
Is Mycobacterium tuberculosis aerobic or anaerobic?
Mycobacterium tuberculosis is a strict aerobe capable of prolonged survival in the absence of oxygen. We investigated the ability of anaerobic M. tuberculosis to counter challenges to internal pH homeostasis in the absence of aerobic respiration, the primary mechanism of proton efflux for aerobic bacilli.
What are the characteristics of Mycobacterium?
Microbiologic characteristics. Mycobacteria are aerobic. They are bacillary in form, at least in most phases that have attracted human microbiological attention to date; they are straight or slightly curved rods between 0.2 and 0.6 µm wide and between 1.0 and 10 µm long.
Are bacteria aerobic or anaerobic?
These bacteria require a lot of oxygen their very makeup is aerobic which is true of animals, fungi and many other bacteria. Molds and singular human cells are composed of a specialized anaerobic type of cell called a faculative anaerobe. Anaerobic organisms do not need oxygen for growth and faculative anaerobes can use the oxygen or not.
What is the most important Mycobacterium species?
Clinically, the most important species is Mycobacterium tuberculosis, which causes tuberculosis in humans. Tuberculosis in cattle and humans is also caused by Mycobacterium bovis, whilst Mycobacterium africanum is a rare cause of human tuberculosis in central Africa.
Is mycobacteria aerobic or anaerobic?
Mycobacterium is a dominant genus in the soil, and all its species are obligate aerobes.
Is Mycobacterium an anaerobe?
Mycobacteria are rod-shaped, Gram-positive aerobes, or facultative anaerobes.
Is Mycobacterium Genavense aerobic or anaerobic?
Mycobacteria are generally considered to be aerobic; however, Wayne and Hayes recently reported that Mycobacterium tuberculosis can adapt to low oxygen concentrations (17), and Realini et al. showed enhanced growth of Mycobacterium genavense under microaerophilic conditions (16).
Is Mycobacterium tuberculosis an anaerobe?
M. tuberculosis is a tiny thin obligate aerobic (3 µm in length and 0.5 µm in width), acid-fast and a Gram-positive pathogen. As mentioned above, it can also be a facultative anaerobe. It is metabolically catalase-and phenylase-positive.
Are mycobacteria aerobic?
Metabolism and morphology Mycobacteria are aerobic. They are bacillary in form, at least in most phases that have attracted human microbiological attention to date; they are straight or slightly curved rods between 0.2 and 0.6 µm wide and between 1.0 and 10 µm long.
Are mycobacteria strictly aerobic?
Examples of obligately aerobic bacteria include Mycobacterium tuberculosis (acid-fast), Pseudomonas aeruginosa (Gram-negative), Bacillus (Gram-positive), and Nocardia asteroides (Gram-positive). With the exception of the yeasts, most fungi are obligate aerobes.
Does Mycobacterium need oxygen?
Introduction. Mycobacterium tuberculosis is an obligate aerobe bacteria requiring oxygen in its metabolism processes.
What are the characteristics of Mycobacterium?
Mycobacteria are Gram-positive, catalase positive, non-motile, non-spore forming rod-shaped bacteria (0.2–0.6 μm wide and 1.0–10 μm long). The colony morphology of mycobacteria varies with some species growing as rough or smooth colonies. Colony colour ranges from white to orange or pink (Iivanainen, 1999).
What is the classification of Mycobacterium?
Taxonomically, mycobacteria belong to the genus Mycobacterium, which is the single genus within the family of Mycobacteriaceae, in the order Actinomycetales.
Why is Mycobacterium tuberculosis aerobic?
The physiology of M. tuberculosis is highly aerobic and requires high levels of oxygen. Primarily a pathogen of the mammalian respiratory system, it infects the lungs....Mycobacterium tuberculosisFamily:MycobacteriaceaeGenus:MycobacteriumSpecies:M. tuberculosisBinomial name10 more rows
How does Mycobacterium respire?
Electron donors fueling respiration in mycobacteria Mycobacterial species use a variety of primary dehydrogenases to deliver electrons from central metabolism into the respiratory chain to generate energy (Figure 1).
Does Mycobacterium tuberculosis need oxygen to survive?
Mycobacterium tuberculosis is a strict aerobe capable of prolonged survival in the absence of oxygen.
What are anaerobic bacteria examples?
