
Steps to Writing Effective Progress Notes
- Get into the habit of writing your notes at the end of every work day.
- Use an online system so the process is faster.
- If you handwrite, use a black pen and ensure your handwriting is legible.
- Sign, time, and date the entry.
- Always check that you are writing in the relevant client’s notes.
- Double-check spelling.
- Avoid acronyms and abbreviations.
- Always check that you are writing in the relevant person's notes. ...
- Use a blue or black pen. ...
- Write legibly. ...
- Note the date of your entry. ...
- Sign your entry. ...
- Avoid blank space between entries. ...
- Make it clear if notes span more than one page. ...
- Errors happen.
How to write better therapy progress notes?
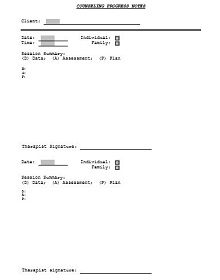
Writing a Progress Note By Section
- Subjective. Give a brief statement on how the patient feels they have been progressing since starting PT (their subjective experience of therapy).
- Summary of Treatment Provided. ...
- Objective: ROM, Strength, Special Tests. ...
- Assessment and Goal Status. ...
- Plan. ...
- Physical Therapy Progress Note Examples. ...
What is an example of a progress note?
The healthcare professionals write the progress note in a different format depending on the clinical situation at hand. One example is using a SOAP note, where the progress note is organized into Subjective, Objective, Assessment, and Plan sections. The progress notes focus on the objectives stated in the nursing care plan.
How to create progress notes?
The Do’s and Don’ts of Creating Progress Notes
- Be concise. ...
- Include adequate details. ...
- Ensure the progress notes are readable to other health care providers. ...
- Ensure the progress notes are legible. ...
- Respect the privacy of the patient. ...
- Avoid including complaints about staff members. ...
- Note down the responses to and from other health care providers. ...
Do you write progress notes daily?
When do you write a progress note? Ideally, you would complete a progress note as soon after the service is delivered, or the information is learned, as possible. Best practice is no more than five days. CDDPs or Brokerages may have specific policies around expectations on frequency of writing progress notes.
How do you write effective progress notes?
Progress Notes entries must be:Objective - Consider the facts, having in mind how it will affect the Care Plan of the client involved. ... Concise - Use fewer words to convey the message.Relevant - Get to the point quickly.Well written - Sentence structure, spelling, and legible handwriting is important.
What needs to go in a progress note?
Write out a specific plan: The progress note should include the treatment plan, tests, and therapies. The rationale for ordering something or initiating a treatment should be explained. There should be sufficient specific details in the plan.
What is the most recommended format for documenting progress notes?
The SOAP (Subjective, Objective, Assessment, and Plan) note is probably the most popular format of progress note and is used in almost all medical settings.
What is a simple progress note?
In the simplest terms, progress notes are brief, written notes in a patient's treatment record, which are produced by a therapist as a means of documenting aspects of his or her patient's treatment. Progress notes may also be used to document important issues or concerns that are related to the patient's treatment.
How long should a progress note be?
For the sake of your sanity, progress notes should take no longer than five to ten minutes at most. If you're in an agency setting, this is typically the expectation.
What is the purpose of a progress note?
These "progress notes" serve as the repository of medical facts and clinical thinking, and are intended as a concise vehicle of communication about a patient's condition to those who access the health record. They should be readable, easily understood, complete, accurate, and concise.
How do you write a process note?
How to create process documentationStep 1: Define the process and its scope. Decide which process you are going to document. ... Step 2: Organize the steps. ... Step 3: Describe who is involved. ... Step 4: Note down exceptions to the normal process flow. ... Step 5: Add control points. ... Step 6: Review and test the process.
What does SOAP stand for?
Subjective, Objective, Assessment and PlanIntroduction. The Subjective, Objective, Assessment and Plan (SOAP) note is an acronym representing a widely used method of documentation for healthcare providers.
How often should progress notes be recorded?
Ideally, progress notes should be present on every day of the patient's stay. And, in cases where the patient's condition is changing quickly, progress notes may be warranted more frequently than daily. Progress notes usually contain information regarding the "progress" that the patient is making.
What are the different types of progress notes?
Types of Progress NotesSession Notes.Event Notes.Contact Notes.Supervision Notes.Documents.Treatment Summary.
How do you write a quick case note?
