Healthline.com
1. Flavonoids...
2. Deglycyrrhizinated licorice...
3. Probiotics...
4. Honey...
5. Garlic...
6. Cranberry...
7. Mastic...
Learn More...Medicalnewstoday.com
1. Probiotics...
2. Ginger...
3. Colorful fruits...
4. Plantain bananas...
5. Honey...
6. Turmeric...
7. Chamomile...
8. Garlic...
Learn More...Allremedies.com
1. Cabbage - Carrots...
2. Coconut...
3. Bananas...
4. Honey...
5. Garlic...
6. Cayenne Pepper...
7. Licorice Root...
8. Fenugreek Honey...
Learn More...Trueremedies.com
1. Honey...
2. Garlic...
3. Apple Cider Vinegar...
4. Broccoli...
5. Cabbage...
6. Ginger...
7. Licorice...
8. Mastic...
Learn More...Effectiveremedies.com
1. Cabbage And Carrot...
2. Cayenne Pepper And Warm Water...
3. Bananas With Honey And Milk...
4. Coconut...
5. Fenugreek, Water, Honey, And Milk...
6. Licorice, Water, And Cooked Broken Rice...
7. Raw Honey...
Learn More...How to treat a stage 2 pressure ulcer?
- Patient should be repositioned with consideration to the individual’s level of activity, mobility and ability to independently reposition. ...
- Keep the skin clean and dry.
- Avoid massaging bony prominences.
- Provide adequate intake of protein and calories.
- Maintain current levels of activity, mobility and range of motion.
What are the stages of a pressure ulcer?
Pressure Ulcer Staging Stage 1: Intact skin with non-Stage 2 fi Stage 3: Full thickness tissue loss. Stage 4 Unstageable: Full thickness tissue Suspected Deep Tissue Injury (sDTI): Purple or maroon localized area of discolored intact skin or blood-fi lled blister due to damage of underlying soft tissue from pressure and/or shear.
How do you heal a pressure ulcer?
What you need to do is:
- Boil 2 teaspoons of salt in a cup of water
- Allow it to cool down
- Apply it to the affected areas gently
- Let it dry naturally and use a bandage to cover it
- Do it a few times per day to get faster results
What is the best treatment for buttock ulcer?
hydrocolloid dressings – contain a gel that encourages the growth of new skin cells in the ulcer, while keeping the surrounding healthy skin dry. other dressing types – such as foams, films, hydrofibres/gelling fibres, gels and antimicrobial (antibiotic) dressings may also be used.
What is the best treatment for decubitus ulcers?
Treatments for pressure ulcers (sores) include regularly changing your position, using special mattresses to reduce or relieve pressure, and dressings to help heal the ulcer. Surgery may sometimes be needed.
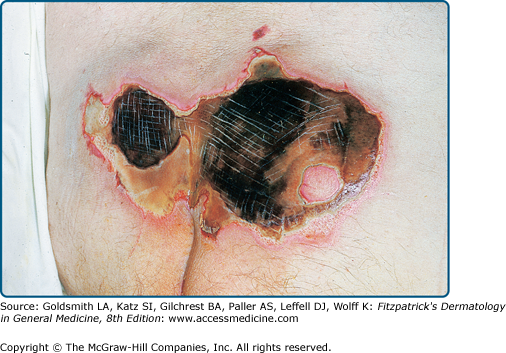
What does a decubitus ulcer look like?
Stages of Decubitus Ulcers Dark complexioned people may have a discoloration that is blue or purple. In some people, the discoloration is white. Stage II: Skin breaks open and the ulcer is shallow with a reddish or pinkish wound bed. There may be tissue death around the wound, or a fluid-filled blister.
Can decubitus ulcers be cured?
Bedsores can develop over hours or days. Most sores heal with treatment, but some never heal completely. You can take steps to help prevent bedsores and help them heal.
What is the best ointment for pressure sores?
Options that are antimicrobial or hydrocolloid, or that contain alginic acid, may be best. Dressings are available for purchase online. Use topical creams: Antibacterial creams can help combat an infection, while barrier creams can protect damaged or vulnerable skin.
Is Vaseline good for bed sores?
You can use any mild ointment, such as antibiotic cream or petroleum jelly (Vaseline). This will prevent the skin from becoming dry and will also protect the sore from dust, dirt, flies and other insects. Be careful not to rub or massage the skin around the pressure sore.
What happens if a bed sore doesn't heal?
