Type 2 MI is defined as “myocardial infarction secondary to ischaemia due to either increased oxygen demand or decreased supply, e.g. coronary artery spasm, coronary embolism, anaemia
Anemia
A state in which hemoglobin in blood is below the reference range.
Irregular Heartbeat
Any change from the normal sequence of heart's impulses causing the heart to beat too fast, too slow, or erratically.
High blood pressure (hypertension)
High pressure in the arteries (vessels that carry blood from the heart to the rest of the body).
Full Answer
What is type 2 myocardial infarction?
Expert Analysis. Type 2 MI is defined as "myocardial infarction secondary to ischaemia due to either increased oxygen demand or decreased supply, e.g. coronary artery spasm, coronary embolism, anaemia, arrhythmias, hypertension or hypotension.". The definition of type 2 MI is unsatisfactory because it is not really defined by what it is...
What is a type 2 mi?
Type 2 MI is defined as "myocardial infarction secondary to ischaemia due to either increased oxygen demand or decreased supply, e.g. coronary artery spasm, coronary embolism, anaemia, arrhythmias, hypertension or hypotension."
Is type 2 myocardial injury more dangerous than Type 1 mi?
In most, studies, 11, 20, 29 both short- and long-term mortality were higher among patients with type 2 MI or myocardial injury than in patients with type 1 MI ( Table 2, Figure 2 ). 9, 10, 17, 18, 23–25 Differences in type 2 MI mortality between studies are likely explained by differences in patient selection.
How serious is a type 2 heart attack?
A "type 2" heart attack caused by severely restricted blood flow can be just as serious as a heart attack caused by a sudden complete blockage. In TV shows and movies, a man having a heart attack typically clutches his chest and falls to the ground, but most heart attacks are not nearly as dramatic.

What is Type 2 heart attack?
Type 2: A heart attack occurring when the heart needs more oxygen than it can get. This type of heart attack is an oxygen demand problem, resulting from higher need for blood flow. Type 3: A fatal heart attack that causes death before the diagnosis can be confirmed with blood tests.
Is a Type 2 MI serious?
Type 2 MI is distinguished from myocardial injury without acute ischemia, for example, acute heart failure and myocarditis. Type 2 MI is associated with a poor outcome. Several studies have demonstrated higher mortality rates among patients with type 2 MI as compared with patients with type 1 MI.
What does type 2 MI mean in medical terms?
Type 2 myocardial infarction (MI) is defined by a rise and fall of cardiac biomarkers and evidence of ischemia without unstable coronary artery disease (CAD), due to a mismatch in myocardial oxygen supply and demand. Myocardial injury is similar but does not meet clinical criteria for MI.
Is Type 1 or Type 2 MI worse?
Compared with type 1 MI, patients with type 2 MI had significantly worse survival free from cardiovascular death over long-term follow-up (unadjusted HR: 2.0; 95% CI: 1.6 to 2.7; p < 0.001).
Is MI considered heart attack?
A lack of blood flow can damage or destroy part of the heart muscle. A heart attack is also called a myocardial infarction. Prompt treatment is needed for a heart attack to prevent death. Call 911 or emergency medical help if you think you might be having a heart attack.
What causes a type 2 myocardial infarction?
[1] Type-II MI was defined as MI secondary to ischemia due to either increased oxygen demand or decreased supply caused by conditions as coronary artery spasm, coronary embolism, anemia, arrhythmias, hypertension, or hypotension.
Do you treat type 2 MI?
Treatment of type 2 MI is to treat the underlying condition and hence remove the cardiac insult. To adequately assess the prognosis and determine appropriate further treatment in patients with type 2 MI, information about whether the patient has (or is likely to have) significant underlying CAD is essential.
What is the difference between Type 1 and Type 2 MI?
Type 1 MI is a primary coronary arterial event attributable to atherothrombotic plaque rupture or erosion. Type 2 MI occurs secondary to an acute imbalance in myocardial oxygen supply and demand without atherothrombosis.
What are the 4 types of myocardial infarction?
A heart attack is also known as a myocardial infarction....The three types of heart attacks are:ST segment elevation myocardial infarction (STEMI)non-ST segment elevation myocardial infarction (NSTEMI)coronary spasm, or unstable angina.
What is the difference between NSTEMI and type 2 MI?