Some examples of facultative anaerobic bacteria are Staphylococcus (Gram positive), Escherichia coli and Shewanella oneidensis (Gram negative), and Listeria (Gram positive).
Which of these are anaerobes?
Two examples of obligate anaerobes are Clostridium botulinum and the bacteria which live near hydrothermal vents on the deep-sea ocean floor. Aerotolerant organisms, which cannot use oxygen for growth, but tolerate its presence.
Are Mycobacterium obligate aerobes?
Mycobacterium is a dominant genus in the soil, and all its species are obligate aerobes.
Which organism is an obligate anaerobe?
requirements of bacteria … methane-producing archaea (methanogens), are called obligate anaerobes because their energy-generating metabolic processes are not coupled with the consumption of oxygen. In fact, the presence of oxygen actually poisons some of their key enzymes.
What is the effect of acidic pH on anaerobic bacteria?
An acidic environmental pH greatly increased the susceptibilities of anaerobic bacilli to the collapse of the proton motive force by protonophores, to antimicrobial compounds that target entry into the electron transport system, and to small organic acids with uncoupling activity.
Do anaerobic bacteria tolerate pH?
However, anaerobic bacilli exhibited high tolerance against these challenges at a near-neutral pH. At a slightly alkaline pH, which was near the optimum intracellular pH, the addition of protonophores even improved the long-term survival of bacilli.
Why is M. tuberculosis waxy?
First discovered in 1882 by Robert Koch, M. tuberculosis has an unusual, waxy coating on its cell surface primarily due to the presence of mycolic acid. This coating makes the cells impervious to Gram staining, and as a result, M. tuberculosis can appear either Gram-negative or Gram-positive.
What are the host derived lipids in M. tuberculosis?
tuberculosis, consisting entirely of host-derived lipids such as fats and cholesterol. Bacteria isolated from the lungs of infected mice were shown to preferentially use fatty acids over carbohydrate substrates.
What is the growth rate of M. tuberculosis?
Compared to other commonly studied bacteria, M. tuberculosis has a remarkably slow growth rate, doubling roughly once per day. Commonly used media include liquids such as Middlebrook 7H9 or 7H12, egg-based solid media such as Lowenstein-Jensen, and solid agar-based such as Middlebrook 7H11 or 7H10.
Why are granulomas formed in M. tuberculosis?
Protective granulomas are formed due to the production of cytokines and upregulation of proteins involved in recruitment.
What is the best way to identify M. tuberculosis?
Acid-fast stains such as Ziehl–Neelsen, or fluorescent stains such as auramine are used instead to identify M. tuberculosis with a microscope. The physiology of M. tuberculosis is highly aerobic and requires high levels of oxygen. Primarily a pathogen of the mammalian respiratory system, it infects the lungs.
When was tuberculosis first discovered?
M. tuberculosis, then known as the " tubercle bacillus ", was first described on 24 March 1882 by Robert Koch, who subsequently received the Nobel Prize in Physiology or Medicine for this discovery in 1905; the bacterium is also known as "Koch's bacillus".
Where did M. tuberculosis evolve?
Evolution. The M. tuberculosis complex evolved in Africa and most probably in the Horn of Africa. In addition to M. tuberculosis, the M. tuberculosis complex (MTBC) has a number of members infecting various animal species, these include M. africanum, M. bovis (Dassie's bacillus), M. caprae, M. microti, M. mungi, M. orygis, and M. pinnipedii.
How to differentiate mycobacterium tuberculosis from anaerobic bacteria?
Mycobacterium tuberculosis bacteria, like other aerobic bacteria, can be differentiated from anaerobic bacteria by putting them to grow in a liquid culture that has been placed in a test tube and watching to see whether they congregate toward the top or the bottom of the culture.
Where do aeorobic and anaeorobic bacteria locate?
The aeorobic bacteria will locate very near the top of the solution, while the anaeorobic bacteria will locate as near to the bottom as they can, this is because the aeorobic bacteria are seeking the oxygen which is located at the top of the solution and the anaeorobic bacteria are avoiding it. The Mycobacterium tuberculosis bacteria, in addition ...
What is the bacteria responsible for tuberculosis?
The Mycobacterium tuberculosis bacteria is the bacteria that is responsible for causing tuberculosis, or, in most instances this is the mycobacteria behind the infection. These bacteria require a lot of oxygen their very makeup is aerobic which is true of animals, fungi and many other bacteria.
