How do baroreceptors send signals?
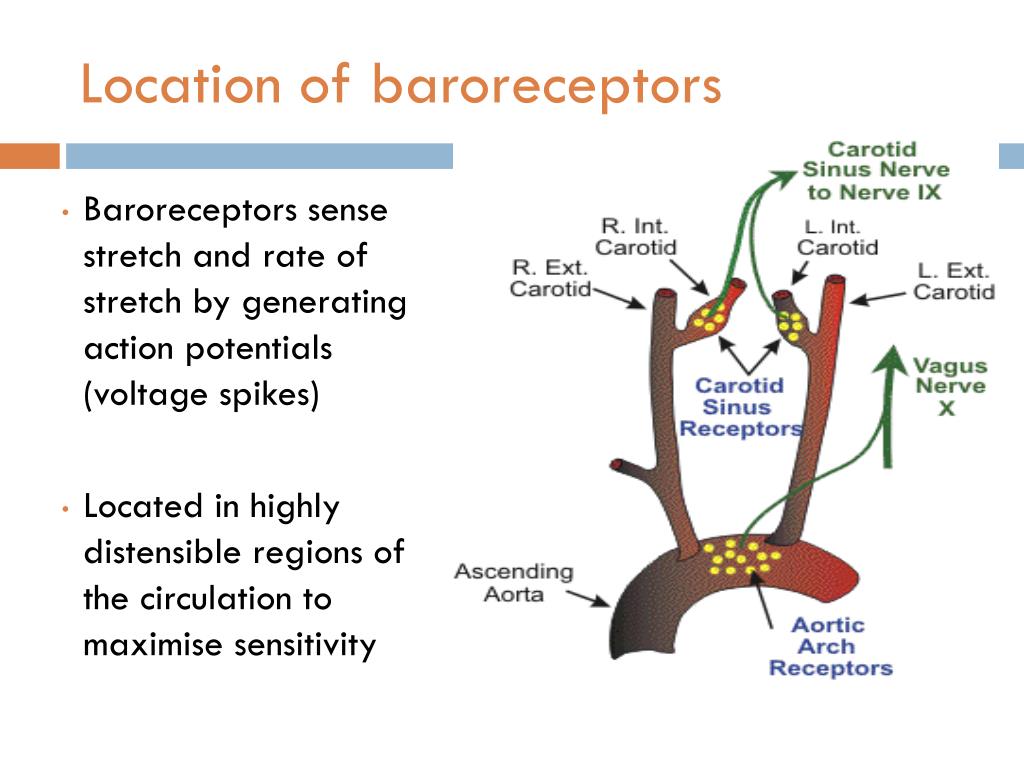
Signals from the carotid baroreceptors are sent via the glossopharyngeal nerve (cranial nerve IX). Signals from the aortic baroreceptors travel through the vagus nerve (cranial nerve X).
How do baroreceptors detect pressure?
Baroreceptors are mechanoreceptors located in blood vessels near the heart that provide the brain with information pertaining to blood volume and pressure, by detecting the level of stretch on vascular walls. As blood volume increases, vessels are stretched and the firing rate of baroreceptors increases.
How do baroreceptors help control heart rate?
The baroreflex or baroreceptor reflex is one of the body's homeostatic mechanisms that helps to maintain blood pressure at nearly constant levels. The baroreflex provides a rapid negative feedback loop in which an elevated blood pressure causes the heart rate to decrease.
How do baroreceptors affect heart rate?
The baroreceptor reflex dampens the short-term fluctuations in blood pressure by feedback modulation of heart rate (HR) and vascular resistance. Impairment of this reflex has been observed in hypertension and heart failure.
What happens when baroreceptor is activated?
Baroreceptor exerts control of mean arterial pressure as a negative feedback loop. Nerve impulses from arterial baroreceptors are tonically active; increases in arterial blood pressure will result in an increased rate of impulse firing.
What happens when baroreceptors are stimulated?
