noun, plural tho·ra·cen·te·ses [thawr-uh-sen-tee-seez, thohr-]. insertion of a hollow needle or similar instrument into the pleural cavity of the chest in order to drain pleural fluid. Origin of thoracentesis
Thoracentesis
Thoracentesis, also known as thoracocentesis or pleural tap, is an invasive procedure to remove fluid or air from the pleural space for diagnostic or therapeutic purposes. A cannula, or hollow needle, is carefully introduced into the thorax, generally after administration of local anesthesia. The pro…
What should I expect during a thoracentesis?
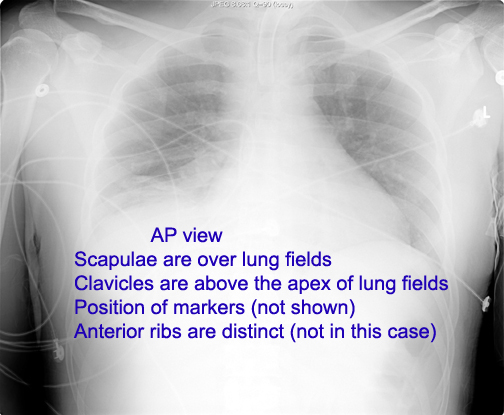
What should I expect during a Thoracentesis procedure? Before your procedure, your physician will most likely order a chest X-ray as well as certain blood tests. The area is then thoroughly cleaned with an antiseptic or special soap and you will receive a local anesthetic to numb the area.
What should I expect after a thoracentesis?
What should I expect after a thoracentesis? A chest x-ray may be needed to check that your lungs were not damaged during the procedure. You may also need any of the following after your procedure: A chest tube may be placed into your chest to drain extra fluid. The chest tube is attached to a container to collect the fluid.
What is the difference between thoracentesis and chest tube?
Thoracocentesis is most frequently performed as a diagnostic procedure to identify the nature of the intrapleural fluid. In contrast to thoracocentesis, chest tube insertion is frequently performed as an emergency procedure. The emergency situations include large pneumothorax or hemopneumothorax and esophageal rupture.
What is the proper position for a thoracentesis?
- Position with good lung down
- Post-procedure vital signs
- Monitor site and dressing Bleeding SubQ Air
- Monitor for infection
- Label & Send Specimens

Is a thoracentesis a major surgery?
A thoracentesis is a minimally invasive procedure that involves a doctor removing fluid or air from the pleural space around your lungs with a needle. It's often performed to improve breathing or help make a diagnosis.
Is a thoracentesis painful?
You will feel a stinging sensation when the local anesthetic is injected. You may feel pain or pressure when the needle is inserted into the pleural space. Tell your provider if you feel short of breath or have chest pain, during or after the procedure.
How long does it take to recover from a thoracentesis?
Recovery time for thoracentesis is short. Your provider may tell you avoid strenuous activities for 48 hours. You can usually take off the bandage after 24 hours. Ask your provider how to manage any symptoms or side effects you have after the procedure, including pain, coughing or fluid leaking from the drainage site.
What fluid is removed in thoracentesis?
Thoracentesis is a procedure used to obtain a sample of fluid from the space around the lungs, called the pleural space. This fluid is called pleural fluid and normally exists only as a thin layer in the area between the lungs and chest wall.
Are you put to sleep for thoracentesis?
You do not need a driver to transport you to or from the procedure unless you will be sedated for the procedure. Most thoracenteses are performed with local numbing medicine, and do not require sedation. If you are taking anti-coagulation medication (blood thinners), please let your pulmonary doctor know.
What is the most common complication from thoracentesis?
Pneumothorax is the most common complication of thoracentesis, with historical incidence rates as high as 19% [19]. Iatrogenic pneumothorax significantly impacts patient outcomes. A recent meta-analysis found that up to one-third of cases require chest tube drainage [2].
What happens to lung after thoracentesis?
The risks of this procedure may include: Air in the space between the lung covering (pleural space) that causes the lung to collapse (pneumothorax) Bleeding. Infection.
What kind of doctor performs thoracentesis?
Thoracentesis is a minimally invasive procedure performed by a radiologist in which fluid that has collected in the pleural space between the lungs and the chest wall is drained through an inserted needle.
Can you go home after thoracentesis?
Once the thoracentesis is done, you will have a chest x-ray. This is to make sure that all the fluid was taken out and that your lungs are working the way they should be. You will be able to go home after your x-ray is done.
How many times can you have thoracentesis?
Depending on the rate of fluid reaccumulation and symptoms, patients are required to undergo thoracentesis from every few days to every 2–3 weeks.
