
Tips for Writing SOAP note assessment
- Follow the SOAP format
- Keep confidential information out of the assessment
- Your objective has to be specific and realistic
- Assess and give realistic examples
- Take note of your grammar and spelling
- Keep notes on your assessment for future purposes
Full Answer
How to write a SOAP note assessment?
Write an Amazing Occupational Therapy SOAP Note (With Example)
- S – Subjective. This is where therapists will include information about the patient’s demeanor, mood, or any changes in their medical status.
- O – Objective. Under the objective heading, therapists will include the activities they did. ...
- A – Assessment. This is where all that OT schooling comes into play. ...
- P – Plan. ...
- 4 Things To Remember With SOAP Notes. ...
What are the four parts of a SOAP note?
What are the four parts of a SOAP note?
- Vital signs.
- Physical exam findings.
- Laboratory data.
- Imaging results.
- Other diagnostic data.
- Recognition and review of the documentation of other clinicians.
How to write a proper SOAP note?
- The Subjective section of your soap note is about what the patient is experiencing and how they are handling their concerns.
- Some common examples may include chest pain, decreased appetite, and shortness of breath.
- You can also talk to a family member or spouse to get any necessary information.
How to write effective SOAP notes?
Tips for completing SOAP notes:
- Consider how the patient is represented: avoid using words like “good” or “bad” or any other words that suggest moral judgments
- Avoid using tentative language such as “may” or “seems”
- Avoid using absolutes such as “always” and “never”
- Write legibly
- Use language common to the field of mental health and family therapy
What is assessment in a SOAP note?
Assessment. This section documents the synthesis of “subjective” and “objective” evidence to arrive at a diagnosis. This is the assessment of the patient's status through analysis of the problem, possible interaction of the problems, and changes in the status of the problems.
How do you write a SOAP note assessment?
A: Assessment You should include: Your analysis of the subjective and objective information. Clinical and professional knowledge to interpret your client's problems. DSM criteria/Therapeutic Model to identify the issues and treatment.
How do you document assessment?
An assessment report should accomplish the following:Outline the student learning or program outcomes or goals assessed during the assessment cycle timeframe.Identify and describe the specific assessment method(s) and tools used to gather evidence for the outcomes or goals.Identify the specific source(s) of the data.More items...
How do I write a medical assessment?
Assessment & PlanWrite an effective problem statement.Write out a detailed list of problems. From history, physical exam, vitals, labs, radiology, any studies or procedures done, microbiology write out a list of problems or impressions.Combine problems.
What goes in assessment of SOAP note physical therapy?
The American Physical Therapy Association provides general guidance on what information should be included in Physical Therapist SOAP Notes:Self-report of the patient.Details of the specific intervention provided.Equipment used.Changes in patient status.Complications or adverse reactions.More items...•
What is the difference between objective and assessment in SOAP note?
Subjective - What the patient says about the problem / intervention. Objective - The therapists objective observations and treatment interventions. (e.g. ROM, Outcome Measures) Assessment - The therapists analysis of the various components of the assessment.
What are the steps of patient assessment?
emergency call; determining scene safety, taking BSI precautions, noting the mechanism of injury or patient's nature of illness, determining the number of patients, and deciding what, if any additional resources are needed including Advanced Life Support.
What is subjective assessment?
A subjective test is evaluated by giving an opinion. It can be compared with an objective test, which has right or wrong answers and so can be marked objectively. Subjective tests are more challenging and expensive to prepare, administer and evaluate correctly, but they can be more valid.
How do you write a better assessment?
Five tips for writing a good assessmentMake it applicable. Think of the most realistic way of assessing the learner's ability. ... There shouldn't be any surprises. ... Test knowledge of the subject matter, not reading comprehension. ... Don't go above and beyond. ... Give learners the best chance of succeeding.
How do you write a assessment report?
CONTENTS OF AN ASSESSMENT REPORTThe aim of the assessment.The candidate's professional experience.The results of the assessment test.The explanation of the test's results that has been delivered by the candidate.The candidate's possible disagreement with this or that part of the test results or interpretation.More items...
What is an assessment statement?
Assessment Statement means the statement provided by the Validation/Verification Body in accordance with the VCS Program Rules in respect of the Methodology Element; Sample 1Sample 2. Assessment Statement means a statement provided by a Validation/Verification Body in accordance with the VCS Rules; Sample 1.
How do you write a nursing assessment?
How to write a Nursing Assessment Report: A Step by step GuideCollect Information. ... Focused assessment. ... Analyze the patient's information. ... Comment on your sources of information. ... Decide on the patient issues.
How do you present an assessment and plan?
Classically, the assessment and plan are presented together by problem, one problem at a time: present problem A, given your assessment for it, then provide a plan, then move on to problem B and repeat.
What should be included in assessment and plan?