The pulse generator delivers activation energy (voltage range 1-7.5 V) through electrode leads to stimulate the carotid sinus, and then the triggered baroreceptors send signals to the brain, which are interpreted as a rise in blood pressure.
What do baroreceptors do when blood pressure decreases?
Conversely, baroreceptor activity decreases when blood pressure falls, producing a reflex-mediated increase in heart rate and peripheral resistance.
Do baroreceptors increase heart rate?
This causes the vasomotor center to uninhibit sympathetic activity in the heart and blood vessels and decrease vagal tone (parasympathetic influence on the cardiac SA node) causing an increase in heart rate. The baroreflex responds to acute changes in blood pressure.
Do baroreceptors sense blood pressure?
Arterial baroreceptors are sensory neurons that monitor blood pressure for real-time stabilization of cardiovascular output.
How do baroreceptors respond to an increase in blood pressure?
These receptors respond to stretching of the arterial wall so that if arterial pressure suddenly rises, the walls of these vessels passively expand, which increases the firing frequency of action potentials generated by the receptors.
How do baroreceptors know if blood pressure is correct or incorrect?
They respond to changes in blood volume to regulate blood pressure. If the baroreceptors in the aorta detect low blood pressure, it triggers vasoconstriction of systemic blood vessels. This increases the resistance of the circulation to increase blood pressure.
How does the baroreflex regulate blood pressure?
0:033:06Baroreflex Regulation of Blood Pressure, Animation. - YouTubeYouTubeStart of suggested clipEnd of suggested clipBarrow reflex or baroreceptor reflex is one of the mechanisms. The body uses to maintain stableMoreBarrow reflex or baroreceptor reflex is one of the mechanisms. The body uses to maintain stable blood pressure levels or homeostasis baroreflex is a rapid negative feedback loop in which an elevated
What do the baroreceptors sense and how?
“Baro-“ means pressure or stretch, so baroreceptors are special nerve cells or receptors that sense blood pressure, by the way that the walls of the blood vessels stretch. That information is sent from the baroreceptors to the brain to help keep blood pressure balanced.
Do baroreceptors detect high or low blood pressure?
The baroreceptors send signals to the brain and the signals are interpreted as a rise in blood pressure. The brain sends signals to other parts of the body to reduce blood pressure such as the blood vessels, heart and kidneys.
Do baroreceptors sense blood pressure?
Arterial baroreceptors are sensory neurons that monitor blood pressure for real-time stabilization of cardiovascular output.
Are baroreceptors pressure sensors?
Arterial baroreceptors are mechanical sensors that detect blood pressure changes. It has long been suggested that the two arterial baroreceptors, aortic and carotid baroreceptors, have different pressure sensitivities.
What are the stretch receptors that are stimulated by distortion of the arterial wall when pressure changes?
Arterial baroreceptors are stretch receptors that are stimulated by distortion of the arterial wall when pressure changes. The baroreceptors can identify the changes in both the average blood pressure or the rate of change in pressure with each arterial pulse.
How do baroreceptors work?
If blood pressure falls, such as on orthostatic hypotension or in hypovolaemic shock, baroreceptor firing rate decreases and baroreceptor reflexes act to help restore blood pressure by increasing heart rate. Signals from the carotid baroreceptors are sent via the glossopharyngeal nerve ( cranial nerve IX). Signals from the aortic baroreceptors travel through the vagus nerve ( cranial nerve X ). Carotid sinus baroreceptors are responsive to both increases or decreases in arterial pressure, while aortic arch baroreceptors are only responsive to increases in arterial pressure. Arterial baroreceptors inform reflexes about arterial blood pressure but other stretch receptors in the large veins and right atrium convey information about the low pressure parts of the circulatory system.
What are the sensory neuron that are excited by a stretch of the blood vessel?