(NSTEMI) is a common diagnosis in hospitalized patients. Type 2 has been reported up to 25% of cases of MI depending on the population studied. Type 2 NSTEMI is defined as myocardial ischemia resulting from mismatched myocardial oxygen supply and demand that is not related to unstable coronary artery disease (CAD).
Can you survive with high troponin levels?
A positive troponin result (that is, higher than the upper limit of normal) signified a 3.2 higher mortality hazard (95% confidence interval 3.1 to 3.2) over three years. Mortality varied noticeably with age, with a hazard ratio of 10.6 (8.5 to 13.3) in 18-29 year olds and 1.5 (1.4 to 1.6) in those older than 90.
What happens if myocardial infarction is not treated?
If a person does not receive immediate treatment, this lack of blood flow can cause damage to the heart. Complications arising from this situation include: Arrhythmias: These are abnormal heartbeats. Cardiogenic shock: This refers to severe damage to the heart muscle.
What is a Type 2 troponin elevation?
Type II MI is defined as the detection of a rise and/or fall of cardiac troponin values with at least one value above the 99th percentile of the upper reference limit, and evidence of an imbalance between myocardial oxygen supply and demand unrelated to coronary thrombosis, requiring at least one of the following ...
What is a Type 3 myocardial infarction?
The type 3 myocardial infarction was defined according to the Universal definition of myocardial infarction, that is, cardiac death with symptoms suggestive of myocardial ischemia and presumed new ischemic ECG changes or new left bundle branch block, but death occurring before blood samples could be obtained, before ...
What are 4 signs of myocardial infarction?
What are the symptoms of heart attack?Chest pain or discomfort. ... Feeling weak, light-headed, or faint. ... Pain or discomfort in the jaw, neck, or back.Pain or discomfort in one or both arms or shoulders.Shortness of breath.
What triggers myocardial infarction?
Acute myocardial infarction is triggered by various factors, such as physical exertion, stressful events, heavy meals, or increases in air pollution.
How long can you live after a myocardial infarction?
About 68.4 per cent males and 89.8 per cent females still living have already lived 10 to 14 years or longer after their first infarction attack; 27.3 per cent males, 15 to 19 years; and 4.3 per cent, 20 years or longer; of the females, one is alive 15 years, one 23 years and one 25 years or longer.
How many types of myocardial infarction are there?
STEMI, NSTEMI, and type 2 MI. Type 1 MI can be further divided into two classifications: ST‐elevation myocardial infarction (STEMI) and non‐ST‐elevation myocardial infarction (NSTEMI).
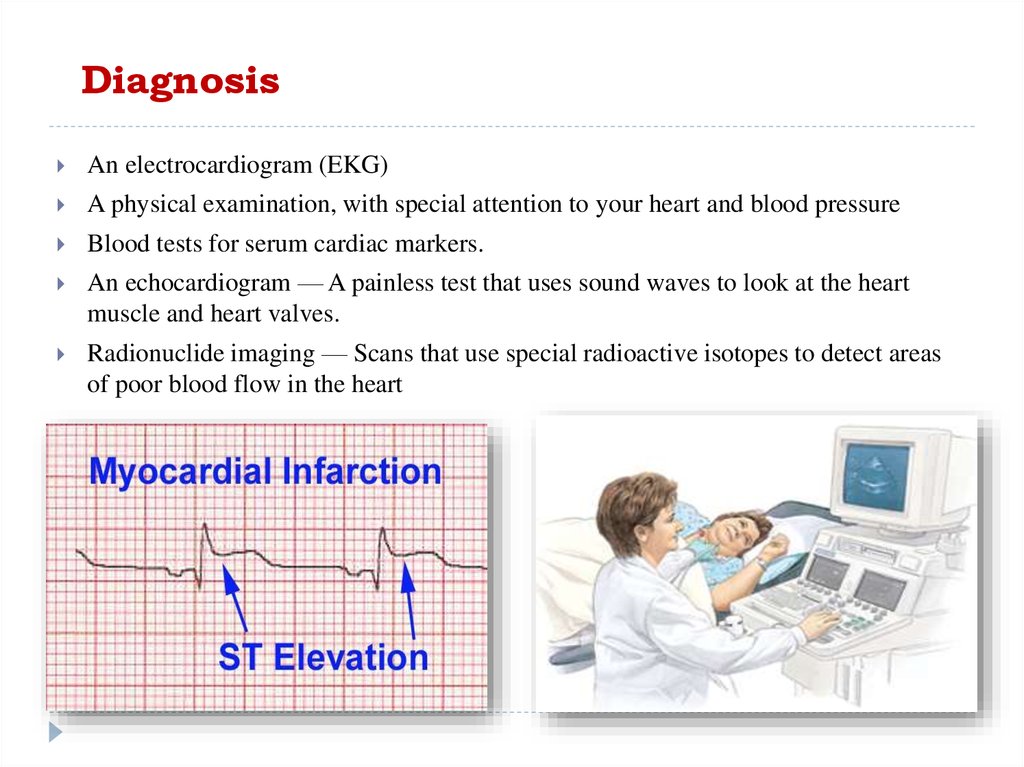
What tests confirm a diagnosis of myocardial infarction?
