Follow these steps to manually submit a claim to Medicare:
- Open the Medicare Claiming dashboard
- Click Accounts at the top of the page
- Click Claiming
- Make sure you are in the " Unclaimed Amount " module
- Click the Tick-box next to the name
- All items being claimed on the selected invoice will be selected
- Click Claim to open the Claim Submission Summary
- Click Claim to send the claim to medicare
Full Answer
How long do you have to submit a medical claim?
You should only need to file a claim in very rare cases. Medicare claims must be filed no later than 12 months (or 1 full calendar year) after the date when the services were provided. If a claim isn't filed within this time limit, Medicare can't pay its share.
What to do if Medicare denies your medical claim?
You can also take other actions to help you accomplish this:
- Reread your plan rules to ensure you are properly following them.
- Gather as much support as you can from providers or other key medical personnel to back up your claim.
- Fill out each form as carefully and exactly as possible. If necessary, ask another person to help you with your claim.
How to check Medicare claims submitted?
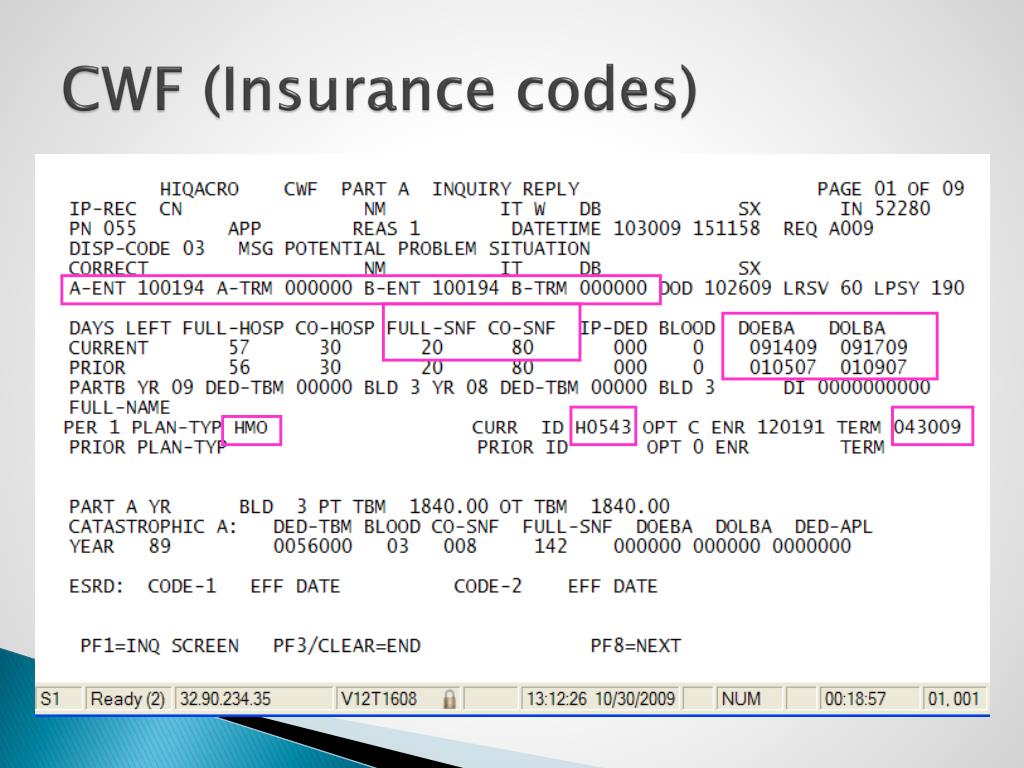
- Providers can enter data via the Interactive Voice Response (IVR) telephone systems operated by the MACs.
- Providers can submit claim status inquiries via the Medicare Administrative Contractors’ provider Internet-based portals.
- Some providers can enter claim status queries via direct data entry screens.
Do I need to file any claims with Medicare?