1:043:31Productivity Hack for Writing Case Notes (Best Secret Revealed!)YouTubeStart of suggested clipEnd of suggested clipThe Pomodoro method is a specific strategy for being really productive. For long periods of timeMoreThe Pomodoro method is a specific strategy for being really productive. For long periods of time when you have something that needs to get done. What you do is set a timer for 25 minutes.
What is the difference between a SOAP note and a progress note?
A SOAP note is a progress note that contains specific information in a specific format that allows the reader to gather information about each aspect of the session.
What are the parts of a SOAP note?
The 4 headings of a SOAP note are Subjective, Objective, Assessment and Plan.
What are progress notes in a medical record?
Progress Note. Description. Represents a patient's interval status during a hospitalization, outpatient visit, treatment with a post-acute care provider, or other healthcare encounter.
How do you write patient progress notes in nursing?
How to Write Nursing Progress Notes: A Cheat SheetDate and time.Patient's name.Nurse's name.Clinical assessment, e.g. vital signs, pain levels, test results.Details of any incidents.Changes in behaviour, well-being or emotional state.Changes in the care provided.Instructions for further care.
What goes in objective content in therapy notes?
Objective Content This is the section to document that which can be seen, heard, smelled, counted, or measured. You can document observations such as the mood and affect of the client here as well.
What are the three main types of progress notes?
There are a lot of different formal approaches to taking progress notes, but the three main types are SOAP notes, BIRP notes, and DAP notes: 1. SOAP notes: SOAP notes are the most common type, containing four separate types of information in four distinct rows: S = Subjective information, such as quotes from the client, ...
How to make notes easy to review?
To make notes extra easy to review, challenge yourself to write a one-sentence summary of the session as the first note each time. That way, you’ll have an easy way to remember the broad strokes if you don’t have a lot of time to review their notes before their next session.
What is process notes?
Process notes are sometimes also referred to as psychotherapy notes—they’re the notes you take during or after a session. They tend to be more freeform notes about the session and your impressions of the client’s statements and demeanour. Since these notes often contain highly sensitive information, HIPAA grants them special protection. Unlike progress notes, you’re not legally obligated to release these notes to your client by federal law—although some states may require you to share them if the client asks for them.
How to make note taking more efficient?
One way group therapists make note-taking more efficient is to write a generalized note about the group interaction (with all names in initials), including group interventions planned. Then, you can include this note in each group member’s progress notes.
Why is it important to take notes in therapy?
Good notes improve your ability to recall details between sessions, and avoid repeating past interventions that didn’t work. Bringing details of past sessions into the therapy room also helps you establish trust and rapport with your new clients , as evidence that you’re really listening.
Why is my client frustrated with my ability to write by hand?
S: Client expressed frustration at compromised ability to write by hand due to cerebral palsy. Said, “I feel like I can do more than people give me credit for.” Client is eager to learn new skills and improve motor functions.
When to write therapy notes?
Writing Efficient Therapy Notes. Some therapists write notes during or right after each session, while others need time to decompress before they tackle client notes. Whenever you decide to do your notes, the key to efficiency is knowing what information is important before you start writing.
What is progress note in therapy?
Therapy progress notes often include information on different areas of functioning that can change as a result of therapeutic intervention, as assessed by Quenza’s Outcome Rating Scale.
Why are progress notes important in therapy?
They’re instrumental in monitoring a patient’s progress, the efficacy of their treatment, and helping professionals understand their patient’s personal experiences. To be helpful and informative, though, progress notes in mental health need ...
What Are Progress Notes in Mental Health?
Progress notes are clinical notes made by psychologists, therapists, clinical counselors, psychiatrists, and other practitioners involved in a patient’s treatment and care.
How to integrate subjective data into therapy progress notes?
Another clever way to integrate subjective data into therapy progress notes is by inviting clients to contribute their own notes from sessions.
What is a psychotherapy note?
Also, unlike progress notes, psychotherapy notes are only written by counselors, therapists, and mental health practitioners who are actively involved in their therapy. This table outlines a few more differences between ...
What is a soap note?
A specific type of progress note, SOAP notes can be shared with any other therapists and care professionals the client may be working with. The four sections of a SOAP method note are: Subjective Data on a patient’s feelings, experiences, or thoughts, such as direct quotes or their observations.
What is a note header?
Note Header: A brief overview of the essential practitioner, patient, and session information, such as when the appointment took place, its duration, and service codes for practice administration.