Diagnosis of a heart attack includes checking blood pressure, pulse and temperature. Tests are done to see how the heart is beating and to check overall heart health....TestsElectrocardiogram (ECG or EKG). ... Blood tests. ... Chest X-ray. ... Echocardiogram. ... Coronary catheterization (angiogram). ... Cardiac CT or MRI .
What is considered a high troponin level?
InterpretationConcentration (ng/mL)Interpretation< 0.04Normal0.04 - 0.39Elevated above the 99th percentile of a healthy population.Oct 4, 2022
What are the 4 types of myocardial infarction?
A heart attack is also known as a myocardial infarction....The three types of heart attacks are:ST segment elevation myocardial infarction (STEMI)non-ST segment elevation myocardial infarction (NSTEMI)coronary spasm, or unstable angina.
What is a normal level of troponin?
The normal levels of troponin in the blood are very low. Usual results are 0 to 0.04 nanograms per milliliter. Such low levels are difficult to measure accurately with standard testing.
What is the type of MI?
Type 1: Spontaneous MI caused by ischemia due to a primary coronary event (eg, plaque rupture, erosion, or fissuring; coronary dissection) Type 2: Ischemia due to increased oxygen demand (eg, hypertension), or decreased supply (eg, coronary artery spasm or embolism, arrhythmia, hypotension)
Is takotsubo type 2 MI?
It is an exclusion diagnosis, encompassing many conditions and including both type 1 and 2 MI. Myocardial injury, myocarditis and takotsubo syndrome do not come under the terminology because they are not MI.
What is the implication of Type 2 MI?
There is always an underlying etiology. The implication of a Type 2 MI is that it portends a worse prognosis for the causative condition.
When to consider Type 2 MI?
If you note an abnormal troponin early and you are interacting with a provider verbally and concurrently, bring it to their attention. It is optimal to consider Type 2 MI early, and to diagnose or rule out subsequently. I would not formally query unless and until the condition declares itself.
What is type 3 MI?
Type 3 MI, which is cardiac death with symptoms of myocardial ischemia and suggestive EKG changes, but demise occurs before any biomarker trending can be demonstrated;
What is myocardial infarction?
Myocardial infarction is a specific subset of myocardial injury. The definition of MI includes a rise and/or fall (depending on when the patient is encountered in the evolution of the MI) of a cardiac biomarker signifying cell death, with at least one value above the 99 th percentile upper reference limit (URL), plus some evidence of myocardial ischemia (be it symptoms, EKG or imaging evidence, or demonstration of a thrombus).
What is MI in cardiology?
Acute myocardial infarction (MI) is the term for myocardial necrosis, or cell death, in a clinical setting, consistent with myocardial ischemia. “Ischemia” implies insufficient blood perfusion, and prolonged ischemia results in cell death.
What is the third universal definition of myocardial infarction?
Such is the case with troponin. In October 2012, the Third Universal Definition of Myocardial Infarction (TUDMI) was published by the American Heart Association, redefining myocardial infarction (MI).
What is the ICD-10 code for a type 2 MI?
One of the problems providers have had with diagnosing Type 2 MI was that there was no unique code for a Type 2 MI until October 2017. This meant that every time a Type 2 MI was diagnosed, the patient was marked as having atherosclerotic heart disease, and the core measures were initiated. Last October, the code I21.A1, Myocardial infarction, Type 2, was added to ICD-10-CM.
What is a type 2 MI?
Type 2 myocardial infarction (MI) is defined by a rise and fall of cardiac biomarkers and evidence of ischemia without unstable coronary artery disease (CAD), due to a mismatch in myocardial oxygen supply and demand. Myocardial injury is similar but does not meet clinical criteria for MI. There is uncertainty regarding clinical characteristics, management and outcomes of type 2 MI and myocardial injury in comparison to type 1 MI.