You usually don’t have to file a Medicare claim. Doctors or hospitals typically file Original Medicare claims for you. Private insurers that administer Medicare Advantage and Part D plans handle those claims. In the rare cases when you have to file a claim, Medicare provides a form to download and mail in.
Can I submit claims directly to Medicare?
Contact your doctor or supplier, and ask them to file a claim. If they don't file a claim, call us at 1-800-MEDICARE (1-800-633-4227). TTY: 1-877-486-2048. Ask for the exact time limit for filing a Medicare claim for the service or supply you got.
What is the first step in submitting a Medicare claim?
The first thing you'll need to do when filing your claim is to fill out the Patient's Request for Medical Payment form. ... The next step in filing your own claim is to get an itemized bill for your medical treatment.More items...•
Can I submit Medicare claim online?
You can submit your claims for Medicare online through your “MyMedicare.gov” account. Or, you can send your paper claim to the address on the Medicare Summary Notice.
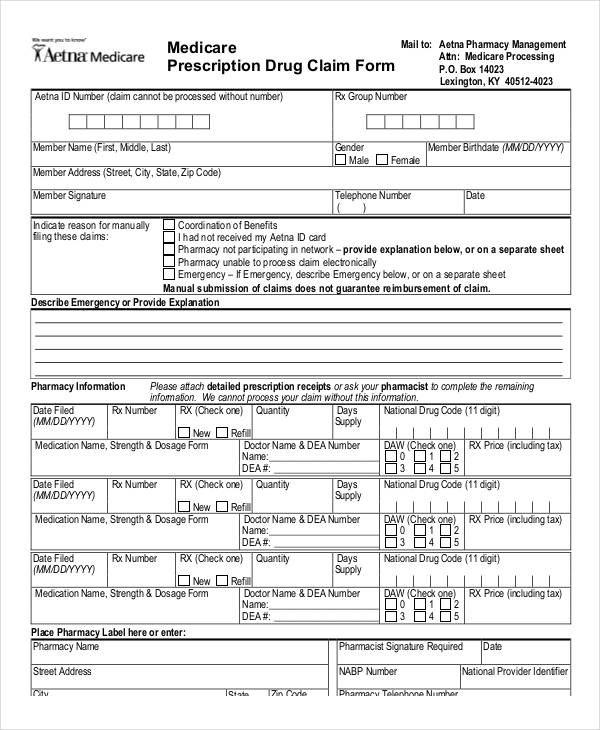
What form is used to send claims to Medicare?
Claim Form (CMS-1500) and Instructions The CMS-1500 claim form is used to submit non-institutional claims for health care services provided by physicians, other providers and suppliers to Medicare.
Does Medicare accept paper claims?
The Administrative Simplification Compliance Act (ASCA) requires that Medicare claims be sent electronically unless certain exceptions are met. Providers meeting an ASCA exception may send their claims to Medicare on a paper claim form.
How long does a Medicare claim take?
If you make a claim at a service centre, you'll get your benefit within 28 days.
How do I submit a claim?
0:152:07How to submit claims online - YouTubeYouTubeStart of suggested clipEnd of suggested clipOnline start by logging on to the plan member site and selecting submit a claim. Click continue toMoreOnline start by logging on to the plan member site and selecting submit a claim. Click continue to go to the submit a claim. Page choose the plan that you want your claim paid.
What are two ways electronic claims can be submitted?
You can submit electronic claims through either self-service or outsourced full-service models. This article is for medical practice owners interested in learning more about electronic claims in medical billing.
How many days will it take to process a Medicare claim that is submitted electronically?
Overview. Your Medicare Part A and B claims are submitted directly to Medicare by your providers (doctors, hospitals, labs, suppliers, etc.). Medicare takes approximately 30 days to process each claim.
How do I fill out a CMS 1500 form for Medicare?