What is a good progress note?
Writing a good progress note generally requires four things: Check Epic to read about the patient’s medical and surgical history, medications, imaging reports, lab results, vital signs. Read progress notes and orders written since you last saw your patient.
Who can read a patient note?
While your readers will most often include members of your own team (intern, resident, attending) and the other health workers caring for that patient (nurses, physios, social workers, etc.), your note potentially could be read by anyone who takes an interest in that patient. Therefore, it’s a good idea to know how to write a good note.
What should a physical exam begin with?
The physical exam should almost always begin with a review of vital signs.
How many lines should a patient review be?
Start with your subjective review^ of the patient (usually 3-5 lines), including any events or developments since you or your service last saw the patient.
Why are progress notes important?
Progress Notes are written to supplement care documentation so that the quality of care can be continuously improved. They enable staff to re-assess the needs of residents, make changes to their Social Profiles and seek appropriate interventions for Care Plans.
What is progress note?
Progress Notes are brief narrative entries written to record negative and positive events relating to residents. They are also used to record situations regarded as irregular, and residents’ response to lifestyle issues. Progress Notes are written to supplement care documentation so that the quality of care can be continuously improved.
What is objective progress note?
To be effective, Progress Notes must be objective: you must report information that is measurable. You should record situations that you have witnessed or initiated. Subjective documentation is not recommended as it cannot be evaluated. Subjective entries are those which reflect your opinions or assumptions.
Can progress notes be typed?
Progress Notes can be handwritten or typed. If you are lucky enough to work in a facility where Progress Notes are recorded electronically, you will find that Progress Notes are quick to access and easy to record, saving you valuable time.
When should progress notes be read?
Progress Notes should be read at the start of each shift, so staff have a clear understanding of what kind of support will be required.
Why are progress notes important?
Progress notes also provide an important means of communication among staff and reflect the soundness of care delivery in any organization. They are legal documents and should be accurate and plausible and clearly written.
What is progress note in Golden Carers?
Progress notes are an essential part of the documentation required in nursing homes and assisted care facilities. They record changes that impact on the delivery of care.
When to write occurrences?
Write occurrences as soon as possible after the event/situation.
What to do when client falls?
NOTE: In the case of a fall, make client as comfortable as possible (do not lift or help client to stand up), and send somebody to fetch clinical staff. Stay with client until help arrives.
Where to list location in a note?
So when we’re talking about location we want to make sure that we are listing at the top of the note.
Is there such a thing as a perfect note for a therapist?
Every therapist is a work in progress and there is no such thing as a perfect note.
Is progress note a psychotherapy note?
OK, OK, and another consideration is psychotherapy notes versus progress notes. The difference being progress notes are part of the clinical record, right, and are subject to being requested by the client or and, or subpoenaed by the court where psychotherapy notes are considered to be private notes.

Components of A Good Note
- First, write the date and time*.
- On the top line, write the name of your service* (examples: “IM-4”, “Vasc Surg”, “Gyn-Onc”, “Gen Peds”) as well as “MS-3*” or “MS-4” (MS = med student, followed by your year).
- Start with your subjective review^ of the patient (usually 3-5 lines), including any events or developments since you or your service last saw the patient.
- First, write the date and time*.
- On the top line, write the name of your service* (examples: “IM-4”, “Vasc Surg”, “Gyn-Onc”, “Gen Peds”) as well as “MS-3*” or “MS-4” (MS = med student, followed by your year).
- Start with your subjective review^ of the patient (usually 3-5 lines), including any events or developments since you or your service last saw the patient.
- Next comes the physical exam^:
Things Not to Forget
- The date and time and name of your service. Gotta have this.
- The physical exam should almost always begin with a review of vital signs.
- The assessment and plan should begin with a concise summary of the patient’s identity and chief complaint (CC).
- Sign your name.
A Cardinal Sin
- We know, we know – it’s reeeally early in the morning, you’re pressed for time, rounds are about to begin, and your patient keeps on talking. Nevertheless, the worst mistake you can make is to FAIL TO SEE YOUR PATIENT. You may get away with it … but if you don’t, it will be a black mark on your attending’s and resident’s view of you.
A Tip
- If you’re not sure what info to include in your note, look at a note written earlier by an intern or resident. Their notes should clue you in to what aspects of care are pertinent to your patient, and how that information has been recorded before.