Baroreceptors are a type of mechanoreceptor sensory neuron that are excited by a stretch of the blood vessel. Thus, increases in the pressure of blood vessel triggers increased action potential generation rates and provides information to the central nervous system. This sensory information is used primarily in autonomic reflexes that in turn influence the heart cardiac output and vascular smooth muscle to influence vascular resistance. Baroreceptors act immediately as part of a negative feedback system called the baroreflex, as soon as there is a change from the usual mean arterial blood pressure, returning the pressure toward a normal level. These reflexes help regulate short-term blood pressure. The solitary nucleus in the medulla oblongata of the brain recognizes changes in the firing rate of action potentials from the baroreceptors , and influences cardiac output and systemic vascular resistance.
What are the two types of blood vessels that are based on the type of blood vessel in which they are located?
Baroreceptors can be divided into two categories based on the type of blood vessel in which they are located: high-pressure arterial baroreceptors and low-pressure baroreceptors (also known as cardiopulmonary or volume receptors ).
What happens when baroreceptors are not working?
When baroreceptors are not working, blood pressure continues to increase, but, within an hour, the blood pressure returns to normal as other blood pressure regulatory systems take over.
Which baroreceptors are responsive to both increases or decreases in arterial pressure?
Carotid sinus baroreceptors are responsive to both increases or decreases in arterial pressure, while aortic arch baroreceptors are only responsive to increases in arterial pressure. Arterial baroreceptors inform reflexes about arterial blood pressure but other stretch receptors in the large veins and right atrium convey information about ...
Where are the baroreceptors located?
Baroreceptors (or archaically, pressoreceptors) are sensors located in the carotid sinus (at the bifurcation of external and internal carotids) and in the aortic arch. They sense the blood pressure and relay the information to the brain, so that a proper blood pressure can be maintained.
How does a traumatic accident affect blood pressure?
On the flip side, let’s say that you’re in a terrible traumatic accident and start losing a lot of blood, causing your blood pressure to fall. The decreased pressure causes the walls of the aortic arch and carotid sinus to become less stretched, and the baroreceptors start firing less frequently. The glossopharyngeal and vagus nerve carry that decreased signal to the cardiovascular centers of the brainstem. To bring the pressure back up to normal, these centers stimulate the sympathetic and inhibit the parasympathetic nervous systems. Specifically, the vasomotor center increases the vasoconstrictive effect of the sympathetic nervous system. In other words, the arterioles narrow, increasing total peripheral arterial resistance, and there’s increased constriction of veins, which returns more blood to the heart rather than allowing it to pool in the periphery. Increased venous return means there’s more preload, and that also increases cardiac output. Meanwhile, remember that the cardiac accelerator center is also stimulated, increasing the sympathetic effect on the heart, and letting the heart work faster and more forcefully, in other words increasing the heart rate and contractility, while the cardiac decelerator center is deactivated, reducing the parasympathetic effects on the heart, which again speeds up the heart rate. Combined, these effects result in an increased cardiac output (CO) and an increase in total peripheral resistance (TPR) which raises the blood pressure (BP) back to normal. In this case, these changes can save your life.
Which nerves carry the increased signal to the cardiovascular centers of the brainstem?
The increased pressure stretches the walls of the aortic arch and the carotid sinus, and the baroreceptors start firing at an increased frequency. The glossopharyngeal and vagus nerve carry that increased signal to the cardiovascular centers of the brainstem.
Where are baroreceptors located?