What is the diagnosis of myocardial infarction?
According to the Universal Definition of Myocardial Infarction (MI), the diagnosis of MI requires the rise and/or fall of cardiac biomarkers with clinical evidence of ischemia, defined by symptoms, electrocardiographic (ECG) changes, or new regional wall motion abnormalities. Since 2007, this definition has classified MI into 5 distinct subtypes.1In contrast to MI due to an acute coronary syndrome (type 1 MI), type 2 MI is defined as a mismatch in myocardial oxygen supply and demand that is not attributed to unstable coronary artery disease (CAD). Type 2 MI has been reported in 2% to 25% of cases of MI, depending on the population studied and the sensitivity of the cardiac biomarker assay.2–11Although type 2 MI has been formally described for a decade, there remains considerable uncertainty regarding its pathogenesis, provoking factors, optimal medical management, and long-term outcomes.2,12Myocardial injury without definite MI, defined by a rise and/or fall in cardiac biomarkers that does not fulfill the Universal Definition criteria for MI, has also been increasingly recognized as a significant entity. Myocardial injury is well characterized in the post-operative period following non-cardiac surgery and is strongly associated with short-term mortality.3,13,14The aim of the present study was to evaluate clinical characteristics, medical treatment, and intermediate-term cardiovascular outcomes of all patients admitted to a large urban Veterans Affairs (VA) hospital with abnormal cardiac biomarkers by myocardial injury and MI subtype.
What are the most common provoking conditions associated with a mismatch in myocardial oxygen supply and demand?
Provoking conditions associated with type 2 MI and myocardial injury are shown in Table 1. Overall, tachyarrhythmia (34.3%), severe hypertension (21. 8%), and anemia (19.9%) were the most common provoking conditions associated with a mismatch in myocardial oxygen supply and demand. Non-cardiac surgery was a provoking condition of myocardial injury or type 2 MI in 11.8% of cases. Among patients with any myocardial injury after non-cardiac surgery, only 21% (8/38) met the universal definition for type 2 MI. Multiple provoking conditions were identified in 41% of patients with type 2 MI or myocardial injury without definite MI.
What is the risk of death for type 2 MI?
The risk profile of patients with type 2 MI and nonischemic myocardial injury differs significantly from patients with type 1 MI; they are at higher risk of death from noncardiovascular causes. This competing risk of noncardiovascular death is important, and may explain some of the observed variability in major adverse cardiovascular event (MACE) rates in observational data sets to date. In a study of consecutive hospitalized patients with myocardial injury, MACE rates were similar between participants with type 2 MI (30%), type 1 MI (33%), and nonischemic myocardial injury (31%). 24 In a multivariable model that attempted to account for competing risk of death between subclassifications, the adjusted risk of 5-year MACE was lower in type 2 MI versus type 1 MI (risk ratio, 0.74 [95% CI, 0.62–0.88]). 24 The higher mortality but similar or lower MACE rate among type 2 MI and nonischemic myocardial injury versus type 1 MI suggests this risk of death is driven by patient comorbidities rather than by complications of ischemia or necrosis. This hypothesis is further supported by the fact that high cardiovascular and noncardiovascular mortality in type 2 MI and nonischemic myocardial injury occurs despite quantitatively less myocardial injury versus type 1 MI, as reflected by a lower median peak cTn level ( Figures 2 and 3, Table 2 ).
How long does a type 2 MI stay in the hospital?
In a US Veterans Affairs cohort, the duration of hospital stay among patients with type 2 MI (median, 7 [intraquartile range, 2–17 days]) and nonischemic myocardial injury (10 [intraquartile range, 4–23 days]) was double in comparison with type 1 MI (4 [intraquartile range, 2–7 days]), 23 but readmission rates over an average of 1.8 years of follow-up were similar (type 2 MI, 43%; type 1 MI, 42%; and nonischemic myocardial injury, 46%). 25
What is the consensus classification of MI?
Consensus in classification will facilitate effective research and design of therapeutic studies for these common entities across different medical facilities. In the absence of evidence for type 1 MI, we propose the default position of acute nonischemic myocardial injury for patients presenting with evidence of elevated cTn with a dynamic pattern and acute decompensated heart failure, sepsis, or postoperative state from a noncardiac procedure, and to reserve the designation of type 2 MI for those patients with acute myocardial injury and clear evidence of ischemia or notable extracardiac supply/demand mismatch (eg, significant tachycardia, hypertension, hypotension, hypoxemia, or anemia) or acute nonatherothrombotic coronary obstruction (eg, dissection, embolization).