How to fill out a CMS-1500 formThe type of insurance and the insured's ID number.The patient's full name.The patient's date of birth.The insured's full name, if applicable.The patient's address.The patient's relationship to the insured, if applicable.The insured's address, if applicable.Field reserved for NUCC use.More items...•
Who uses CMS 1500 form?
The CMS-1500 form is the standard claim form used by a non-institutional provider or supplier to bill Medicare carriers and durable medical equipment regional carriers (DMERCs) when a provider qualifies for a waiver from the Administrative Simplification Compliance Act (ASCA) requirement for electronic submission of ...
What is the first step in submitting Medicare claims quizlet?
The first step in submitting a Medicare claim is the health provider must submit the covered expenses.
What is the first step in submitting Medicare claims quizlet?
The first step in submitting a Medicare claim is the health provider must submit the covered expenses.
Where do I mail Medicare Part B claims?
GBA Medicare Part B Claims.P.O. Box 6169 Indianapolis, IN 46206.
Who files for Medicare?
Medicare is health insurance for people 65 or older. You're first eligible to sign up for Medicare 3 months before you turn 65. You may be eligible to get Medicare earlier if you have a disability, End-Stage Renal Disease (ESRD), or ALS (also called Lou Gehrig's disease).
How does Medicare reimbursement work?
Medicare pays for 80 percent of your covered expenses. If you have original Medicare you are responsible for the remaining 20 percent by paying deductibles, copayments, and coinsurance. Some people buy supplementary insurance or Medigap through private insurance to help pay for some of the 20 percent.
What is a Medicare claim?
A claim asks Medicare or your insurer to pay for your medical care. Claims are submitted to Medicare after you see a doctor or are treated in a hos...
Who files Medicare claims?
Your healthcare provider will usually file claims for you. You should never have to submit claims for Part A services such as hospital, skilled nur...
When do I need to file Medicare claim?
Original Medicare has both participating and non-participating providers. Participating providers accept Medicare’s reimbursement plus your coinsur...
How long do I have to file a claim?
Original Medicare claims have to be submitted within 12 months of when you received care. Medicare Advantage plans have different time limits for w...
What should I do if my provider doesn’t file my claim?
Before receiving care, ask your provider’s office whether they will submit your bill to Original Medicare. While they aren’t required to do so, som...
Are claim filing requirements different if I have Medicare Advantage or Medigap?
If you have Medicare Advantage, providers in the plan’s network have to bill your insurer for your care. As mentioned above, you may have to submit...
What if I’ve already paid for my care?
You may have already paid in full for your care when you filed your claim. Be sure to note that you’ve paid on your submission, so Medicare or your...
Do I need to file Part D claims?
Medicare Part D plans contract with pharmacies where you can fill your prescriptions. Both preferred and non-preferred pharmacies can bill your Par...
How do I check on my claim to make sure it was processed?
Original Medicare beneficiaries should receive an MSN every three months detailing their recent Medicare claims. Medicare Advantage and Part D enro...
How should I ensure my claims are also filed with Medicaid?
Many Medicare beneficiaries also qualify for Medicaid due to having limited incomes and resources. Medicaid pays for Medicare co-pays, deductibles...
How to file an original Medicare claim?
You can file an Original Medicare claim by sending a Beneficiary Request for Medical Payment form and the provider’s bill or invoice to your regional Medicare Administrative Contractor (Here is a list of these broken down by state). Keep copies of everything you submit. (Original Medicare providers have to give you an advance beneficiary notice ...
Who files Medicare claims?
Your healthcare provider will usually file claims for you. You should never have to submit claims for Part A services such as hospital, skilled nursing facility (SNF) or hospice care. When it comes to outpatient care, some providers will not file claims. This can happen if you have Original Medicare and see a non-participating provider, or if you have Medicare Advantage and visit an out-of-network doctor.
What is a Medicare claim?
A claim asks Medicare or your insurer to pay for your medical care. Claims are submitted to Medicare after you see a doctor or are treated in a hospital. If you have a Medicare Advantage or Part D plan, your insurer will process claims on Medicare’s behalf.