Without proper treatment, the loss of blood can cause the skin to die and a wound to form. A stage 4 bedsore is the worst-case scenario: the blood loss is so severe that the wound tunnels down through all layers of the skin and exposes bone.
How do you treat a decubitus ulcer at home?
Cleaning and dressing woundsCleaning. If the affected skin isn't broken, wash it with a gentle cleanser and pat dry. Clean open sores with water or a saltwater (saline) solution each time the dressing is changed.Putting on a bandage. A bandage speeds healing by keeping the wound moist.
Is silver sulfadiazine cream good for bed sores?
It is particularly helpful in preventing burn wounds and small skin grafts from becoming infected. It is also prescribed to help treat infected leg ulcers and pressure sores....About silver sulfadiazine.Type of medicineAn anti-infective skin creamAvailable asCream2 more rows•Feb 10, 2021
Which powder is best for bed sores?
Metronidazole powder (after crushing metronidazole tablets) is economic and effective antibacterial agent. Moreover, it prevents malodor. So, metronidazole powder is widely used for dressing of bedsores.
What is the fastest way to heal a pressure ulcer?
Relieve the pressure on the area.Use special pillows, foam cushions, booties, or mattress pads to reduce the pressure. Some pads are water- or air-filled to help support and cushion the area. ... Change positions often. If you are in a wheelchair, try to change your position every 15 minutes.
How often should a pressure ulcer dressing be changed?
Dressings should be changed regularly and as soon as they become soiled with urine or feces to prevent wound contamination. Each dressing change should be accompanied by concurrent wound reassessment.
What does a Stage 1 pressure ulcer look like?
STAGE 1. Signs: Skin is not broken but is red or discolored or may show changes in hardness or temperature compared to surrounding areas. When you press on it, it stays red and does not lighten or turn white (blanch).
What does a bed sore look like in the beginning?
Bedsores occur in stages: Stage 1 has unbroken, but pink or ashen (in darker skin) discoloration with perhaps slight itch or tenderness. Stage 2 has red, swollen skin with a blister or open areas. Stage 3 has a crater-like ulcer extending deeper into the skin.
What are the four stages of decubitus ulcers?
Stage 1 ulcers have not yet broken through the skin. Stage 2 ulcers have a break in the top two layers of skin. Stage 3 ulcers affect the top two layers of skin, as well as fatty tissue. Stage 4 ulcers are deep wounds that may impact muscle, tendons, ligaments, and bone.
What does it mean when a bed sore turns black?
The skin may turn black in a stage four bed sore, and show signs of infection. The feet are most susceptible to developing eschar, but it can cover any area of the body. The layer of eschar may appear at the bottom or top of the sore. Skin around the eschar may be red, swollen, or tender.
What is a decubitus ulcer?
Decubitus ulcers or pressure sores/bedsores can be a serious problem for patients that are immobile. They are caused by pressure on soft tissue over bony areas of the body. Areas such as the coccyx, heels, hips, and other joints are susceptible to this type of pressure wound. These ulcers can lead to complications such as autonomic dysreflexia, ...
What is the best dressing for ulcers?
This, in turn, makes dressing changes virtually painless. This type of dressing would be a good choice for ulcers that are exuding a lot of liquid. Some alginate dressings on the market are Aquacel, Maxorb, and Kaltostat.
Can an ulcer heal?
Even with the most diligent care, an ulcer can develop. Once these wounds develop, it is important for them to heal as soon as possible to avoid infection and other complications. There are numerous types of dressings that can help with this.
What is a decubitus ulcer?
A decubitus ulcer is also known as a pressure ulcer, pressure sore, or bedsore. It’s an open wound on your skin. Decubitus ulcers often occur on the skin covering bony areas. The most common places for a decubitus ulcer are your: This condition is common among people who:
How to treat ulcers?
Treatment can include: medications. local wound care, including specific dressing recommendations. lifestyle changes, such as repositioning frequently and using special off-loading cushions, as well as making healthy eating choices.
Why does my decubitus hurt?
Prolonged pressure is essentially the main cause of a decubitus ulcer with other factors such as moisture, poor circulation, and poor nutrition contributing. Lying on a certain part of your body for long periods may cause your skin to break down. The areas around the hips, heels, and tailbone are especially vulnerable to pressure sores.
How to remove dead tissue from decubitus?
A process to remove dead or infected tissue called debridement may be recommended by your doctor. Keeping the site clean, dry, and free of irritants is important to promote healing. Off-loading the pressure as well as frequent repositioning is very important when treating a decubitus ulcer.
What does an ulcer look like?
The ulcer is much deeper within the skin. It affects your fat layer and looks like a crater.