The assessment and plan (abbreviated A/P" or A&P) is a component of an admission note. Assessment includes a discussion of the differential diagnosis and supporting history and exam findings. The plan is typically broken out by problem or system.
What is included in the assessment section of a SOAP note quizlet?
- The assessment section ( or interpretation of the data) is the MOST important section of the progress note. It should inform the reader about the effectiveness of the treatment plan and the progress the patient is making toward goals.
What is Objective assessment?
Edulytic defines objective assessment as “a way of examining in which questions asked has a single correct answer.” Mathematics, geography, science, engineering, and computer science are all subjects that rely heavily on objective exams.
What is Objective assessment in physiotherapy?
The objective assessment is the method by which you discover the clinical signs of the pathology rather than just the symptoms. It is good practice to obtain information from the other side too and comment on whether anything you find (such as swelling) is of long standing or a new sign.
How do you write a good physical therapy assessment?
A great therapy assessment accomplishes two things: It highlights the necessity for skilled therapy....Try following this simple outline for an evaluation assessment:Restate the diagnosis.Remark on the patient's rehab potential.Identify their key impairments.State why skilled PT is necessary.
What is soap subjective Objective assessment Plan?
In modern clinical practice, doctors share medical information primarily via oral presentations and written progress notes, which include histories, physicals and SOAP notes. SOAP—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a structured way.
What does subjective Objective assessment and plan mean?
A process used by clinicians to identify and assess a patient's health status, and the subsequent treatments or course of therapy to improve this status.
What are the 4 parts of soap?
The acronym SOAP stands for Subjective, Objective, Assessment, and Plan.
How do nurse practitioners write SOAP notes?
9:2229:55HOW TO WRITE A SOAP NOTE / Writing Nurse Practitioner Notes ...YouTubeStart of suggested clipEnd of suggested clipQuestion mark um less exercise. Question mark anything else you want to ask them about it write theMoreQuestion mark um less exercise. Question mark anything else you want to ask them about it write the question out there so all you have to write is like yes or no when you're actually in the room.
How do you write an Objective on a SOAP note?
Objective means that it is measurable and observable. In this section, you will report anything you and the client did; scores for screenings, evaluations, and assessments; and anything you observed. The O section is for facts and data. The O section is NOT the place for opinions, connections, interpretations, etc.
How do you write a nursing SOAP note?
0:105:59How to Make SOAP Notes Easy (NCLEX RN Review) - YouTubeYouTubeStart of suggested clipEnd of suggested clipUse the soap note as a documentation method to write out notes in the patient's chart. So stands forMoreUse the soap note as a documentation method to write out notes in the patient's chart. So stands for subjective objective assessment and plan let's take a look at each of the four components.
How important is this method of assessment?
Very important. Especially if you are one working in the medical profession and healthcare profession. As notes are important, as well as the infor...
What should be avoided when writing the Objective part of the note assessment?
Avoid writing not so realistic objectives. As your objectives are also a part of the assessment and looking for the answer to the problem.
Who is the audience for this SOAP assessment?
The people who may be reading your SOAP note assessments are your colleagues, yourself and your superiors. You must always remember to follow the f...
Is there another thing I should watch out for in this method of assessment?
Apart from remembering the format of your notes, you must also remember to take down important information. Which would become useful in different...
Who is reading your soap note?
The people who may be reading your SOAP note assessments are your colleagues, yourself and your superiors. You must always remember to follow the format. Keep in mind that this format is used to make note writing easier as well as easier to find for medical purposes.
What should be avoided when writing the Objective part of the note assessment?
Avoid writing not so realistic objectives. As your objectives are also a part of the assessment and looking for the answer to the problem.
How important is this method of assessment?
Very important. Especially if you are one working in the medical profession and healthcare profession. As notes are important, as well as the information given, it is best to use the SOAP method to make your notes clearer and less confusing.
Why is it important to assess data?
The importance of this method for assessing is that relevant data are easier to find. As well as everything you may need is immediately there. The reason for this method is to make sure that all the data that has been collected are easily given for use. The advantage of using this method is to organize all the information in one location for easier search. Take it like a file folder with all the detailed information. It would be easier to store them in one folder than to store them in different places. It lessens the time for looking and more into finding.
What is the purpose of assessment?
An assessment is a type of examination that allows the assessor to check, analyze, and evaluate a person or an object. The act of assessing something or someone to see if they are still up to the task of handling things. The process of gathering data, interpreting the results and evaluating to check if there is any improvement whatsoever. A systematic basis of examination where the assessor processes the results and information they have gathered for educational purposes.
What does "soap" mean in healthcare?
Have you ever encountered this word SOAP? Did you know that this is merely an abbreviation and the full meaning of the word is different? SOAP actually means Subjective, Objective, Assessment, Plan/Procedure. Now that we know what this abbreviated word means, let’s move on to the general definition of the term. Subjective, Objective, Assessment and Plan is an acronym referring to a method used mostly by healthcare professionals. This document is used by healthcare as it is more structured and in an organized way. Imagine a table where you are going to put the correct information, that is how SOAP Assessment helps them.