How do you drain mucus from your lungs naturally?
Consider the following steps to help eliminate excess mucus and phlegm:Keep the air moist. ... Drink plenty of fluids. ... Apply a warm, wet washcloth to the face. ... Keep the head elevated. ... Do not suppress a cough. ... Discreetly get rid of phlegm. ... Use a saline nasal spray or rinse. ... Gargle with salt water.More items...
What should I do after thoracentesis?
Take it easy for 48 hours after the procedure. Don't do anything active until your doctor says it's OK. Don't do strenuous activities, such as lifting, until your doctor says it's OK. You will have a small bandage over the puncture site.
Is it painful to have fluid drained from lungs?
The procedure may have been done to help with shortness of breath and pain caused by the fluid buildup, or you may have had this procedure so the doctor could test the fluid to find the cause of the buildup. Your chest may be sore where the doctor put the needle or catheter into your skin (the procedure site).
Do you cough during a thoracentesis?
The health care provider may use ultrasound to find the best spot to insert the needle. You may be asked to hold your breath or breathe out during the procedure. You should not cough, breathe deeply, or move during the test to avoid injury to the lung. Fluid is drawn out with the needle.
What should I do before thoracentesis?
Before a thoracentesis, a chest ultrasound will be done to identify the exact location of the pleural effusion. An ultrasound is preferred because it is more accurate in determining the location of the effusion and the distance from the skin to the fluid collection than a chest X-ray or physical examination.
How long does a thoracentesis last?
When the needle reaches the pleural space between the chest wall and lung, the doctor removes the pleural fluid through a syringe or suction device. Thoracentesis usually takes about 15 minutes. At the end of the procedure, the doctor will remove the needle and apply pressure to stop any bleeding.
Meanings for thoracentesis
It is a medical procedure where a needle in the space between the lungs and the chest wall. It is done to improve breathing. The side effects can be internal bleeding, infection.
Synonyms for thoracentesis
Learn more about the word "thoracentesis" , its origin, alternative forms, and usage from Wiktionary.
What is thoracentesis?
Thoracentesis is a procedure to remove fluid or air from around the lungs. A needle is put through the chest wall into the pleural space. The pleural space is the thin gap between the pleura of the lung and of the inner chest wall. The pleura is a double layer of membranes that surrounds the lungs. Inside the space is a small amount of fluid. The fluid prevents the pleura from rubbing together when you breathe. Excess fluid in the pleural space is called pleural effusion. When this happens, it’s harder to breathe because the lungs can’t inflate fully. This can cause shortness of breath and pain. These symptoms may be worse with physical activity.
What is the name of the medicine that is injected into the area of the swollen ear?
A numbing medicine (local anesthetic) will be injected in the area.
What causes pleural effusion?
Congestive heart failure (CHF), the most common cause of pleural effusion. Systemic lupus erythematosus (SLE) and other autoimmune disease. An area of pus in the pleural space (empyema) Your healthcare provider may have other reasons to advise thoracentesis.
Can you do a thoracentesis on bleeding?
Thoracentesis should not be done in people with certain bleeding conditions.
Can you wear a hospital gown during a thoracentesis?
It depends on your condition and your healthcare provider's methods. In most cases, a thoracentesis will follow this process: You may be asked to remove your clothes. If so, you will be given a hospital gown to wear.
What is a thoracentesis?
Thoracentesis is a procedure that is performed to remove fluid from the thoracic cavity for both diagnostic and/or therapeutic purposes. [1][2]
What is thoracentesis procedure?
Thoracentesis is a procedure that is performed to remove fluid from the thoracic cavity. This can be done for both diagnostic and therapeutic purposes. A potential space exists in the left and right side of the chest cavity between the inner chest wall and lung. In healthy individuals, a trace amount of fluid is found in this space and provides lubrication between the lung parenchyma and musculoskeletal structures of the rib-cage during expansion and recoil. However, excess fluid is pathological. The volume of excessive fluid, the rate of accumulation, the cellular content of the fluid, and the chemical composition of the fluid are all used to guide the management and the differential diagnosis of the underlying etiology. This activity reviews the indications, contraindications, and techniques involved in performing thoracocentesis and highlights the role of the interprofessional team in the care of patients undergoing this procedure.
What position is thoracentesis done in?
Thoracentesis is done in either a supine or sitting position depending on patient comfort, underlying condition, and the clinical indication. [3]
What is therapeutic thoracentesis?
Typically, therapeutic thoracentesis is a large volume (multiple liters of fluid). A small sample of a large volume thoracentesis should be sent for analysis when the etiology of the fluid is unknown or there is a question of a change in the etiology (e.g., new infection, decompensated chronic condition).