Who evaluates pressure ulcers?
Your healthcare provider may refer you to a wound care team of doctors, specialists, and nurses experienced in treating pressure sores. The team may evaluate your ulcer based on several things. These include:
Can you move a person with deep ulcers?
This condition is common among people who: are older. have decreased mobility. spend long periods in bed or a wheelchair. can’t move certain body parts without help. have fragile skin. The condition is treatable, but chronic deep ulcers can be difficult to treat.
What are Bedsores (Decubitus Ulcers)?
Bedsores, also called pressure ulcers or decubitus ulcers, are areas of broken skin that can develop in people who:
How long does it take for a stage IV ulcer to heal?
Stage III and Stage IV ulcers can take longer than six months to heal. Some never heal. Bedsores can be an ongoing problem in chronically ill people who have multiple risk factors, such as incontinence, the inability to move and circulatory problems.
How long does it take for a bed sore to heal?
For example, there is a good chance that a Stage II bedsore will heal within one to six weeks in a relatively healthy older person who eats well and is able to move. Stage III and Stage IV ulcers can take longer than six months to heal. Some never heal. Bedsores can be an ongoing problem in chronically ill people who have multiple risk factors, such as incontinence, the inability to move and circulatory problems.
Why do people with atherosclerosis have bedsores?
This is because the blood flow in their skin is weak, even before pressure is applied to the skin.
How to diagnose a bedsore?
A doctor or nurse can diagnose a bedsore by examining the skin. Testing is usually unnecessary unless there are symptoms of infection.
Can bedsores cause blisters?
Where bedsores occur. At first, there may be only a patch of redness. If this red patch is not protected from additional pressure, the redness can form blisters or open sores (ulcers). In severe cases, damage may extend through the skin and create a deep crater that exposes muscle or bone.
Can you get bedsores from incontinent people?
People who can't control their bladders or bowels (people who are in continent) are at high risk of developing bedsores. Decreased movement — Bedsores are common in people who can't lift themselves off the bed sheets or roll from side to side.
Decubitus meaning and definition
Decubitus is the Latin name for pressure ulcers. Decubitus refers to skin tissue damaged by permanent pressure, shear force, friction, or a combination of these effects. If it’s not prevented and treated normally, skin cells and even bone cells can die during this disease.
What is the cause of decubitus ulcers?
The primary cause of decubitus ulcers is the time that the patient spends in bed. Unfortunately, bedridden patients easily develop decubitus ulcers, especially when they have limited mobility. Elderly and paralyzed patients with pathological weaknesses or the ones with multiple sclerosis or stroke are at particular risk.
Pressure ulcers stages
The development of pressure ulcers has four distinct stages, according to the depth of the wound. The later the treatment begins, the harder it gets to heal bedsores.
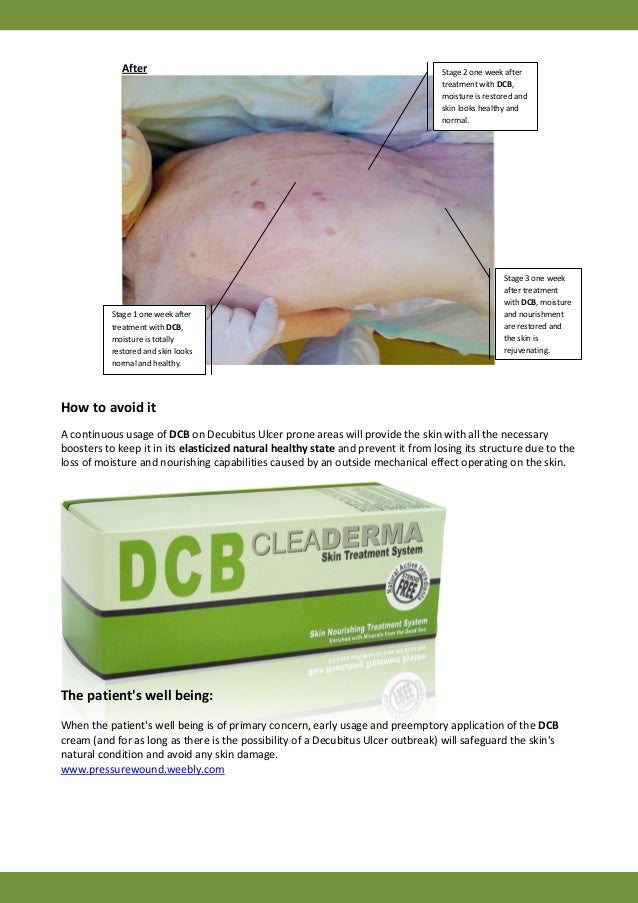
Pressure ulcers treatment: how to treat bedsores?
