Tracheitis in some infectious diseases
- Diagnostics. Tracheitis is diagnosed on the basis of a set of methods described for laryngeal diseases. ...
- Treatment. Tracheitis is treated symptomatically and specifically, the treatment corresponds to each type of infection.
- Forecast. Tracheitis has a very varied prognosis, from benign to very serious. ...
How is the diagnosis of bacterial tracheitis confirmed?
Diagnosis of bacterial tracheitis is suspected clinically and can be confirmed by direct laryngoscopy, which reveals purulent secretions and inflammation in the subglottic area with a shaggy, purulent membrane, or by lateral neck x-ray, which reveals subglottic narrowing that may be irregular as opposed to the symmetric tapering typical...
What does bacterial tracheitis stand for?
Bacterial tracheitis, also known as bacterial croup, acute laryngotracheobronchitis, or membranous croup, is a potentially lethal infection of the subglottic trachea. This activity outlines the evaluation and treatment of bacterial tracheitis and explains the role of the interprofessional team in managing patients with this condition. Objectives:
How to treat a tracheitis to an adult?
How to treat a tracheitis to an adult if it is not burdened by a bacterial infection - also the doctor will recommend only that the therapy be comprehensive and give quick positive results. the appointment of expectorants that will dilute thick sputum and remove it from the trachea;
What is the pathophysiology of tracheitis?
Bacterial tracheitis is a bacterial infection of the trachea often preceded by a viral upper respiratory infection. The most common viruses implicated include Influenza A and B (with type A being the most common), respiratory syncytial virus (RSV), parainfluenza virus, measles virus, and enterovirus.

What are the signs and symptoms of tracheitis?
What are the symptoms of bacterial tracheitis?high fever.deep severe cough.difficulty breathing.wheezing.nasal flaring.cyanosis, a blue tinge to their skin.
What are the symptoms of an inflamed trachea?
SymptomsAsthma (wheezing)Bluish tint to skin color, or in the mucous membrane of nose or mouth.Coughing or hoarseness.Coughing up blood.Difficulty breathing.Frequent cases of pneumonia or other upper respiratory infections.Respiratory distress.Shortness of breath.More items...
Does tracheitis go away?
Most children recover without debilitating sequelae with the tracheal mucosa fully healing without permanent damage. Bacterial tracheitis complications may include: Airway obstruction (can lead to death) Toxic shock syndrome if the condition was caused by the bacteria staphylococcus.
What causes tracheitis in adults?
Usually, bacterial tracheitis happens after an upper respiratory infection like the flu, measles, or parainfluenza. Viruses like these can cause damage to the membrane of the trachea, leaving the body sensitive to infection.
How do you cure tracheitis?
Treatment for Tracheitis Antibiotic treatment for bacterial infection is also necessary. Commonly the antibiotics of choice include IV ceftriaxone and IV vancomycin. If cultures come back resistant to these antibiotics, your child's regimen will be changed.
How long can tracheitis last?
Definition. The term acute bronchitis and tracheitis defines a self-limited (1 to 3 weeks) inflammation of the large airways of the lung that extends to the tertiary bronchi (Fig.
What does an irritated trachea feel like?
Pain or a scratchy sensation in the throat. Pain that worsens with swallowing or talking. Difficulty swallowing. Sore, swollen glands in your neck or jaw.
What virus causes tracheitis?
Causes. Bacterial tracheitis is most often caused by the bacteria Staphylococcus aureus. It often follows a viral upper respiratory infection. It affects mostly young children.
What does trachea pain feel like?
In addition to a feeling of fatigue or a general feeling being unwell (malaise), the symptoms of tracheal stenosis typically are: Wheezing, coughing or shortness of breath, including difficulty breathing. A high-pitched squeal coming from your lungs when inhaling.
What does an irritated trachea feel like?
Pain or a scratchy sensation in the throat. Pain that worsens with swallowing or talking. Difficulty swallowing. Sore, swollen glands in your neck or jaw.
What does trachea pain feel like?
In addition to a feeling of fatigue or a general feeling being unwell (malaise), the symptoms of tracheal stenosis typically are: Wheezing, coughing or shortness of breath, including difficulty breathing. A high-pitched squeal coming from your lungs when inhaling.