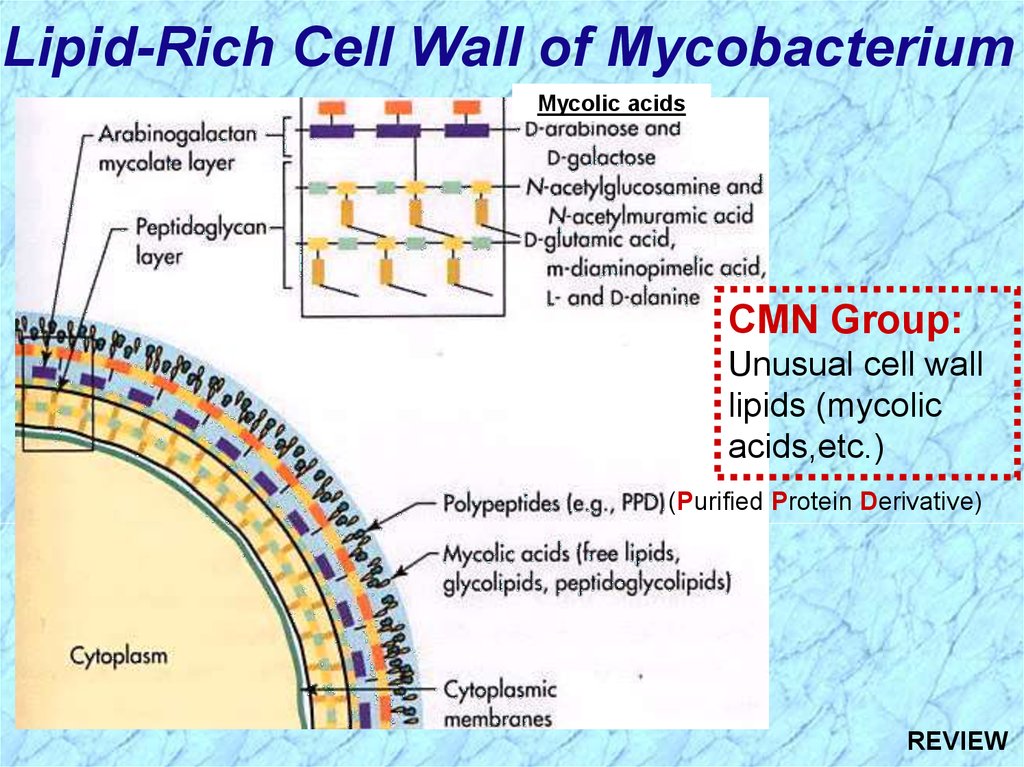
What is the cell wall of Mycobacterium tuberculosis?
Mycobacterium tuberculosis is a bacillus or rod shaped bacteria. It has a unique and lipid cell wall that is composed primarily of mycolic acid and a high resistance to the human macrophages, which are part of the immune network involving antibodies and white blood cells, as well as most drugs.
What are the pathways that bacteria need to invade the human body?
To invade the human body the bacteria need a pathway. Pathways can occur during treatments for other disorders such as chemotherapy or an antibiotic therapy. The pathways can occur if the person is infected with the HIV virus and during other run down conditions.
Which bacteria are most likely to cause disease in humans?
The tuberculosis bacteria, Mycobacterium tuberculosis, is the most common harmful or pathogenic bacteria that is known to instigate disease in humans of all the bacteria.
When was M. tuberculosis discovered?
Mycobacterium tuberculosis was only discovered in 1882 like many diseases tuberculosis was much less well understood before the discovery of the bacteria or viruses ...
What are the habitats of mycobacteria?
Artificial habitats such as sewage sludge and water distribution systems are colonized by a considerable number of Mycobacterium species. Aquatic mycobacteria colonize biofilms at solid-water and air-water interfaces, which seem to be important replication sites in oligotrophic habitats (Schulze-Röbbecke, 1993 ).
Where can I find mycobacteria?
Mycobacteria are often found in waters that receive runoff from pasture land and in a study of the River Tywi in South Wales, UK, 48 of 70 water samples (69%) were contaminated with M. avium subsp. paratuberculosis ( Pickup et al., 2006 ).