Alright, baroreceptors are actually groups of nerve endings located within the blood vessel walls. and they can be classified into two types based on their location: the arterial ones and the cardiopulmonary ones. The arterial baroreceptors can be found on the wall of the aortic arch as well as on the wall of the carotid sinus, which is basically a bulge of the internal carotid artery just above its split from the common carotid artery in the neck. In the aortic arch, these nerve endings join up to form the vagus, or tenth (X) cranial nerve, and in the carotid sinus, they form the glossopharyngeal, or ninth (IX) cranial nerve. Both of these cranial nerves travel up towards the brainstem, carrying information about the stretch they sense in the arteries. They synapse at the nucleus tractus solitarius in the medulla oblongata of the brainstem, which then relays the information to the cardiovascular centers. The cardiovascular centers are areas in the lower one-third of the pons and medulla oblongata of the brainstem, responsible for the autonomic or involuntary control of the cardiac and vascular function. They do that by coordinating the sympathetic and parasympathetic branches of the autonomic nervous system. There are two main cardiovascular centers - the first is the vasomotor control center, which controls the diameter of the blood vessels, using the sympathetic nerve fibers to cause vasoconstriction. The second is the cardiac control center, which is further divided into the cardiac accelerator and cardiac decelerator centers. The cardiac accelerator center speeds up the heart rate and increases cardiac contractility through the sympathetic outflow tract, while the cardiac decelerator center slows down the heart rate through the parasympathetic outflow tract. Notice that both the sympathetic and parasympathetic system affect the heart rate, but that only the sympathetic system has an effect on the diameter of the blood vessels and the contractility of the heart muscle. This whole process is known as the baroreceptor reflex, or baroreflex in short, and takes place in seconds to minutes, allowing us to rapidly adjust our blood pressure.
What is the cardiovascular center?
The cardiovascular centers are areas in the lower one-third of the pons and medulla oblongata of the brainstem, responsible for the autonomic or involuntary control of the cardiac and vascular function . They do that by coordinating the sympathetic and parasympathetic branches of the autonomic nervous system.
What is the meaning of baro-?
Tanner Marshall, MS, Evan Debevec-McKenney. “Baro-“ means pressure or stretch, so baroreceptors are special nerve cells or receptors that sense blood pressure, by the way that the walls of the blood vessels stretch. That information is sent from the baroreceptors to the brain to help keep blood pressure balanced.
Which branch of the nervous system controls the diameter of blood vessels?
They do that by coordinating the sympathetic and parasympathetic branches of the autonomic nervous system. There are two main cardiovascular centers - the first is the vasomotor control center, which controls the diameter of the blood vessels, using the sympathetic nerve fibers to cause vasoconstriction.
Does blood pressure decrease with TPR?
Combined, these effects result in a decreased cardiac output (CO). Since blood pressure (BP), roughly equals cardiac output (CO) times total peripheral resistance (TPR), the decrease in cardiac output CO and the decrease in total peripheral resistance (TPR) means that blood pressure (BP) will decrease back down to normal as well.
What is the function of BRs?
Baroreceptors (BRs) are mechanosensitive nerve endings in carotid sinuses and aortic arch that function as arterial blood pressure (BP) sensors.
Why are baroreceptors mechanosensing?
The mechanosensing property of baroreceptors is likely due to the coupling of mechanosensitive ion channels with cytoskeletal membrane and extracellular proteins.
What is a baroreceptor?
Baroreceptors are mechanosensitive afferent nerve endings that are interspersed in the arterial elastic layers. Baroreceptors detect mechanical deformation of the vessel wall (i.e., vascular wall stretch due to changes in intraluminal pressure).
How do baroreceptors help maintain ABP?
Arterial baroreceptors provide a dynamic signal to the brain regarding changes in ABP and elicit reflex responses to maintain ABP within a narrow range. Baroreceptor reflexes are essential for normal cardiovascular homeostasis and stabilize ABP at normal levels on a rapid time frame. Studying the impact of destruction of arterial baroreceptors on cardiovascular regulation has provided useful information on their function. Elimination of baroreceptor signals carried in the aortic depressor nerve and carotid sinus nerve results in a rapid increase in ABP and heart rate, reflecting the marked decrease in baroreceptor afferent signal to brain. Over the course of several days, ABP returns to a normal average level, but the variability around this normal average is markedly increased. A conclusion that can be drawn from such observations is that arterial baroreceptor reflexes are not critical for the maintenance of a normal average level of ABP, but they are essential for stabilizing ABP. These results from baroreceptor-denervated animals have also been used to support the notion that baroreceptor reflexes are not important in the long-term control of blood pressure, but this conclusion has been challenged by more recent studies showing that chronic stimulation of arterial baroreceptor afferents can have a sustained influence on ABP.