What is myocardial infarction?
Myocardial infarction (MI) is defined pathologically as myocardial cell death attributable to prolonged myocardial ischemia ( inadequate oxygen supply to the myocardium). Each year, >8 million Americans present to the hospital with signs and symptoms suggestive of acute MI. 1 Approximately 700 000 are ultimately diagnosed with MI. 1, 2 Although coronary thrombus overlying a disrupted atherosclerotic plaque remains the hallmark and primary therapeutic target for MI, multiple other mechanisms are now known to contribute to MI and nonischemic causes of myocardial injury ( Table 1, Table I in the online-only Data Supplement, Figure 1 ); however, optimal diagnostic and treatment strategies for patients with myocardial injury attributable to these nonthrombotic mechanisms have yet to be defined. 3, 4
What is cardiac MRI?
Cardiac MRI is a noninvasive imaging modality for assessing myocardial dysfunction and, in conjunction with delayed contrast enhancement, can differentiate between acute and chronic myocardial injury via the presence of tissue edema. 59, 60 Ischemia-induced myocardial injury typically extends from the subendocardium to the epicardium, whereas nonischemic myocardial injury can be seen at the epicardium, mid-wall, or the insertion points of the right ventricle. MRI is not well suited to assess the coronary arterial anatomy because of its limited spatial resolution with standard protocols. At specialized centers, dedicated sequencers may allow the assessment of coronary arterial characteristics, including high-risk plaque and thrombus. 61 A major strength of MRI is its capability to identify conditions associated with myocardial injury not related to MI. Among patients presenting with suspected acute MI in whom obstructive CAD was excluded, MRI found evidence of acute myocarditis in 15% to 75% of patients 62 with an accuracy of 78% to 83% in comparison with histology/clinical diagnosis. 63 Cardiomyopathies, in particular, stress cardiomyopathy, are well characterized by MRI. 62
What are the symptoms of myocardial ischemia?
The UDMI notes the following symptoms, in various combinations, as associated with myocardial ischemia: chest, upper extremity, mandibular, or epigastric discomfort, and dyspnea or fatigue during exertion or at rest. 4 Although data on the duration of symptoms are lacking, experts have suggested a minimum of 10 minutes for symptoms to be considered consistent with MI. However, these symptoms, regardless of duration, are not specific for myocardial ischemia, and MI may occur with atypical symptoms or even without symptoms at all. 4 For example, an assessment of >4 million patients with MI found that 33% did not report chest pain on presentation. 34 A cardiac catheterization study of patients with a history of angina and known obstructive CAD reported denial of all typical symptoms of ischemia, including chest pain, in >30% of patients during ECG-confirmed ischemia induced via prolonged coronary balloon inflation. 35 Symptoms atypical for myocardial ischemia are more common in diabetic patients, the elderly, and women, 36 a combined demographic that accounts for the majority of patients ultimately diagnosed with acute MI. 37–40 Moreover, surveillance studies have found up to 45% of all MIs to be silent or unrecognized with mortality rates similar to recognized MIs. 41, 42
What is the importance of classification in myocardial injury?
Specifically, classification is important for the timely initiation of evidence-based therapies for patients with type 1 MI, including antiplatelet and anticoagulation therapies, and coronary revascularization. However, the use of diagnostic imaging modalities that use contrast agents must be weighed against the risk of nephropathy, radiation exposure, or nephrogenic systemic fibrosis, whereas the potential benefit of antithrombotic therapies must consider the risk of bleeding. Balancing the risk and benefit of each diagnostic and therapeutic modality requires an estimation of: (1) the likelihood of the diagnosis being considered, (2) the potential outcome of such a diagnosis in the presence or absence of treatment, and (3) the risk of side effects or complications from the diagnostic and therapeutic options, all in the context of patient-specific factors that influence these risks. Figures 4 and 5 illustrate a pragmatic systematic approach to the evaluation and management of patients with myocardial injury; however, the authors acknowledge that diagnostic certainty is not always possible.
What is a heart attack?
Acute coronary syndrome (ACS) is when the arteries that carry blood, oxygen, and nutrients get blocked. Heart attacks are a form of ACS. They occur when your heart doesn’t get enough blood supply. A heart attack is also known as a myocardial infarction.