Prevention is the most important, but if it’s already in one of the above-mentioned stages, proper treatment is inevitable for the patient. The spreading of pressure ulcers has to be prevented.
Decubitus ulcers prevention with dermolex
How to prevent pressure ulcers? Herbs can play a complementary role in the prevention and treatment of bedsores. Our dermolex gel includes herbs like aloe vera, echinacea purpurea, or menthol.
How to treat pressure ulcers?
Treating pressure ulcers involves reducing pressure on the affected skin, caring for wounds, controlling pain, preventing infection and maintaining good nutrition.
What can a social worker do for a child with pressure ulcers?
Parents or caregivers of children with pressure ulcers can talk with a child life specialist for help in coping with stressful health situations.
What to do if a bedsore doesn't heal?
One method of surgical repair is to use a pad of your muscle, skin or other tissue to cover the wound and cushion the affected bone (flap surgery).
What is the best way to heal a wound?
A bandage speeds healing by keeping the wound moist. It also creates a barrier against infection and keeps skin around it dry. Bandage choices include films, gauzes, gels, foams and treated coverings. You might need a combination of dressings.
How to treat bedsore?
The first step in treating a bedsore is reducing the pressure and friction that caused it. Strategies include: Repositioning. If you have a bedsore, turn and change your position often. How often you reposition depends on your condition and the quality of the surface you are on. Using support surfaces.
What is the best medication for a wound?
Drugs to control pain. Nonsteroidal anti-inflammatory drugs — such as ibuprofen (Advil, Motrin IB, others) and naproxen sodium (Aleve) — might reduce pain. These can be very helpful before or after repositioning and wound care. Topical pain medications also can be helpful during wound care.
How to heal a wound?
To heal properly, wounds need to be free of damaged, dead or infected tissue. The doctor or nurse may remove damaged tissue (debride) by gently flushing the wound with water or cutting out damaged tissue.
How to tell if a pressure ulcer is forming?
This is a sign that a pressure ulcer may be forming. The skin may be warm or cool, firm or soft. Stage II: The skin blisters or forms an open sore. The area around the sore may be red and irritated. Stage III: The skin now develops an open, sunken hole called a crater. The tissue below the skin is damaged.
What is stage IV pressure ulcer?
Stage IV: The pressure ulcer has become so deep that there is damage to the muscle and bone, and sometimes to tendons and joints. There are two other types of pressure sores that don't fit into the stages. Sores covered in dead skin that is yellow, tan, green, or brown.
What to do if you have a sore on your back?
Keep the sore covered with a special dressing. This protects against infection and helps keep the sore moist so it can heal. Talk with your provider about what type of dressing to use. Depending on the size and stage of the sore, you may use a film, gauze, gel, foam, or other type of dressing.
How to get rid of pressure sores on skin?
Avoid further injury or friction. Powder your sheets lightly so your skin doesn't rub on them in bed. Avoid slipping or sliding as you move positions. Try to avoid positions that put pressure on your sore. Care for healthy skin by keeping it clean and moisturized. Check your skin for pressure sores every day.
How to check for pressure sores?
Check your skin for pressure sores every day. Ask your caregiver or someone you trust to check areas you can't see. If the pressure sore changes or a new one forms, tell your provider. Take care of your health.
How to treat a pressure sore at home?
Here's how to care for a pressure sore at home. Relieve the pressure on the area. Use special pillows, foam cushions, booties, or mattress pads to reduce the pressure. Some pads are water- or air-filled to help support and cushion the area.
How to clean a stage 2 pressure sore?
Ask your provider what type of moisturizer to use. Stage II pressure sores should be cleaned with a salt water (saline) rinse to remove loose, dead tissue.
What to use to clean a skin ulcer?
If you have a mild skin ulcer, you can clean it with sterile salt water called saline. If your ulcer is severe, a wound-care nurse should do it instead. Turmeric. Turmeric has antimicrobial, antioxidant, and anti-inflammatory properties that may help wound healing.
What is the goal of skin ulcer treatment?
The goal of skin ulcer treatment is to heal the wound, reduce pain, and treat any infection. Your treatment may include:
Why do ulcers develop on the legs?
They develop when blood can’t flow to an injury. Causes of poor blood flow include diabetes, atherosclerosis, pressure, and vein problems. Typically, skin ulcers affect the legs, but they can occur on the feet, hips, and back. Treatment depends on your ulcer and overall health.