What are the two types of baroreceptors?
The presence of two distinct types of baroreceptors is well known. 21 Generally speaking, baroreceptors are classified based on their discharge properties and degree of myelination. 30 One group is formed by neurons with large myelinated afferent fibers. These baroreceptors have lower activation thresholds and fire more rapidly upon stimulation. These are often referred to as type I baroreceptors. The other group is formed by neurons with unmyelinated or small poorly myelinated afferent fibers. These baroreceptors tend to have higher activation thresholds and discharge at lower frequencies. They are referred to as type II baroreceptors. These two receptor types may have a differential role in the regulation of arterial pressure. 31 For example, type II baroreceptors show less resetting than type I baroreceptors and, therefore, may be more important in long-term control of arterial pressure. 32 How differences in mechanotransduction might account for the specific discharge properties of baroreceptor subtypes is poorly understood.
What is the relationship between baroreceptors and PED?
Baroreceptor adaptation and PED contribute to acute resetting of the baroreceptor pressure-activity relationship to higher mean pressures in hypertension. The baroreceptor function curve is shifted in a parallel manner with little or no change in baroreceptor sensitivity (slope), and is usually accompanied by resetting of the arterial BP-HR relation ( Fig. 33.3 ). Central mechanisms may exacerbate or oppose resetting of the baroreflex function curve. While baroreflex resetting compromises the ability to counter the sustained hypertension, it helps preserve the ability to buffer acute fluctuations in BP at the new higher prevailing level of BP.
How do baroreceptors regulate sodium?
In contrast, as vessels contract in response to reduced blood volume, baroreceptors decrease firing. Since sodium insufficiency is often accompanied by changes in blood volume, it was reasoned that baroreceptors were involved in the regulation of sodium appetite. Consistent with this, surgical manipulation of baroreceptors (Thunhorst et al., 1994) or the sinoaortic nerves that communicate their status to the brain ( Thunhorst et al., 1994) alters sodium consumption. For example, Toth et al. (1987) implanted small balloons into the superior vena caval–right atrial junction of rats in order to model volume expansion and determine its impact on sodium appetite. Inflation of these balloons led to stretching of the baroreceptors and signaled volume expansion to the brain. This manipulation also attenuated NaCl intake elicited either by peritoneal dialysis or by administration of DOC, and intakes returned to normal when the balloons were deflated. Similarly, NaCl intake elicited by furosemide is significantly reduced when baroreceptor input is eliminated by sinoaortic denervation ( Thunhorst et al., 1994 ). Collectively, these studies suggest that baroreceptors provide the brain with neural signals pertaining to blood volume that are critical for the normal expression of sodium appetite.
What is the role of the baroreceptor in blood pressure?
The arterial baroreceptor reflex exerts a powerful excitatory influence on parasympathetic activity ( Katona et al., 1970; Kunze, 1972; Kircheim, 1976 ). Baroreceptors are sensory nerve endings located in carotid sinuses, aortic arch, and the juncture of the right carotid and subclavian arteries ( Fig. 7.2 A ). The nerve endings are sensitive to changes in arterial blood pressure. Baroreceptor afferent nerves synapse on neurons in nucleus tractus solitarius (NTS) that ultimately project to nucleus ambiguus and dorsal motor nucleus of the vagus ( McAllen and Spyer, 1978a) ( Fig. 7.2 B). Baroreceptor afferents provide the major excitatory drive to cardiovagal neurons under resting baseline conditions when arterial pressure is normal. Increases in baroreceptor activity during increases in blood pressure reflexively increase parasympathetic activity, thereby reducing HR. Conversely, decreases in arterial pressure reduce baroreceptor activity leading to reflex inhibition of parasympathetic activity and an increase in HR.
How do baroreceptors regulate blood pressure?
