. When looking down, the lower lid is no longer shaped like an arc, but bows outward around the pointed cornea.
What does a person with keratoconus see?
In keratoconus, your cornea thins and gradually bulges outward into a cone shape. This can cause blurry, distorted vision. Keratoconus (ker-uh-toe-KOH-nus) occurs when your cornea — the clear, dome-shaped front surface of your eye — thins and gradually bulges outward into a cone shape.
Can you see up close with keratoconus?
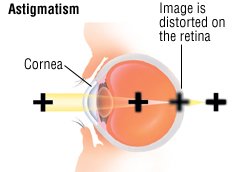
Blurred Objects Near and Far Those with keratoconus often complain of poor vision at all distances even with the best eyeglasses or soft contact lenses. This condition is what's known as “irregular astigmatism” which blurs vision near and far.
How do you suspect keratoconus?
Diagnosis. Diagnosis can be made by slit-lamp examination and observation of central or inferior corneal thinning. Computerized videokeratography is useful in detecting early keratoconus and allows following its progression. Ultrasound pachymetry can also be used to measure the thinnest zone on the cornea.
At what age keratoconus stops?
In any case, progression of the disease is generally considered to have stopped before the age of 40 after approximately 20 years since onset, if any progression had occurred.
Does keratoconus count as a disability?
Is Keratoconus a Disability? Keratoconus eye disease could cause loss of visual acuity that is severe enough to be considered a disability. Keratoconus is not a disability, but vision loss caused by keratoconus may be severe enough to qualify as a disability.
Can a person with keratoconus drive?
But driving — especially in California — is synonymous with freedom, and if your Keratoconus is preventing you from driving, it can alter your life tremendously. Many people with Keratoconus cannot drive safely, especially at night, and so driving with Keratoconus is always on their mind.
Are you legally blind with keratoconus?
A: Keratoconus does not typically cause total blindness. However, as keratoconus progresses it can cause visual impairment including blurred distance vision, distortion, glare, astigmatism, extreme light sensitivity and even vision loss that can be classified as “legal blindness.
Are people with keratoconus allowed to drive?
As most people with keratoconus can have their vision corrected, driving shouldn't be a problem.
How is early keratoconus detected?
Keratoconus early detection (screening) and diagnosis requires an in-deep corneal analysis with different techniques; slip lamp assessment, corneal topography and corneal tomography are the most commonly accepted to detect clinical signs and assess anterior and posterior corneal surface and global corneal pachymetry.
How do you slow down keratoconus?
You may be able to reduce your chance of getting keratoconus by:Protecting your eyes from UV radiation with sunglasses.Making sure your contact lenses fit well.Getting treatment for any kind of eye discomfort (for example, from allergies)Not rubbing your eyes.
How do you fix keratoconus naturally?
But whatever the cause of your own Keratoconus, there is no way to naturally or medically reverse your Keratoconus with diet, exercise, drugs or other therapies.
Can you still drive with keratoconus?
As most people with keratoconus can have their vision corrected, driving shouldn't be a problem.
Can keratoconus patients wear glasses?
For a while, people with a serious eye condition called keratoconus can get by with prescription glasses or contact lenses, although they must ramp up regularly to stronger and stronger lenses.
What causes keratoconus to get worse?
Contact lenses that are not correctly fitted is another reason that Keratoconus gets worse. If the lenses are not accurately fitted on someone with Keratoconus, the lenses can rub against the diseased part of the cornea. The excessive rubbing causes symptoms to worsen by aggravating the already thin cornea.
What is considered severe keratoconus?
Severe keratoconus Dramatic corneal distortion, substantial corneal scarring and thinning. Often there is poor vision with rigid gas permeable contact lenses, substantially reduced contact lens tolerance and usually very difficult to fit an acceptable rigid gas permeable contact lens.
What is keratoconus?