How long do I have to file a claim?
Original Medicare claims have to be submitted within 12 months of when you received care. Medicare Advantage plans have different time limits for when you have to submit claims, and these time limits are shorter than Original Medicare. Contact your Advantage plan to find out its time limit for submitting claims.
What should I do if my provider doesn’t file my claim?
Before receiving care, ask your provider’s office whether they will submit your bill to Original Medicare. While they aren’t required to do so, some non-participating providers will still file your claims with Medicare.
What if I’ve already paid for my care?
You may have already paid in full for your care when you filed your claim. Be sure to note that you’ve paid on your submission, so Medicare or your insurer reimburses you rather than your provider. Keep copies of everything you submit.
Do I need to file Part D claims?
If you have to fill medications at a pharmacy outside your plan’s network because of an emergency, you may be able to receive partial reimbursement by submitting your receipt and supporting documentation to your Part D insurer. Contact your insurer for instructions if you need to file an out-of-network claim.
How to file a claim for Medicare?
How to File a Medicare Claim Yourself. If you need to file your own Medicare claim, you’ll need to fill out a Patient Request for Medical Payment Form, the 1490S. Make sure it’s filed no later than 1 full calendar year after the date of service. Medicare can’t pay its share if the submission doesn’t happen within 12 months.
Who Submits Medicare Claims?
For the most part, your doctor will submit claims to Medicare. But, in some instances, like foreign travel or doctors that don’t accept the coverage, you’ll file the claim. If you receive an Advance Beneficiary Notice of Noncoverage and decide to proceed, it’s best to request your doctor submit the claim to Medicare before billing you.
How Are Medicare Claims Processed?
Then, Medicare will take about 30 days to process the claim. When it comes to Part A services, Medicare will pay the hospital directly.
What Does Medicare Adjustment Mean?
Adjustment claims will be submitted when changing the information on a previous claim is necessary. The change made must impact the processing of the original bill for the change to take place.
What to do if Medicare is denied?
If your Medicare claim is denied, you’ll want to file an appeal.
What is a claim number?
A claim number helps Medicare track your claim. This number is most likely your social security number with a letter after it.
How to check Medicare claim status?
You can easily check the status of Medicare claims by visiting MyMedicare.gov; all you need to do is log into your account. Most claims are sent in within 24 hours of processing.
How long do you have to file a Medicare claim?
You have 1 year to file your Medicare claim after receiving services covered by Medicare as a beneficiary. Your claim may be rejected if you wait longer. Contact a Medicare representative if you have other questions regarding your claim. You can log into your MyMedicare account to check the status of your claim.
How often do you get a Medicare summary notice?
People with original Medicare (parts A and B) may need to file their own claims if their healthcare provider: If you have original Medicare, you’ll receive a Medicare summary notice in the mail every 3 months. This notice will detail your Medicare plans and costs.
What should be included in an itemized bill?
Your itemized bill should include: the date of your medical treatment. the hospital or doctor’s office you went to for treatment. your doctor or healthcare provider’s name and address. a description of each surgical or medical treatment received. an itemized charge for each treatment. your diagnosis.
Do you have to file a claim with Medicare Advantage?
Medicare-approved providers usually send claims directly to Medicare so that you won’t need to. And people with Medicare Advantage (Part C) don’t need to file claims at all because the private insurance companies that offer these plans are paid by Medicare each month.
Do you need to add supporting documents to your claim?
You’ll need to add any supporting documents to your claim after getting an itemized bill for your treatment.
Can I file a Medicare claim online?
You must file your Medicare claim by mail. There isn’t an option to file your Medicare claim online. According to Medicare.gov, you may find the address for where to send your claim in two places: on the second page of the instructions for filing a claim, listed as “How do I file a claim?”.
How to file a claim for Medicare?