How many species are there in the Mycobacterium genus?
The genus Mycobacterium is composed of more than 100 recognized or proposed species. The most familiar pathogens are Mycobacterium tuberculosis complex (tuberculosis) and Mycobacterium leprae (leprosy or Hansen’s disease). Mycobacterium species produce a wide spectrum of infections in humans and animals ranging from localized lesions to disseminated disease. Most of the nontuberculous mycobacteria live freely in the environment and some have been implicated as opportunistic pathogens in patients with underlying lung disease, immunosuppression, or percutaneous trauma. New rapid culture methods and the application of molecular biology have decreased the time required to isolate and identify clinically significant mycobacteria.
How are mycobacteria phylogenetic studies based?
Phylogenetic studies of the genus Mycobacterium have been based, in the past three decades, on the sequence of the 16S rRNA gene, on concatenated sequences of a few housekeeping genes and, very recently, on whole genome sequences. Surprisingly these approaches produced highly consistent phylogenetic reconstructions. In all cases, the rapidly and slowly growing species were clearly separated. The species composition of the major clusters was largely overlapping and one of them, the M. terrae complex, constantly took its place between the branches leading to rapid and slow growers. The clade of rapid growers including the species of the M. abscessus-chelonae complex was revealed to be the most ancestral and is located close to the root of the genus. The pathogenic species ( M. tuberculosis and M. leprae) clustered together with most species frequently involved in opportunistic human infections. The major discrepancies among different phylogenetic approaches occurred with a group of species genetically related to M. simiae; the large grouping defined by the 16S sequences emerged scaled down in the phylogeny inferred by the whole genome sequences with most of them reallocated among other, apparently unrelated, species.
What is the purpose of cell division in Mycobacterium spp.?
involves asymmetric septal placement in growing cells, which need to be converted to binary fission with equipartition of the chromosome to prevent loss of genomic information.
What temperature does M. avium colonize?
Temperature plays an important role in the mycobacterial colonization of water systems, with M. avium prolific in hospital water supplies at temperatures of 52–57°C and M. avium levels are higher in hot rather than cold water systems ( Du Moulin, 1988 ).
When was Mycobacterium introduced?
Lehmann and Neumann first introduced the genus Mycobacterium into the scientific literature in 1896. The subsequent history of the genus has been profoundly influenced by the fact that only very few of the more than over 100 currently recognized species have been a devastating cause of human disease and suffering, above all M. tuberculosis. Thus, studies of microbial physiology, structure, genetics and diagnostic tools have mainly focused on M. tuberculosis and secondarily on Mycobacterium leprae.
Where is mycobacterium abscessus found?
It is part of a group known as rapidly growing mycobacteria and is found in water, soil, and dust. It has been known to contaminate medications and products, including medical devices.
What is the skin color of mycobacterium abscessus?
Mycobacterium abscessus. Skin infected with M. abscessus is usually red, warm, tender to the touch, swollen, and/or painful. Infected areas can also develop boils or pus-filled vesicles. Other signs of M. abscessus infection are fever, chills, muscle aches, and a general feeling of illness.
What is the name of the bacterium that causes tuberculosis?
General information about Mycobacterium abscessus. Mycobacterium abscessus [mī–kō–bak–tair–ee–yum ab–ses–sus] (also called M. abscessus) is a bacterium distantly related to the ones that cause tuberculosis and Hansen’s Disease (Leprosy). It is part of a group of environmental mycobacteria and is found in water, soil, and dust.
How does M. abscessus spread?
abscessus can occur in several ways. Infection with M. abscessus is usually caused by injections of substances contaminated with the bacterium or through invasive medical procedures employing contaminated equipment or material .
Where is M. abscessus found?
It is part of a group of environmental mycobacteria and is found in water, soil, and dust. It has been known to contaminate medications and products, including medical devices. M. abscessus can cause a variety of infections. Healthcare-associated infections due to this bacterium are usually of the skin and the soft tissues under the skin.
Can a bacterium be found in blood?
When the infection is severe, the bacterium can be found in the blood and isolated from a blood sample. To make the diagnosis, your healthcare provider will have to take a sample from the infected area and/or blood and send it to a laboratory for identification.
What is a nontuberculous mycobacteria?