How do you tell if your trachea is damaged?
What are the symptoms of tracheal disorders?Many patients do not experience any symptoms of tracheal stenosis. ... Wheezing.Stridor (a high-pitched, musical breathing sound)Shortness of breath.Difficulty breathing/respiratory distress.Coughing.Hoarseness.Frequent upper respiratory infections, such as pneumonia.More items...
Why does my trachea feel irritated?
Issues such as the common cold, viral infections, strep throat, or acid reflux can all cause throat irritation. However, throat irritation can sometimes be a sign that a more serious issue is present. A person can often treat throat irritation with a number of home remedies or OTC products.
What is tracheitis in children?
Tracheitis is a bacterial infection of the trachea or windpipe. Tracheitis is an emergency medical condition. Go to the emergency room right away if your child has had a recent upper respiratory infection and suddenly has a high fever, a cough that gets worse, or trouble breathing. Bacterial tracheitis also known as “bacterial croup,” “acute laryngotracheobronchitis,” or “membranous croup,” is due to a secondary bacterial infection of the trachea, resulting in the formation of mucopurulent exudates that may acutely obstruct the upper airway, resulting in a life-threatening condition 1). Bacterial tracheitisis often a secondary bacterial infection preceded by a viral infection affecting children most commonly under age six 2). This may be due to children’s tracheas being smaller and more easily blocked by swelling. Bacterial tracheitis is most often caused by the bacteria Staphylococcus aureus, although reports suggest Moraxella catarrhalis is becoming more common especially in younger children.
What are the effects of bacterial tracheitis?
In bacterial tracheitis, opportunistic bacteria invade damaged tracheal mucosa and stimulate local and systemic inflammatory responses. Local responses cause swelling, thick mucopurulent secretions, ulceration, and mucosal sloughing, which can predispose to subglottic narrowing. Systemic inflammation leading to sepsis is rare but can occur in immunocompromised children.
What is the Gram stain of tracheal secretions?
Microscopic Gram stain analysis of tracheal secretions usually reveals neutrophilia and bacteria identification. Often, bacterial tracheitis is polymicrobial. Infection of the tracheal mucosa causes local inflammation, swelling, thick exudates, pseudomembranes, and necrosis of the larynx, trachea, and mainstem bronchi.
How long does it take to recover from tracheal mucosa infection?
Mean duration of hospitalization is estimated to range from 3 to 12 days 4). One small case series of children with bacterial tracheitis reported a mean duration of hospitalization of 20.8 days 5). The authors speculated that this was due to complications associated with a protracted recovery in several patients 6). Most children recover without debilitating sequelae with the tracheal mucosa fully healing without permanent damage.
How long does it take for a child to recover from tracheitis?
With prompt treatment, the child with tracheitis should recover. Mean duration of hospitalization is estimated to range from 3 to 12 days 16). The mortality rate due to bacterial tracheitis has decreased dramatically with time. In the early twentieth century, the mortality rate was 10% to 40% 17). This has declined slowly with time, and the most recent and largest case series reported no mortality associated with the illness 18). The improvement in mortality rate is likely due to the early recognition and improved treatment of the disorder with aggressive airway clearance techniques and early initiation of broad spectrum antibiotics.
Is bacterial tracheitis a long term complication?
Long-term morbidity associated with bacterial tracheitis is minimal. As treatment in the acute phase of the illness frequently requires insertion of an endotracheal tube into an inflamed airway, the potential for the subsequent development of subglottic stenosis is recognized. This complication, indeed, has been reported in two papers. Gallagher 12) reported that three of 18 patients had subglottic stenosis, and Kasian 13) reported one case in 14 patients.
Can trachea infection be caused by a virus?
Yes. Tracheitis can be caused bacterial and/or viral infection of the trachea or windpipe. Bacterial tracheitis often preceded by a viral upper respiratory infection. Most common viruses implicated include Influenza A and B (with type A being the most common), respiratory syncytial virus (RSV), parainfluenza virus, measles virus, and enterovirus. These viruses cause airway mucosal damage via a local immune response which predisposes the trachea to the seeding of bacterial infections. Staphylococcus aureus has been the most commonly implicated pathogen in tracheitis.