Is the soap method good for healthcare?
Rather than having to keep up with writing about a patient’s history, using the SOAP method can help lessen the problem.
What is assessment section?
The assessment section is where you document your thoughts on the salient issues and the diagnosis (or differential diagnosis), which will be based on the information collected in the previous two sections.
What should be included in subjective documentation?
The subjective section of your documentation should include how the patient is currently feeling and how they’ve been since the last review in their own words.
What is the final section of a review?
The final section is the plan, which is where you document how you are going to address or further investigate any issues raised during the review.
When to use quotation marks in a patient response?
You should document the patient’s responses accurately and use quotation marks if you are directly quoting something the patient has said.
Do you need to tell us which article this feedback relates to?
You don't need to tell us which article this feedback relates to, as we automatically capture that information for you .
Can you comment on a diagnosis that is already known?
If the diagnosis is already known and the findings of your assessment remain in keeping with that diagnosis, you can comment on whether the patient is clinically improving or deteriorating:
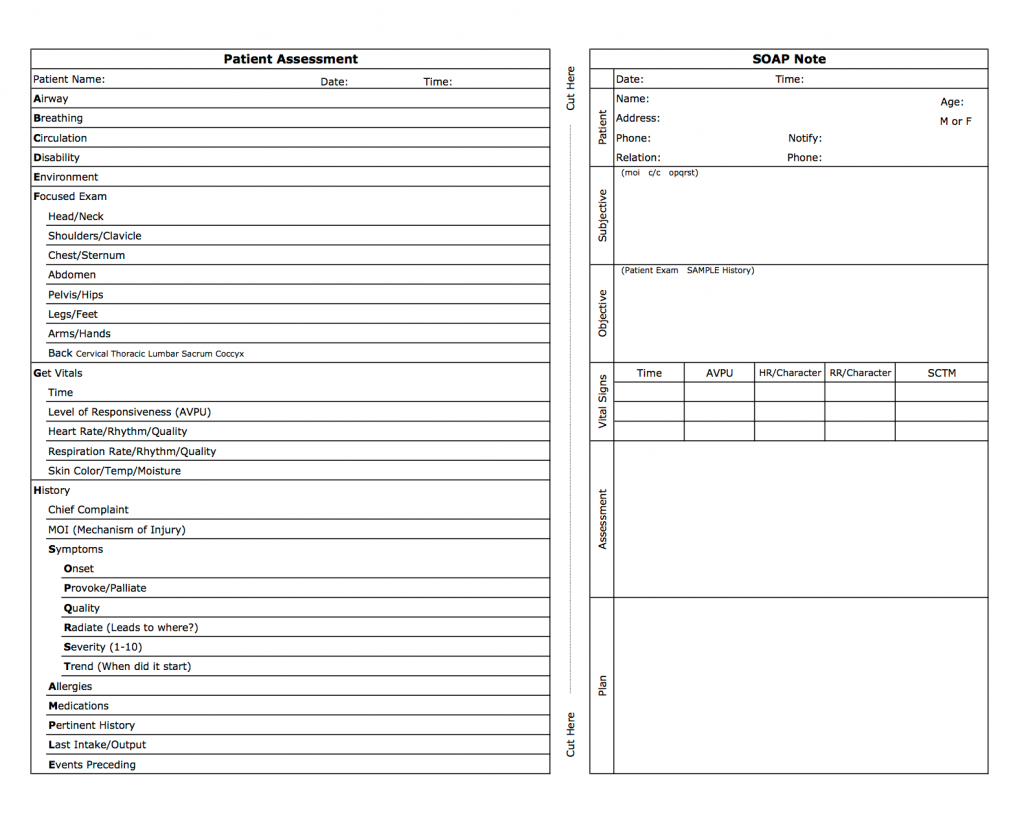
What is a soap note template?
The SOAP Note Template is a documentation method used by medical practitioners to assess a patient's condition. It is commonly used by doctors, nurses, pharmacists, therapists, and other healthcare practitioners to gather and share patient information.
How many parts are in a SOAP note?
SOAP notes have four main parts, designed to help improve evaluations and standardize documentation:
Why do we use soap notes?
SOAP notes are used so staff can write down critical information concerning a patient in a clear, organized, and quick way. SOAP notes, once written, are most commonly found in a patient’s chart or electronic medical records. To see what a SOAP note template looks like, check out (and use!) this example from Process Street: ...
When was the soap note template developed?
Developed by Dr/ Lawrence Weed in the 1960s, the SOAP Note Template methodology records vital patient medical information, to provide evidence of patient contact, and to inform a clinical reasoning process.