What is skin ulcer?
Skin ulcers definition. A skin ulcer is an open sore caused by poor blood flow. Good blood flow is necessary for wound healing. But if you have blood circulation problems, minor injuries can’t heal properly. Over time, an injury can turn into a skin ulcer. If an ulcer becomes infected, it should be treated quickly.
How to tell if you have a skin ulcer?
The outer border might be raised and thick. In the early stages, you’ll notice skin discoloration in the area. It might look red and feel warm. If you have a darker skin tone, it may look shiny or blue.
How many types of skin ulcers are there?
There are four types of skin ulcers. Each one has a different cause and slightly different symptoms. Skin ulcer types include:
Why do ulcers occur on the skin?
Skin ulcers happen when there’s a problem with blood circulation. Causes of poor blood flow include:
How long does it take for a pressure ulcer to heal?
The healing process varies depending on the stage of the pressure ulcer. Stage I & II pressure ulcers and partial thickness wounds heal by tissue regeneration. Stage III & IV pressure ulcers and full thickness wounds heal by scar formation and contraction. Data indicate a 20% reduction in wound size over two weeks is a reliable predictive indicator of healing. (Flanagan 2003)
What is pressure ulcer?
Previously called decubitus or bed sore, a pressure ulcer is the result of damage caused by pressure over time causing an ischemia of underlying structures. Bony prominences are the most common sites and causes. There are many risk factors that contribute to the development of pressure ulcers.
How many people have ulcers in their legs?
Leg ulcers affect more individuals than Pr Us; one in four Americans over the age of 65 will develop a leg ulcer in their lifetime (Wound Ostomy and Continence Nurses Society [WOCN] 2002)
How many stages are there in pressure ulcers?
Pressure ulcers are classified by stages as defined by the National Pressure Ulcer Advisory Panel (NPUAP). Originally there were four stages (I-IV) but in February 2007 these stages were revised and two more categories were added, deep tissue injury and unstageable. Pressure Ulcer Staging.
What is wound management?
Wound management involves a comprehensive care plan with consideration of all factors contributing to and affecting the wound and the patient. No single discipline can meet all the needs of a patient with a wound. The best outcomes are generated by dedicated, well educated personnel from multiple disciplines working together for the common goal of holistic patient care (Gottrup, Nix & Bryant 2007).

What Are Bedsores (Decubitus Ulcers)?
Symptoms
- Bedsores are classified into stages, depending on the severity of skin damage: 1. Stage I (earliest signs of skin damage)— White people or people with pale skin develop a lasting patch of red skin that does not turn white when you press it with your finger. In people with darker skin, the patch may be red, purple or blue and may be more difficult to detect. The skin may be tender or itchy, a…
Diagnosis
- A doctor or nurse can diagnose a bedsore by examining the skin. Testing is usually unnecessary unless there are symptoms of infection. If a person with bedsores develops an infection, a doctor may order tests to find out if the infection has moved into the soft tissues, into bones, into the bloodstream or to another site. Tests may include blood tests, a laboratory examination of tissu…
Expected Duration
- Many factors influence how long a bedsore lasts, including the severity of the sore and the type of treatment, as well as the person's age, overall health, nutrition and ability to move. For example, there is a good chance that a Stage II bedsore will heal within one to six weeks in a relatively healthy older person who eats well and is able to move. Stage III and Stage IV ulcers can take lo…
Prevention
- Bedsores can still form even if a patient is receiving excellent medical care or household care — they are not necessarily a sign of neglected needs. To help prevent bedsores in a person who is confined to a bed or chair, the plan of care includes these strategies: 1. Relieve pressure on vulnerable areas— Change the person's position frequently, when possible every two hours whe…
Treatment
- If you care for someone with bedsores, your doctor or home care nurse may ask you to help with the treatment by following preventive steps that should stop further damage to vulnerable skin and increase the chances of healing. Additional treatments, usually done by health care professionals, depend on the stage of the bedsore. First, areas of unbroken skin near the bedsor…
When to Call A Professional
- If you find a suspicious area of redness or blistering on a person you are caring for, contact the person's nurse or doctor promptly.
Prognosis
- In many cases, the outlook for bedsores is good. Simple bedside treatments can heal most stage II bedsores within a few weeks. If conservative methods fail to heal a stage III or stage IV bedsore, reconstructive surgery often can repair the damaged area.
Further Information
- Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances. Medical Disclaimer