What is a heart attack that can cause damage?
When most people think of a heart attack, they often think of a STEMI. A STEMI occurs when a coronary artery becomes completely blocked and a large portion of the muscle stops receiving blood. It’s a serious heart attack that can cause significant damage.
How long does it take to recover from a heart attack?
Your recovery from a heart attack will depend on its severity and how it was treated. It can take anywhere from one week to several weeks before you can return to all your regular activities, especially anything involving heavy lifting.
Can a heart attack cause permanent damage?
There is no permanent damage during a coronary artery spasm. While silent heart attacks aren’t as serious, they do increase your risk of another heart attack or one that may be more serious.
Can anxiety increase after a heart attack?
Feelings of anxiety or depression may also increase after a heart attack. Tell your doctor if you feel these emotions or if they interfere with your day-to-day activity. Your doctor can recommend steps to decrease anxiety.
Can a heart attack be a silent heart attack?
It occurs when one of the heart’s arteries tightens so much that blood flow stops or becomes drastically reduced. Only imaging and blood test results can tell your doctor if you’ve had a silent heart attack.
A "type 2" heart attack caused by severely restricted blood flow can be just as serious as a heart attack caused by a sudden complete blockage
In TV shows and movies, a man having a heart attack typically clutches his chest and falls to the ground, but most heart attacks are not nearly as dramatic.
Disclaimer
As a service to our readers, Harvard Health Publishing provides access to our library of archived content. Please note the date of last review or update on all articles. No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.
What is type 2 heart attack?
Type 2: A heart attack occurring when the heart needs more oxygen than it can get. This type of heart attack is an oxygen demand problem, resulting from higher need for blood flow.
Why is it important to distinguish between different types of heart attacks?
The distinctions are important, because the various types of heart attacks may be treated entirely differently. "Having a universally accepted language about the causes of heart attack is important to clinical studies of drugs and other approaches, which may benefit one type of heart attack, but not others," explains Dr.
What is the difference between type 4b and type 5?
Type 4b: A heart attack that occurs when a clot blocks blood flow through a stent—a small metal mesh tube that has been inserted in the artery during angioplasty to keep the artery open. Type 5: A heart attack that occurs during coronary artery bypass surgery.
What are the two common sites of a heart attack?
Blockage can occur in any of your coronary arteries. Two common sites are the right coronary artery (A) and the left anterior descending artery (B). When blockages occur in these locations, adjoining areas of the heart are damaged (shown shaded).
What happens when blood is stopped in the heart?
In a heart attack, the amount of blood reaching heart muscle cells is inadequate to keep them alive. Usually, something has stopped blood flow through an artery that nourishes the heart (a coronary artery). Most often, this occurs when a plaque of atherosclerosis ruptures, spilling its cholesterol-rich contents into the center ...
Why do we need a blood test for heart attack?
For this reason, the task force recommends performing a blood test to measure the level of troponin, a protein found in abundance in the heart muscle. An injured heart releases large quantities of troponin into the bloodstream. Having more than a certain level of troponin in the blood is a sign that you've likely had a heart attack.
What is type 4A?
Type 4a: A heart attack that occurs during angioplasty, a procedure in which a blocked blood vessel is opened with a balloon on the end of a flexible tube inserted in the artery.
What is a heart attack called?
The type of heart attack (also called myocardial infarction, or MI) you experienced determines the treatments that your medical team will recommend. A heart attack occurs when a blockage in one or more coronary arteries reduces or stops blood flow to the heart, which starves part of the heart muscle of oxygen.
Which P2Y 12 inhibitor is stronger?
The three P2Y 12 inhibitors currently available that could be prescribed are clopidogrel, prasugrel, and ticagrelor . Studies have shown that two of these drugs (ticagrelor, prasugrel) are “stronger” than clopidogrel, and are a little better at decreasing the complications of blood clots.
What is the ischemia guided strategy?
Both may involve a test called cardiac catheterization to examine the inside of your heart: The ischemia-guided strategy uses various drugs (antiplatelet agents and anticoagulants) to inhibit blood clot formation. The early invasive strategy will start with the use of various drugs (antiplatelet agents and anticoagulants) to inhibit blood clot ...
How long does P2Y 12 last?
A second type of antiplatelet agent, called a P2Y 12 inhibitor, is usually prescribed for months or years in addition to the aspirin therapy. The type of medication and the duration of your treatment will vary based on your condition and other risk factors.