Keratoconus is characterized by the thinning of the cornea and irregularities of the cornea’s surface. The cornea is the clear, outer layer at the front of your eye. The middle layer is the thickest part of the cornea, mostly made up of water and a protein called collagen. Collagen makes the cornea strong and flexible, and helps keep its regular, round shape. This healthy cornea focuses light so you can see clearly. With keratoconus, the cornea thins and bulges into an irregular cone shape, resulting in vision loss.
How is keratoconus diagnosed?
In addition to a complete medical history and eye exam, your eye care professional may perform the following tests to diagnose keratoconus:
What is the purpose of collagen in the eye?
Collagen makes the cornea strong and flexible, and helps keep its regular, round shape. This healthy cornea focuses light so you can see clearly. With keratoconus, the cornea thins and bulges into an irregular cone shape, resulting in vision loss. Keratoconus generally begins at puberty and progresses into the mid-30s.
Why does keratoconus cause collagen loss?
This may be caused by some imbalance between production and destruction of the corneal tissue by the corneal cells.
How long does it take for a corneal transplant to complete?
In a corneal transplant, a donor cornea replaces the patient’s damaged cornea. Corneal transplants are often performed on an outpatient basis and take about an hour to complete. Vision usually remain blurry for about three to six months after the transplant, and medication must be taken to avoid transplant rejection.
How long does it take for a corneal ring to be implanted?
Intacs are implantable, plastic, C-shaped rings that are used to flatten the surface of the cornea, allowing improved vision. They may also allow a better contact lens fit. The procedure takes about 15 minutes.
How to treat progressive keratoconus?
This one-time, in-office procedure involves the application of a vitamin B solution to the eye, which is then activated by ultraviolet light for about 30 minutes or less. The solution causes new collagen bonds to form, recovering and preserving some of the cornea’s strength and shape.
How common is keratoconus?
Keratoconus affects roughly 1 in 2,000 people. It is most common in people aged 10-25. For many patients, it begins in their late teens and progresses until their mid-thirties.
How many people have keratoconus?
The adverse changes to the shape of the cornea can stop at any time, or continue throughout your lifetime. Keratoconus affects roughly 1 in 2,000 people. It is most common in people aged 10-25.
What Causes Keratoconus?
There is no known cause of keratoconus. Researchers have studied both genetic and environmental factors that may lead to the development of this eye condition. However, the research so far has been inconclusive.
What is the corneal shape of a keratoconus?
Keratoconus Treatment Options. Keratoconus FAQs. Your cornea is the rounded front part of your eye. Keratoconus (also known as KC, bulging cornea, or conical cornea) is a progressive eye disease in which your cornea thins, causing it to bulge into a cone-like shape. A cone-shaped cornea deflects light as it enters your eye on the way to the retina ...
What percentage of people with keratoconus have allergies?
Approximately 30 percent of people with keratoconus have some type of allergic disorder. This is not fully understood either. Allergies may trigger eye rubbing, leading to the thinning of the cornea.
What happens when your cornea is thin?
As your cornea thins and bulges, the shape of your eye changes. This is known as irregular astigmatism and causes nearsightedness (myopia). Objects up close are visible, but anything further away is blurry.
How does a keratometer work?
This can be done in several ways. Keratometry is a procedure that measures the anterior curvature of your cornea. The optometrist uses a keratometer to shine a circle of light on your eye. He then measures its reflection to determine the shape of your cornea. The most accurate and common method is corneal topography.
How to diagnose keratoconus?
To diagnose keratoconus, your eye doctor (ophthalmologist or optometrist) will review your medical and family history and conduct an eye exam. He or she may conduct other tests to determine more details regarding the shape of your cornea. Tests to diagnose keratoconus include: Eye refraction. In this test your eye doctor uses special equipment ...
How to treat keratoconus?
Generally, there are two approaches to treating keratoconus: slowing the progression of the disease and improving your vision.
What is the procedure called when the cornea is saturated with riboflavin?