How to diagnose bacterial tracheitis?
The diagnosis of bacterial tracheitis is primarily clinical via a thorough history and physical examination. Children may appear febrile, toxic-appearing, and in respiratory distress. Trial with nebulized epinephrine and glucocorticoids will fail to show improvement in the patient's clinical course. Laboratory investigation with white blood cell count is variable and nonspecific. Leukocytosis, as well as mild leukopenia, are commonly seen. Erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) are also nonspecific but are estimated to be elevated in 68% of patients. Blood cultures are rarely positive; however, they should be obtained if there is suspicion for sepsis or immunocompromised. Radiographic images of the lateral or anteroposterior neck show tracheal narrowing, typical of that seen with croup (steeple sign). Less commonly, irregularity or haziness of the tracheal mucosal wall can also be seen on lateral neck radiographs. This has been referred to as the "candle dripping" sign. The epiglottis should appear normal. The tracheal air column can sometimes be visualized with atypical clouding. Airway stabilization should be a priority before obtaining imaging in patients with severe respiratory symptoms or overt respiratory compromise. Chest radiographs commonly show findings suggestive of pneumonia, reported in roughly 50% of cases. The presence of concomitant pneumonia increases the severity of disease and the probability of endotracheal intubation.
What is tracheitis in children?
Bacterial tracheitis is a bacterial infection of the trachea often preceded by a viral upper respiratory infection. The most common viruses implicated include Influenza A and B (with type A being the most common), respiratory syncytial virus (RSV), parainfluenza virus, measles virus, and enterovirus. These viruses cause airway mucosal damage via a local immune response which predisposes the trachea to the seeding of bacterial infections. Children affected are usually healthy prior to onset, and most will recover with appropriate recognition and treatment. However, at-risk populations, including immunocompromised individuals, are prone to severe sequelae. Implicated bacteria includeStaphylococcus aureus (most common, including MRSA), Streptococcus pneumoniae, Streptococcus pyogenes, Moraxella catarrhalis, Haemophilus influenzae type B, and less commonly, Pseudomonas aeruginosa, Escherichia coli, Klebsiella pneumonia, and anaerobic organisms. The long-term presence of a tracheostomy is another potential predisposing factor, presumed to be a result of the spread from bacterial colonization of the tracheostomy tube. Meticulous tracheostomy care, including pulmonary toilet and scheduled routine changes of the inner cannula daily and the tracheostomy tube monthly, are required to minimize the risk in this specific population. [4][5][6]
How long does it take for a child to recover from a tracheal tube?
The mean duration of hospitalization ranges from three to 12 days. Most children recover without debilitating sequelae, with the tracheal mucosa fully healing without permanent damage. However, subglottic stenosis has been reported secondary to endotracheal intubation with an inflamed airway, and this is an additional reason an uncuffed endotracheal tube is preferred by many pediatric intensivists in this situation. Mortality has been estimated at 2 to 3% of patients due to primary respiratory failure with cardiac arrest, cerebral anoxia, acute respiratory distress syndrome (ARDS), pulmonary edema, pneumothorax, toxic shock syndrome, and septic shock. These incidences are rare, with septic shock seen in 2 to 6%, cardiorespiratory arrest in 2 to 3%, ARDS in 1 to 3%, and the remainder of complications listed in one percent or less of patients. Prevention is aimed at vaccination against viral syndromes (measles and influenza) and pneumococcus, especially in immunocompromised children.
What is the Gram stain of tracheal secretions?
Microscopic Gram stain analysis of tracheal secretions usually reveals neutrophilia and bacteria identification . Often, bacterial tracheitis is polymicrobial. Infection of the tracheal mucosa causes local inflammation, swelling, thick exudates, pseudomembranes, and necrosis of the larynx, trachea, and mainstem bronchi. Biopsy is rarely performed unless there is concern for underlying malignancy or other neoplasm.
What Are Bacterial Tracheitis Symptoms?