Why doesn't a medical soap note contain all the details?
Because it doesn’t contain all the details a medical SOAP would usually have, including the patient’s race, age, gender, and initial information about the chief complaint. This is because those details were most likely already written about in a previous SOAP note.
What is the history of the soap note?
The SOAP note isn’t some made-up mumbo-jumbo; rather, it has a long history rooted in the need to solve complex real-life problems faced by real-life practicing physicians on a day-to-day basis. Here’s a short history lesson for you.
What is subjective section?
The subjective section refers to what the patient tells you. Use the long-text form field below to detail the chronological complaints given by the patient.
What is the purpose of a SOAP note?
SOAP notes are a clinical method used by healthcare professionals to simplify and organize a patient's information. Healthcare practitioners use the SOAP note format to record information in a consistent and structured way.
What is SOAP Note format?
SOAP is an acronym that stands for subjective, objective, assessment, and plan. The elements of a SOAP note are:
How do you write a SOAP note?
What are the four parts of a SOAP note? What should be included in a SOAP note assessment?
SOAP Note Examples
Ms. M. states that she has "been doing ok." Her depressive symptoms have improved slightly; however, she still often feels "low." Ms. M. says she is sleeping "well" and getting "7 hours sleep per night" She expresses concern with my note-taking, causing her to be anxious during the session.
Free SOAP notes templates
There are many free SOAP note templates available for download. These templates are typically in word or PDF format, so you can easily make changes to them.
Tips for Writing SOAP Notes
Here are our top tips on maximizing the value of SOAP notes regardless of your profession or clinical discipline.
Final thoughts
Whether you're an Nurse, Allied health practitioner, therapist, mental health worker, or medical professional, you'll spend less time creating better documentation with SOAP Notes. The best place to start is with free SOAP note software or with a SOAP note template.
What is a therapy soap note?
Therapy SOAP notes follow a distinct structure that allows medical and mental health professionals to organize their progress notes precisely. [1] As standardized documentation guidelines, they help practitioners assess, diagnose, and treat clients using information from their observations and interactions.
Why are soap notes important?
SOAP notes also play a valuable role in Applied Behavior Analysis, by allowing professionals to organize sessions better and communicate with a client’s other medical professionals. Legally, they may also accompany insurance claims to evidence the service being provided. [4]
How does software help with progress notes?
Many therapy software systems help to speed up the documentation of progress notes through in-built templates and diagnostic codes. At the end of the day, however, clinically valuable notes require careful thought and judgment when it comes to their content.
What format are therapy notes in?
Laid out in the S, O, A, P format on therapy notes software, they might look like this:
Why do we write notes immediately after therapy?
This way, a practitioner’s in-session time is spent focused on patient engagement and care; writing notes immediately after helps minimize common mistakes such as forgetting details or recall bias.
What is the purpose of assessment in clinical practice?
Assessment: Practitioners use their clinical reasoning to record information here about a patient’s diagnosis or health status. A detailed Assessment section should integrate “subjective” and “objective” data in a professional interpretation of all the evidence thus far, and
Is ABA SOAP a private document?
It is important to remember that ABA SOAP notes, as psychotherapeutic documents, must be stored privately. They may form part of a client’s overall medical file other therapy notes.
What is a SOAP note?
The SOAP note is a way for healthcare workers to document in a structured and organized way .[1][2][3] The Subjective, Objective, Assessment and Plan (SOAP) note is an acronym representing a widely used method of documentation for healthcare providers.
Why do we use soap notes?
It also provides a cognitive framework for clinical reasoning. The SOAP note helps guide healthcare workers use their clinical reasoning to assess, diagnose, and treat a patient based on the information provided by them.
What is a comprehensive soap note?
A comprehensive SOAP note has to take into account all subjective and objective information, and accurately assess it to create the patient-specific assessment and plan.
What are the headings of a SOAP note?
The 4 headings of a SOAP note are Subjective, Objective, Assessment and Plan. Each heading is described below.
Why is a soap note important?
The advantage of a SOAP note is to organize this information such that it is located in easy to find places.
What is the opening statement for HPI?
The HPI begins with a simple one line opening statement including the patient's age, sex and reason for the visit. Example: 47-year old female presenting with abdominal pain. This is the section where the patient can elaborate on their chief complaint. An acronym often used to organize the HPI is termed “OLDCARTS”:
What is a soap note?
The SOAP note is an essential method of documentation in the medical field. It's imperative that every student learn the basics for writing a SOAP note to become a health care provider like a physician or an Advanced Practice Nurse.
Why Do We Write SOAP Notes?
Healthcare providers need to be fluent in SOAP notes because it provides concise and complete documentation that should describe what you observed, what data you collected, and what you did. Take full credit for your hard work!
What is the general appearance of a patient?
General appearance: The patient is alert, oriented X 4, in no acute distress.