Nontuberculous mycobacteria (NTM) are emerging human pathogens, causing a wide range of clinical diseases affecting individuals who are immunocompromised and who have underlying health conditions. NTM are ubiquitous in the environment, with certain species causing opportunistic infection in humans, including Mycobacterium aviumand Mycobacterium ...
What are the characteristics of M. aviumare?
aviumare discussed. M. aviumsubsp. Hominissus(MAH) is an opportunistic environmental pathogen for humans, swine, and other animals that are found in soil and water. Drinking water and tap aerosols are considered the primary sources for infection in humans.
What is MAC in a pulmonary infection?
Treatment of Mycobacterium avium/MAC Infections. The Mycobacterium aviumcomplex (MAC) consists of most of the common pulmonary NTM pathogens that are heavily linked to the causes of human disease in almost all regions of the world [66].
Is M. abscessusinfection a pulmonary disease?
M. abscessusinfections are considered one of the most antibiotic-resistant mycobacteria and are associated with pulmonary disease , especially cystic fibrosis, as well as contaminated traumatic skin wounds, postsurgical soft tissue infections, and healthcare-associated infections (HAI).

Overview
Mycobacterium tuberculosis (M. tb) is a species of pathogenic bacteria in the family Mycobacteriaceae and the causative agent of tuberculosis. First discovered in 1882 by Robert Koch, M. tuberculosis has an unusual, waxy coating on its cell surface primarily due to the presence of mycolic acid. This coating makes the cells impervious to Gram staining, and as a result, M. tuberculosis can appear …
Microbiology
M. tuberculosis was found in a complex in 2019 that has at least 9 members: M. tuberculosis sensu stricto, M. africanum, M. canetti, M. bovis, M. caprae, M. microti, M. pinnipedii, M. mungi, and M. orygis. It requires oxygen to grow, it is debated whether it produces spores, and is nonmotile. M. tuberculosis divides every 18–24 hours. This is extremely slow compared with other bacteria, which tend to have division times measured in minutes (Escherichia coli can divide roughly ever…
Pathophysiology
Humans are the only known reservoirs of M. tuberculosis. A misconception is that M. tuberculosis can be spread by shaking hands, making contact with toilet seats, sharing food or drink, or sharing toothbrushes. However, major spread is through air droplets originating from a person who has the disease either coughing, sneezing, speaking, or singing.
Genome
The genome of the H37Rv strain was published in 1998. Its size is 4 million base pairs, with 3,959 genes; 40% of these genes have had their function characterized, with possible function postulated for another 44%. Within the genome are also six pseudogenes.
The genome contains 250 genes involved in fatty acid metabolism, with 39 of these involved in the polyketide metabolism generating the waxy coat. Such large numbers of conserved genes show …
Evolution
The M. tuberculosis complex evolved in Africa and most probably in the Horn of Africa. In addition to M. tuberculosis, the M. tuberculosis complex (MTBC) has a number of members infecting various animal species, these include M. africanum, M. bovis (Dassie's bacillus), M. caprae, M. microti, M. mungi, M. orygis, and M. pinnipedii. This group may also include the M. canettii clade. These animal strains of MTBC do not strictly deserve species status, as they are all closely relat…
Antibiotic resistance (ABR)
M. tuberculosis is a clonal organism and does not exchange DNA via horizontal gene transfer. Despite an additionally slow evolution rate, the emergence and spread of antibiotic resistance in M. tuberculosis poses an increasing threat to global public health. In 2019, the WHO reported the estimated incidence of antibiotic resistant TB to be 3.4% in new cases, and 18% in previously treated cases. Geographical discrepancies exist in the incidence rates of drug-resistant TB. Cou…
Host genetics
The nature of the host-pathogen interaction between humans and M. tuberculosis is considered to have a genetic component. A group of rare disorders called Mendelian susceptibility to mycobacterial diseases was observed in a subset of individuals with a genetic defect that results in increased susceptibility to mycobacterial infection.
Early case and twin studies have indicated that genetic components are important in host susce…
DNA repair
As an intracellular pathogen, M. tuberculosis is exposed to a variety of DNA-damaging assaults, primarily from host-generated antimicrobial toxic radicals. Exposure to reactive oxygen species and/or reactive nitrogen species causes different types of DNA damage including oxidation, depurination, methylation, and deamination that can give rise to single- and double-strand breaks (DSBs).