If you need to file a claim for Medicare reimbursement, here are the steps you should take: 1 Complete a Medicare form 1490s, “Patient’s Request for Medical Payment.” 2 Attach an itemized bill from the provider including the following information: the date and place of service (doctor’s office or hospital, for example), the description and charge for each service, your diagnosis, and the name and address of the provider who cared for you. 3 Send the form and the itemized bill to your local Medicare contractor. You can find your local contractor using the interactive map on the Centers for Medicare and Medicaid Services website.
When would I need to file a claim for Medicare reimbursement?
There may be times when you are treated by a provider that doesn’t accept Medicare assignment. In this scenario, you may have to file a claim for Medicare reimbursement yourself.
What about Medicare Advantage and Part D plans?
If you have a Part D plan or are enrolled in Medicare Advantage, the steps for submitting claims are a bit different. This is because Part D and Medicare Advantage are actually administered by private insurance companies that contract with Medicare. Each plan has its own rules for paying claims.
What is an advance beneficiary notice of non-coverage?
If you have Original Medicare, your provider should give you an Advance Beneficiary Notice of Non-coverage if Medicare doesn’t normally pay for a service your doctor recommends. You have the option of having the service done and possibly paying for it upfront (your doctor will still bill Medicare even if the claim will likely be denied). You also have the option to refuse service.
What is it called when a provider doesn't accept Medicare?
This is called an excess charge .
What information should be included in an itemized bill?
Attach an itemized bill from the provider including the following information: the date and place of service (doctor’s office or hospital, for example), the description and charge for each service, your diagnosis, and the name and address of the provider who cared for you.
Where to send Medicare bill?
Send the form and the itemized bill to your local Medicare contractor. You can find your local contractor using the interactive map on the Centers for Medicare and Medicaid Services website.
How long do you have to file a Medicare claim?
As a beneficiary, you have one calendar year after receiving medical services to file your Medicare claim. If you file your claim after 12 months has elapsed, it will probably be rejected.
How to view Medicare summary notice?
View your Medicare Summary Notice. If you don’t have a hard copy on hand, you can view an electronic version when you log in to MyMedicare.gov
What is the Medicare website?
The Medicare website contains information sheets detailing the specific requirements for these specialized claim types.
How often do you get a summary notice from Medicare?
Check your Medicare Summary Notice issued every month to see whether you have outstanding claims. In most cases, your health provider will resolve these if you bring them to their attention. However, if they are unable to or simply refuse, you will need to file your own Medicare claim.
What is a 1490s form?
Your completed Patient’s Request for Medical Payment (CMS-1490S) form provides most of the information Medicare needs to process your claim.
Do you need to include supporting documents in Medicare?
This could be for any of the reasons discussed above. In addition, you should include any documents that can support your claim.
Is a diagnosis needed on an itemized bill?
Your specific diagnosis. This may not be necessary on the itemized bill if your Patient’s Request for Medical Payment form contains a thorough illness or injury description
What is Medicare contractor edit?
Medicare contractors perform a series of edits. The initial edits are to determine if the claims in a batch meet the basic requirements of the HIPAA standard. If errors are detected at this level, the entire batch of claims would be rejected for correction and resubmission.
Can a provider purchase software?
Providers can purchase software from a vendor, contract with a billing service or clearinghouse that will provide software or programming support, or use HIPAA compliant free billing software that is supplied by Medicare carriers, DMEMACs and A/B MACs.
How to submit Medicare claims electronically?
How to Submit Claims: Claims may be electronically submitted to a Medicare Administrative Contractor (MAC) from a provider using a computer with software that meets electronic filing requirements as established by the HIPAA claim standard and by meeting CMS requirements contained in the provider enrollment & certification category area of this web site and the EDI Enrollment page in this section of the web site. Providers that bill institutional claims are also permitted to submit claims electronically via direct data entry (DDE) screens.
What chapter is Medicare claim processing manual?
For more information please contact your local MAC or refer to the Medicare Claims Processing Manual (IOM Pub.100-04), Chapter 24.