One such example of this process is the arterial baroreceptor reflexes, which regulate blood pressure. The loop is activated when vascular distortion is sensed by mechano-sensitive arterial baroreceptors. When blood pressure rises, the splay endings of the arterial baroreceptors are opened, which triggers the firing of baroreceptor afferents. These fibers travel in the IX and X cranial nerves and terminate in the nucleus tractus solitarus in the brainstem. Their activation restrains sympathetic outflow to the vasculature, eliciting vasodilation, and increases parasympathetic activity to the heart, leading to bradycardia. This combination restores blood pressure back to its original level. Similar feedback loops exist to regulate body temperature by controlling sweat output and piloerection.
What is the function of the baroreceptor reflex?
Under normal conditions, arterial pressure is maintained within very narrow limits, and this regulation is accomplished by a powerful negative feedback reflex, the baroreceptor reflex. As blood pressure begins to deviate from its regulated set point, the baroreceptor reflex rapidly compensates for this change, thereby maintaining arterial pressure within a narrow normal range. The afferent component of the baroreceptor reflex is derived from pressure-sensitive receptors associated with the aortic arch and the carotid sinus. These baroreceptor afferent nerves all project into the CNS via the IXth and Xth cranial nerves and terminate in a distinct region of the nucleus tractus solitarius (NTS). These afferents impact the activity of cardiovascular autonomic outflow, and much is known about the central neural pathways that connect the baroreceptor afferent signal projecting to the NTS to the preganglionic sympathetic vasomotor neurons in the intermediolateral (IML) and vagal cardiomotor neurons. The pathway mediating baroreceptor-evoked changes in sympathetic preganglionic neurons involves a projection from the NTS to neurons in the caudal ventrolateral medulla (CVLM). These cells in the CVLM provide inhibitory innervation of RVLM neurons that innervate sympathetic preganglionic neurons. Thus, the RVLM normally is involved both in the tonic maintenance of arterial pressure and its reflexive regulation. NTS baroreceptive neurons excite vagal preganglionic parasympathetic cardiomotor neurons in the nucleus ambiguus and dorsal motor nucleus, and this input is likely monosynaptic.
Why does blood pressure increase?
Blood pressure and heart rate generally increase in response to acute challenges in the laboratory. During performance of tasks such as mental arithmetic, the increase in blood pressure and heart rate is associated with vasodilation in skeletal muscle and reduced blood flow to the kidneys, skin, and viscera (Tidgren & Hjemdahl, 1989). The high heart rate (tachycardia) is a result of sympathetic stimulation coupled with parasympathetic or vagal withdrawal. Blood flow in adipose tissue is increased, and is associated with enhanced lipolysis (Linde, Hjemdahl, Freyschuss, & Juhlin-Dannfelt, 1989). The sensitivity of the cardiac baroreceptor reflex, the mechanism through which increased blood pressure is offset by slower heart rates and vice versa, is inhibited during acute stress. Power spectrum analysis of heart rate and blood pressure signals show changes in spectral density at different frequencies indicative of these autonomic adjustments (Pagani et al., 1991 ). The capacity of the kidneys to excrete sodium and maintain fluid balance may also be impaired, and this may have implications for the development of hypertension ( Light, Koepke, Obrist, & Willis, 1983 ).
How to assess baroreceptor reflex function?
Baroreceptor reflex function is conveniently assessed by recording peripheral autonomic nerve and systemic parameter variations to bol us injections of a vasodilator (e.g., sodium nitroprusside – 0.1mg i.a.) or a vasoconstrictor (e.g., phenylephrine – 0.25mg i.a.).
What is the effector system of the baroreceptor?
Effector Systems of Arterial Baroreceptor Reflexes. The term ‘arterial baroreceptor reflex’ is used to refer to a variety of physiological responses elicited by changes in baroreceptor afferent activity. While the baroreceptor reflex is often used in specific reference to the reflexive change in ABP and heart rate brought about by changing ...
