It depends on the circumstances. Isolated cases should not been isolated. Infection prevention staff should ensure that universal precautions are used by all staff members.
How can Pseudomonas infections be prevented?
To prevent spreading Pseudomonas infections between patients, healthcare personnel must follow specific infection control precautions. These precautions may include strict adherence to hand hygiene and wearing gowns and gloves when they enter rooms where patients infected with Pseudomonas are staying.
What is a Pseudomonas infection?
Pseudomonas infections are infections caused by a kind of bacteria called Pseudomonas that’s commonly found in soil, water, and plants. The type that typically causes infections in people is called Pseudomonas aeruginosa.
How long do you have to take antibiotics for Pseudomonas?
A severe infection may require weeks of antibiotics that you’ll be given through an IV. Every pseudomonas bacteria is slightly different, and strains are constantly changing, so these types of infections can be hard to treat. Many times, you may need to take more than one kind of antibiotic.
What is the mortality and morbidity associated with Pseudomonas aeruginosa infections?
Multidrug-resistant Pseudomonas can be deadly for patients in critical care. An estimated 51,000 healthcare-associated P. aeruginosa infections occur in the United States each year. More than 6,000 (13%) of these are multidrug-resistant, with roughly 400 deaths per year attributed to these infections.
Is Pseudomonas contagious person to person?
Yes. Pseudomonas is contagious. Transmission is possible through contact with contaminated surfaces or equipment, and also the consumption of contaminated water or fruit and vegetables. It can also pass from person to person via contact with hands and skin.
Is Pseudomonas a contact?
In healthcare settings, Pseudomonas may spread through person-to-person contact. This may occur via the contaminated hands of healthcare personnel, or through direct contact with contaminated environmental surfaces or equipment.
Where can Pseudomonas aeruginosa be isolated?