Usually, bacterial tracheitis symptoms begin as any other viral upper respiratory infection. This stage typically lasts for one to three days and then gives way to more severe symptoms. However, some children can start to show severe signs of bacterial tracheitis straight away. These symptoms are:
What Causes Bacterial Tracheitis?
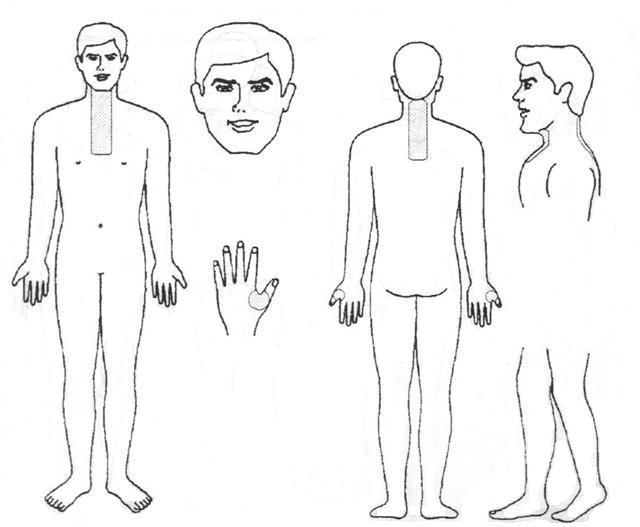
Bacterial tracheitis is an infection of your trachea. The trachea, or windpipe, is found at the top of your airway, and connects your voice box to the large airways, or bronchi, below.
How is tracheitis determined?
Tracheitis and bronchitis, in addition to standard diagnostic methods, is determined using an auscultatory test: the patient takes a deep breath and then a sharp exhalation. With narrowed bronchi, the exhalation is literally “heard” by a typical bronchial whistle.
When does tracheitis occur?
Most often, acute tracheitis occurs in children and the elderly in the spring and autumn periods. Acute banal tracheitis is characterized by hyperemia of the mucous membrane, which is covered by mucus, sometimes forming separate lumps.
What causes acute banal tracheitis?
Primary acute banal tracheitis is most often caused by exposure to colds (general and local cooling, high humidity in the cold season), creating favorable conditions for the activation of conditionally pathogenic local microbiota, as well as increased content of dust, corrosive gases, toxic vapors and all sorts of allergens. Contributing factors may be chronic heart and lung diseases leading to congestion and hyperemia of the upper respiratory tract mucosa, weakening of the nutritional status, low immunity after infectious diseases or HIV infection. In children, exudative diathesis, rickets, dystrophy, as well as poor living conditions can act as contributing factors that cause tracheitis. Most often, acute tracheitis occurs in children and the elderly in the spring and autumn periods.
How to prevent tracheitis during pregnancy?
The only reliable way to prevent tracheitis during pregnancy is prevention , that is, the maximum restriction of contact with patients, sneezing, coughing people who can be found in public places and hospitals.
How long does tracheitis last?
However, with complex intensive treatment, patients with chronic tracheitis recover no later than one month after the onset of the disease .
What is tracheitis inflammation?
Tracheitis is called inflammation in the mucous membrane of the trachea, which can occur in both acute and chronic forms.
How long does it take to recover from tracheitis?
With the usual clinical course and timely started treatment, tracheitis is completed within 1-2 weeks. Under unfavorable conditions, failure to comply with the regimen prescribed by the doctor, untimely treatment of tracheitis and other negative factors, recovery is delayed and the process can turn into a chronic stage.
What is a bacterial tracheitis?
Bacterial tracheitis is bacterial infection of the trachea. Bacterial tracheitis is uncommon and can affect children of any age. Staphylococcus aureus and group A beta-hemolytic streptococci are involved most frequently. Most children have symptoms of viral respiratory infection for 1 to 3 days before the onset of severe symptoms ...
Can bacterial tracheitis be a complication of croup?
Rarely, bacterial tracheitis develops as a complication of viral croup or endotracheal intubation. As in patients with epiglottitis, the child may have marked toxicity and respiratory distress that may progress rapidly and may require intubation. Complications of bacterial tracheitis include hypotension, cardiorespiratory arrest, bronchopneumonia, ...