What is the core of the baroreceptor?
ACTH, adrenocorticotropic hormone. At the core of baroreceptor reflexes are the changes in sympathetic outflow, directed at the vasculature and the heart, and in parasympathetic (vagal) outflow, directed at the heart. Changes in baroreceptor afferent activity evoke reflexive changes in autonomic activity to the heart and sympathetic activity ...
What are the two types of baroreceptors?
There are two types of baroreceptors: 1 High-pressure arterial baroreceptors and low-pressure volume receptors which are both stimulated by stretching of the vessel wall. Arterial baroreceptors are located within the carotid sinuses and the aortic arch. 2 Low-pressure volume receptors, or cardiopulmonary receptors, are located within the atria, ventricles, and pulmonary vasculature
What type of mechanoreceptor is responsible for relaying blood pressure?
Baroreceptors are a type of mechanoreceptor allowing for the relay of information derived from blood pressure within the autonomic nervous system.
What is the primary site of termination of baroreceptor afferent fibers?
The primary site of termination of baroreceptor afferent fibers is the nucleus tractus solitarius (NTS). The NTS has been described by many as the primary visceral sensory relay station within the brain. It receives and responds to stimuli from the respiratory, cardiovascular, and gastrointestinal systems.
How long does it take for baroreceptors to reset?
Over a period of days or weeks they will reset to a new value. In people with essential hypertension the baroreceptors behave as if the elevated blood pressure is normal and aim to maintain this high blood pressure. Considering new approaches to treating hypertension is crucial.
What is a baroreceptor?
Introduction. Baroreceptors are a type of mechanoreceptor allowing for the relay of information derived from blood pressure within the autonomic nervous system. They are spray-type nerve endings in the walls of blood vessels and the heart that are stimulated by the absolute level of, and changes in, arterial pressure.
Where are the arterial baroreceptors located?
Arterial baroreceptors are located within the carotid sinuses and the aortic arch.
How effective are baroreceptors?
Intact baroreceptors are extremely effective in preventing rapid changes in blood pressure from moment to moment or hour to hour, but because of their adaptability to prolonged changes of blood pressure (> 2 or 3 days), the system is incapable of long-term regulation of arterial pressure.

Overview
Baroreceptors (or archaically, pressoreceptors) are sensors located in the carotid sinus (at the bifurcation of external and internal carotids) and in the aortic arch. They sense the blood pressure and relay the information to the brain, so that a proper blood pressure can be maintained.
Baroreceptors are a type of mechanoreceptor sensory neuron that are excited by a stretch of the blood vessel. Thus, increases in the pressure of blood vessel triggers increased action potential g…
Arterial baroreceptors
Arterial baroreceptors are stretch receptors that are stimulated by distortion of the arterial wall when pressure changes. The baroreceptors can identify the changes in both the average blood pressure or the rate of change in pressure with each arterial pulse. Action potentials triggered in the baroreceptor ending are then directly conducted to the brainstem where central terminations (synapses) transmit this information to neurons within the solitary nucleus which lies in the medull…
Low-pressure baroreceptors
The low-pressure baroreceptors, are found in large systemic veins, in pulmonary vessels, and in the walls of the right atrium and ventricles of the heart (the atrial volume receptors). The low-pressure baroreceptors are involved with the regulation of blood volume. The blood volume determines the mean pressure throughout the system, in particular in the venous side where most of the blood is held.
Baroreceptor dysfunction
Baroreceptors are integral to the body's function: Pressure changes in the blood vessels would not be detected as quickly in the absence of baroreceptors. When baroreceptors are not working, blood pressure continues to increase, but, within an hour, the blood pressure returns to normal as other blood pressure regulatory systems take over.
Baroreceptors can also become oversensitive in some people (usually the carotid baroreceptor…
See also
• Atrial volume receptors
• Low pressure receptors
External links
• Baroreceptors at the US National Library of Medicine Medical Subject Headings (MeSH)