Why is ultrasound important in thoracentesis?
If using a sterile probe cover, thoracentesis can be facilitated by ultrasound guidance, improving landmark location and site selection. Ultrasound can also be used to monitor resolution of fluid as thoracentesis is performed or post-procedurally. Ultrasound is also more cost-effective and more accessible if performed at the bedside.
What is the illustration of thoracentesis?
The illustration shows a person having thoracentesis. The person sits upright and leans on a table. Excess fluid from the pleural space is drained into a bag. Contributed by National Heart, Lung and Blood Institute ( PD-US NIH)
When should a thoracentesis be performed?
Thoracentesis should be performed diagnostically whenever the excessive fluid is of unknown etiology. It can be performed therapeutically when the volume of fluid is causing significant clinical symptoms.
Why do doctors do thoracentesis?
Doctors may perform a thoracentesis for one of two reasons: Diagnostic reasons: A thoracentesis can help doctors identify the cause of the pleural effusion. Therapeutic reasons: Too much fluid in the pleural space compresses the lungs, making it difficult for a person to breathe properly. Removing the fluid reduces pressure on the lungs, ...
How long does it take for a thoracentesis to take place?
A thoracentesis usually takes between 10 and 15 minutes, depending on the amount of fluid in the pleural space. The more fluid there is to drain out, the longer the procedure will take.
What is the term for a buildup of fluid in the pleural space?
The medical term for a buildup of fluid in the pleural space is pleural effusion. Some potential causes of pleural effusion include:
What to do after thoracentesis?
A person will receive an X-ray after the thoracentesis to check that the procedure was a success. They will then undergo a period of careful monitoring to ensure that they do not develop complications. A doctor will send fluid samples to a lab to help identify the cause of the pleural effusion.
What is the procedure to remove fluid from the pleural space?
A doctor may suggest a thoracentesis to remove fluid from the pleural space. A thoracentesis is a procedure that involves the use of a needle to remove excess fluid from the pleural space between the lungs and the chest wall. The medical term for a buildup of fluid in the pleural space is pleural effusion.
What is a pleural tap?
It can cause several symptoms, including an inability to breathe properly. A thoracentesis, also called a pleural tap, is a procedure to remove this fluid. Read on to find out how a thoracentesis works, how to prepare for the procedure, and the potential risks and complications.
How to stay awake during thoracentesis?
People usually remain awake for a thoracentesis. A doctor may ask the person to position themselves sitting on the edge of a chair or bed with their head and arms resting on a table. Sitting in this position helps spread out the spaces between the ribs, making it easier for the doctor to insert the needle into the pleural space.
What is therapeutic thoracentesis?
Therapeutic thoracentesis. To relieve symptoms in patients with dyspnea caused by a large pleural effusion. If pleural fluid continues to reaccumulate after several therapeutic thoracenteses, pleurodesis (injection of an irritating substance into the pleural space, which causes obliteration of the space) may help prevent recurrence.
When is thoracentesis not needed?
Diagnostic thoracentesis is usually not needed when the etiology of the pleural fluid is apparent (eg, viral pleurisy, typical heart failure). Selection of laboratory tests typically done on pleural fluid is discussed in pleural effusion.
How to use a thoracentesis needle catheter?
Attach a large-bore (16- to 19-gauge) thoracentesis needle-catheter device to a 3-way stopcock, place a 30- to 50-mL syringe on one port of the stopcock and attach drainage tubing to the other port. Insert the needle along the upper border of the rib while aspirating and advance it into the effusion.
What is the thickness of pleural fluid?
Indicated for almost all patients who have pleural fluid that is new or of uncertain etiology and is ≥ 10 mm in thickness on computed tomography (CT) scan, ultrasonography, or lateral decubitus x-ray (see figure Diagnosis of Pleural Effusion)
How many ml syringes are needed for thoracentesis?
Attach a large-bore (16- to 19-gauge) thoracentesis needle-catheter device to a 3-way stopcock, place a 30- to 50-mL syringe on one port of the stopcock and attach drainage tubing to the other port.
What are the complications of thoracentesis?
Major complications include. Pneumothorax. Bleeding (hemoptysis due to lung puncture) Re-expansion pulmonary edema and/or hypotension ( 1) Hemothorax due to damage to intercostal vessels. Puncture of the spleen or liver. Vasovagal syncope.
How to inject anesthetic into the parietal pleura?
Using a 25-gauge needle, place a wheal of local anesthetic over the insertion point. Switch to a larger (20- or 22-gauge) needle and inject anesthetic progressively deeper until reaching the parietal pleura, which should be infiltrated the most because it is very sensitive.