Therapies. Corneal collagen cross-linking. In this procedure, the cornea is saturated with riboflavin eyedrops and treated with ultraviolet light. This causes cross-linking of the cornea, which stiffens the cornea to prevent further shape changes.
What is the procedure to remove scarring from the cornea?
Penetrating keratoplasty. If you have corneal scarring or extreme thinning, you'll likely need a cornea transplant (keratoplasty). Penetrating keratoplasty is a full-cornea transplant. In this procedure, doctors remove a full-thickness portion of your central cornea and replace it with donor tissue.
What is the purpose of computerized corneal mapping?
Special photographic tests, such as corneal tomography and corneal topography, record images to create a detailed shape map of your cornea. Corneal tomography can also measure the thickness of your cornea. Corneal tomography can often detect early signs of keratoconus before the disease is visible by slit-lamp examination.
Where do scleral contact lenses sit?
Instead of resting on the cornea like traditional contact lenses do, scleral lenses sit on the white part of the eye (sclera) and vault over the cornea without touching it. If you're using rigid or scleral contact lenses, make sure to have them fitted by an eye doctor with experience in treating keratoconus.
What is the protective layer between the eye and contact lens?
Scleral contact lenses cover the white part of the eye and arch over the cornea. A protective layer of saline lies between the eye and contact lens. These lenses are a good alternative to surgery for many patients with keratoconus.
What Is Keratoconus?
The cornea is the front part of your eye. A normal cornea is dome-shaped and round.
When does keratoconus start?
While keratoconus starts in late adolescence to early adulthood, it continues to slowly progress up until about age 40 or so. At this time, the progression of the disorder usually stops.
How long does it take for keratoconus to develop?
Keratoconus typically begins in adolescence or early adulthood and progresses slowly over time, usually over a period of 10 to 20 years, the American Optometric Association (AOA) explains.
What is the treatment for keratoconus?
Corneal cross-linking is a minimally invasive, safe, and effective outpatient treatment for keratoconus that can slow the progression of the disorder and improve vision. Corneal cross-linking involves using liquid B2 (riboflavin) and controlled ultraviolet (UV) light to create links in the collagen fibers in your cornea.
What type of contact lens is best for keratoconus?
Gas permeable contact lenses: Rigid gas permeable (RG P) contact lenses can "vault" over the cornea. They may then provide a better fit than soft contact lenses for keratoconus.
What is the last course of action for keratoconus?
A corneal transplant is typically considered the last course of action in treating keratoconus. All other options have usually been explored and exhausted first.
How long does it take for a corneal implant to work?
This is a surgical procedure that has been FDA-approved to treat keratoconus. The procedure is quick, taking 10 minutes or so.
How Is Keratoconus Diagnosed?
If you suspect you have keratoconus, you should consider making an appointment with your eye doctor immediately. Early diagnosis can prevent further damage and vision loss. During the eye exam, your eye doctor will ask you questions about your symptoms and family medical history.
How does keratoconus affect the eye?
The cornea’s job is to refract light that enters the eye. Because of its important job, abnormalities or injuries to the cornea can significantly affect your vision and impair your ability to perform simple tasks like driving, watching TV, or reading a book. Keratoconus can affect one or both eyes, and it can affect each eye differently.
What is the purpose of corneal topography?
Corneal topography: An automated instrument is used to project illuminated patterns onto the cornea to determine its topology (the relationship between objects that share the same surface or border). This exam works best when keratoconus is in its early stages, as it shows any distortions or scarring on the cornea.
What is the procedure to fix keratoconus?
If keratoconus continues to progress after the Intacs are inserted, a corneal transplant may be necessary. Corneal cross-linking: This procedure involves strengthening the corneal tissue to halt the bulging of the eye’s surface. This method was introduced in the United States in 2008, and is also known as CXL.
How long does it take for keratoconus to heal?
The sutures are removed after healing is complete, which is usually three to four weeks. In most cases, eyeglasses and contact lenses are needed after surgery. In any case of keratoconus, frequent check-ups and changes in prescription are needed to achieve good vision and comfort.