Can antibiotics be used for tracheitis?
Antibiotics effective against S. aureus and streptococcal species. Treatment of bacterial tracheitis in severe cases is the same as that for epiglottitis ; whenever possible, endotracheal intubation should be done in controlled circumstances by a clinician skilled in managing a pediatric airway.
Why do you need to be close to a doctor for tracheitis?
Tracheitis requires close attention to symptoms and timely treatment in the hospital, because complications of the disease can be severe.
What causes tracheitis in the body?
Most often, the attachment of this pathology causes untimely treatment of the primary disease, as well as penetrating into the body of staphylococci and streptococci. Their activation occurs against a background of weakened immunity. Also tracheitis develops in those people who work in hazardous production and are forced to spend a long time in shops with increased gas contamination and dustiness of the premises.
What is the distraction of thick sputum from the bronchi?
Distraction of thick sputum from the bronchi. Tracheitis is a pathology that lasts for a long time and is difficult, against the background of inflamed tissue of the trachea, its mucosa begins to release a small amount of viscous sputum, which has the consistency of clots. In comparison with bronchitis, the amount of sputum for tracheitis is much less.
What is the atrophic form of tracheitis?
The atrophic form of tracheitis is accompanied by thinning of the tissue, it acquires a shine, becomes crusty, which causes a frequent debilitating cough.
How long does it take to treat tracheitis?
The main step in the therapy of tracheitis should be timely diagnosis. The faster the patient goes to the doctor, the more rapid results can be achieved during therapy. If the pathology is complicated by bleeding and abundant discharge of thick mucus, and even against the background of the infection, treatment can take several weeks and require perseverance and effort.
How long does tracheitis last?
Tracheitis in adults, which manifests itself as a prolonged, painful cough, is becoming more common today. It can last for weeks and even months, having under itself a different etiology - viral, bacterial, allergic. Suffer from this pathology and people living in an unfavorable ecological environment - in conditions of dust, gas contamination and excess of household chemicals in the district.
Is tracheitis the same as bronchitis?
Many sick people confuse the manifestations of tracheitis with bronchitis, although these two pathologies have completely different roots. In bronchitis, the alveoli of the bronchial tree become inflamed, and with tracheitis, the mucous membrane of the tissue lining the trachea.
What is tracheitis?
Some time the inner lining of the trachea in the humans can get inflamed and this condition is called tracheitis. Various bacterial infections can lead to tracheitis; however, tracheitis can also be caused by some other infectious and non-infectious factors. In many cases, these factors affect not only the trachea, but neighboring areas as well.
What are the causes of tracheitis?
There are various causes of tracheitis and infections are by far the most common. The trachea is broad tract that leads from the larynx (voice box) and then divides into the two bronchi, which in turn lead to the lungs. The trachea has C-shaped cartilages which keeps it open. Unlike with other parts of the respiratory tract, especially the bronchi, it cannot widen and narrow to a large degree in response to stimuli. Laryngitis and bronchitis are more common than tracheitis but the infection from the larynx or bronchi can easily spread to the trachea.
How to treat tracehitis?
Bacterial infections on the other hand usually requires antibiotics to eradicate the bacteria. The condition should be monitored carefully as a repeat course of antibiotics may be required in severe cases which do not respond to the initial course. Although antibiotics is the mainstay of treatment for bacteria l tracheitis, cough suppressants may also be prescribed for symptomatic relief.
Why does my trachea get swollen?
Tracheitis affects small children more frequently because their windpipes are smaller in size and shape. As a result of inflammation, the trachea get swollen easily.
How long does it take for tracheitis to appear?
The first symptoms associated with tracheitis appear within a few days after contracting the infection.
What is the purpose of X-rays in trachea?
An X-ray of the chest may also be taken to assess the extent of congestion. High number of white blood cells in blood culture also indicates towards an infection.
Can a blow in the trachea cause radiation?
Injury apart from inhalation of toxic substances can also occur with physical factors. Usually a blow may not injure the trachea. However, radiation treatment is one possible cause although uncommon. A radiation injury to the trachea is usually as a result of cancer treatment of either the larynx or thyroid gland.