What is a KC eye?
Talking to Your Eye Doctor ↓. Keratoconus, often referred to as “KC,” is a slowly progressive, non-inflammatory eye disease that causes the cornea to thin and bul ge out, taking on a cone-shaped appearance. The cornea’s job is to refract light that enters the eye. Because of its important job, abnormalities or injuries to ...
How many people have keratoconus?
Keratoconus can affect one or both eyes, and it can affect each eye differently. One out of every two thousand people may develop keratoconus. In most cases, it begins to develop during adolescence and young adulthood and slowly progresses over the next decade or two before possibly stabilizing.
How long does keratoconus last?
The typical person assumes that the condition will continue to progress forever but this is not the case. When I see a teenager accompanied by their parents I normally have a long and careful discussion, as everyone is stressed and upset. I have examined and followed thousands of people with keratoconus for 35 years. My experience is that for the majority of people, their keratoconus usually stabilises quite well after 25 years of age.
What is keratoconus in Australia?
Keratoconus is a disease of the front surface of the eye that causes progressive deterioration in vision. This typically begins in your teens and progresses during your 20s and 30s. Only 1 person in 2000 of the population is affected in a clinically significant way. This means that in Australia at least 10,000 people need treatment ...
How often do you wear contact lenses for keratoconus?
Often glasses do not work very well and consequently contact lenses are worn during all waking hours, seven days per week.
How old does keratoconus progress?
Having read many articles on keratoconus in the literature and on the internet it is common to read that keratoconus progresses through to forty years of age and beyond. This is rare in my experience when lenses are fitted properly and the affected person and his/her family have careful counselling about the potential damage that is done by eye rubbing.
How many people in Australia have keratoconus?
In a country the size of Australia there are therefore only about 10,000 people that have clinically significant keratoconus.
What happens to the front window of the eye during puberty?
It eventually destabilises and becomes irregular in shape, which causes a deterioration in the vision.
Why is keratoconus steered in an inappropriate direction?
Because there is a lack of experience in managing keratoconus, often a patient with the disease will be steered in an inappropriate direction. Fortunately, you can be different!
How do you know if you have keratoconus?
It is important to realize that while keratoconus may affect as many as 1 out of every 375, that many other more common eye conditions share many of these symptoms. Therefore it is essential for you to have a proper examination so that you receive an accurate diagnosis. Keratoconus cannot be diagnosed only by symptoms alone. Objective clinical signs and measurements require the expertise of your eye doctor.
Who is the best doctor for keratoconus?
The good news is that there are many effective treatments for keratoconus today. Dr. Brian Chou is nationally recognized as one of the top doctors to see for keratoconus.
What is the shape of the cornea?
The shape of the cornea is like a dome, however, in rare cases, it bulges forward like a cone. As a result, the distorted cornea does not adequately focus light, even with glasses and traditional soft contact lenses. This medical disease is known as keratoconus and can progress especially during the teenage years and early twenties.
What is the condition called when you can't see far?
This condition is what’s known as “irregular astigmatism” which blurs vision near and far. 3. Blurry Night Vision.
Can keratoconus be treated with surgery?
For a minority with severe symptoms of keratoconus where all non-surgical treatment has been exhausted, a corneal transplant might help. Corneal transplantation involves using corneal tissue from a deceased donor to replace the diseased corneal tissue.
Can keratoconus be genetic?
Keratoconus has a known genetic link, so if you or anyone in your family receives a keratoconus diagnosis, then you’ll want to schedule regular checkups with your optometrist. Even so, one large study found that only 14% with keratoconus can identify another family member with the condition. In addition to genetic predisposition, some researchers ...
Does rubbing your eyes cause keratoconus?
An unusually large number of patients with keratoconus report a tendency to rub their eyes, which is why your doctor may prescribe medicated drops to extinguish the itch.
.jpg)