Pseudomonas aeruginosa was most commonly isolated from sink (13.6%), then mops and cleaning buckets (9.1%) and least from theatre bed, nasal swab, floor, disinfectant, ear and wound swab (4.5%).
How is Pseudomonas aeruginosa transmitted in hospitals?
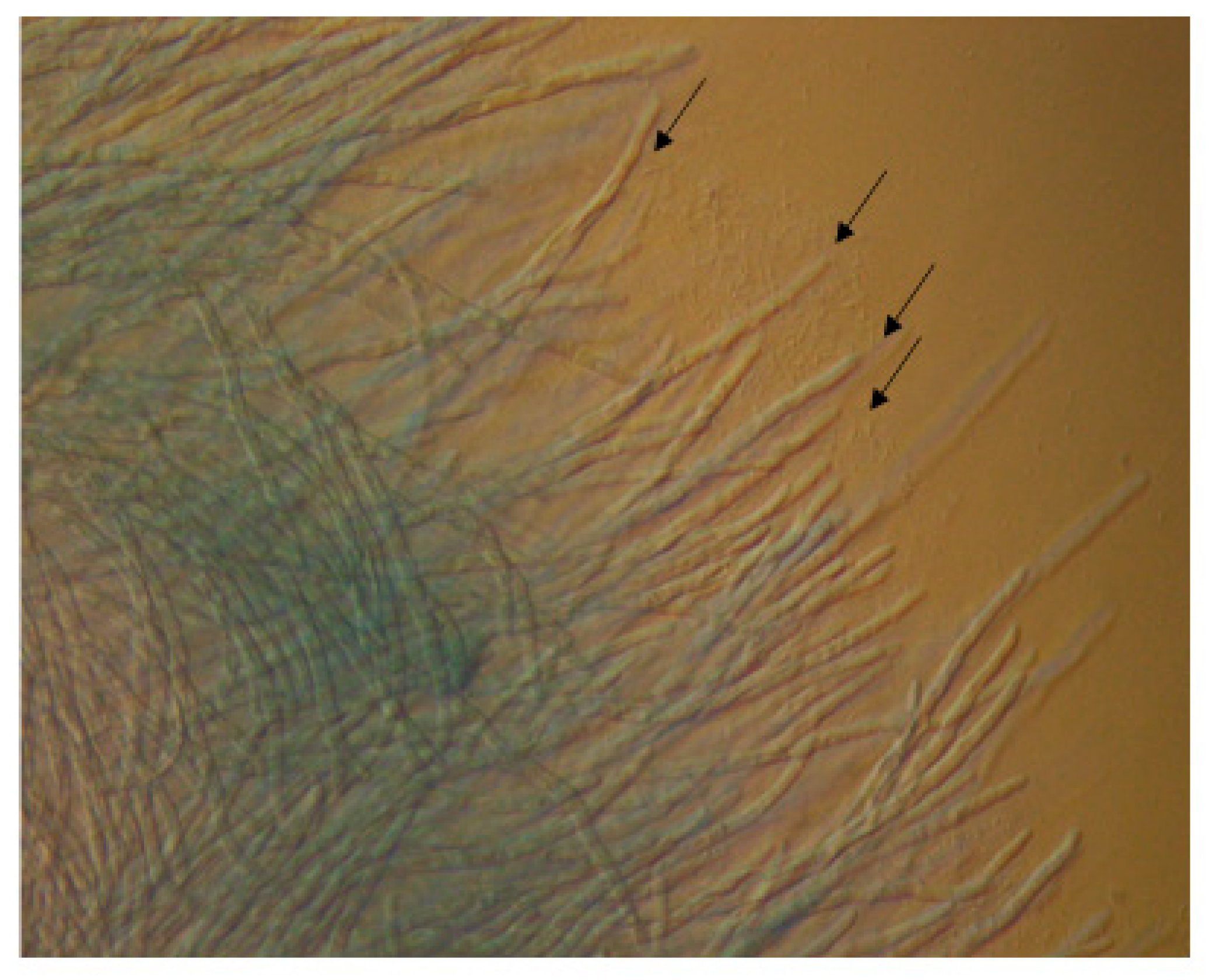
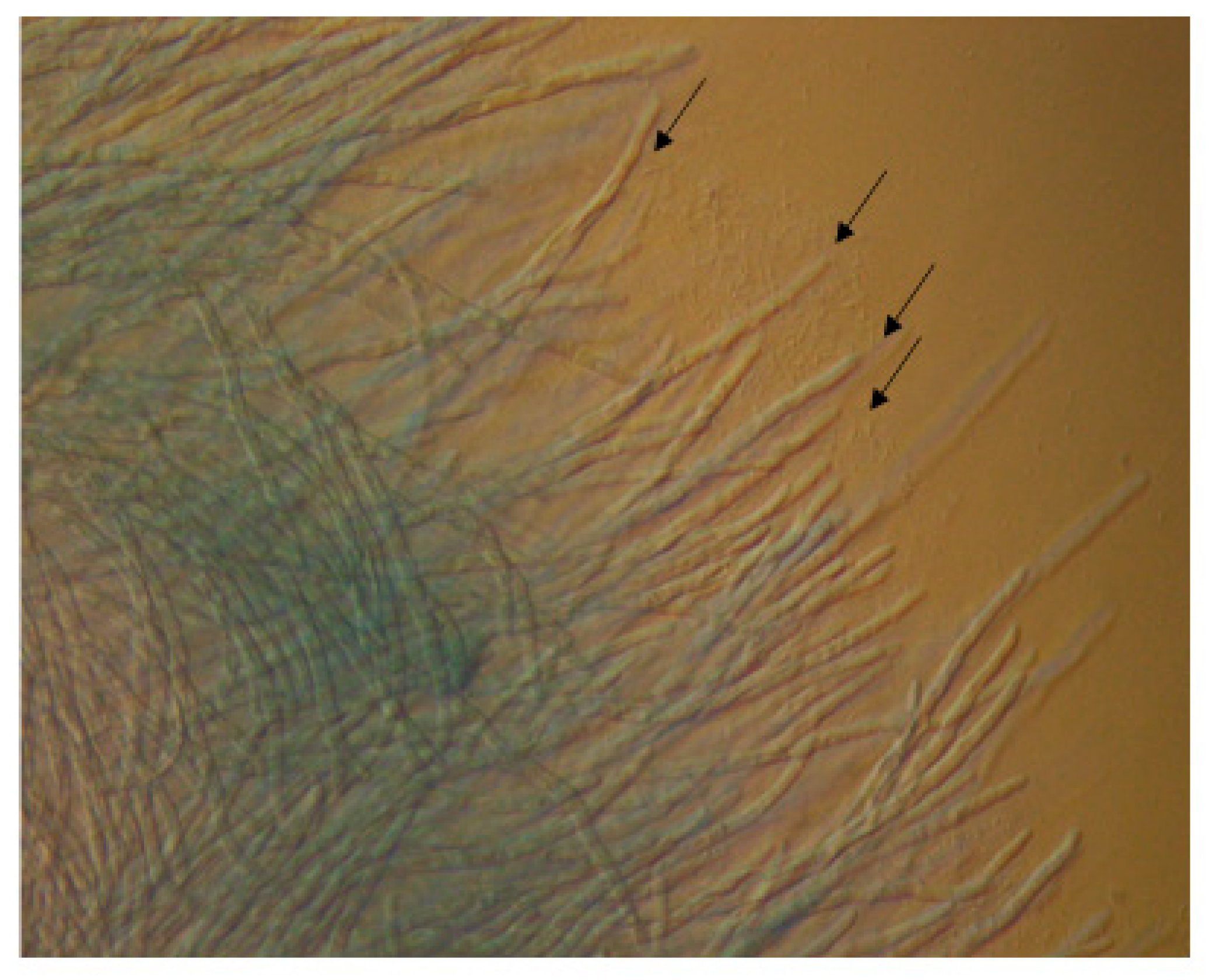
Water sources and water-related devices are often contaminated with pathogens responsible for healthcare-associated infections, including P. aeruginosa[46–48]. This may occur when microorganisms survive treatment protocols or via endpoint contamination.
What are the precautions for Pseudomonas?
Patients and caregivers should:keep their hands clean to avoid getting sick and spreading germs that can cause infections. ... remind healthcare providers and caregivers to clean their hands before touching the patient or handling medical devices.allow healthcare staff to clean their room daily when in a healthcare setting.
How is Pseudomonas transmitted?
Causes and Risk Factors of Pseudomonas Aeruginosa aeruginosa is spread through improper hygiene, such as from the unclean hands of healthcare workers, or via contaminated medical equipment that wasn't fully sterilized. Common hospital-associated P.
Does Pseudomonas aeruginosa need to be isolated?
Although it is generally accepted that patients with MDR P. aeruginosa should be isolated with contact precautions, the duration of contact precautions and the means of surveillance is not well-defined.
Is Pseudomonas a superbug?
The superbug Pseudomonas aeruginosa, which can cause lung infections in people on ventilators in Intensive Care Units.
Who is at risk for Pseudomonas aeruginosa?
MRSAPseudomonasOther factors that should raise suspicion for infection¶ImmunosuppressionImmunosuppressionRisk factors for MRSA colonization, including: End-stage kidney disease Crowded living conditions (eg, incarceration)Δ Injection drug useΔ Contact sports participationΔ Men who have sex with menΔ8 more rows
How serious is pseudomonas infection?
For many people, a Pseudomonas infection will only cause mild symptoms. However, if a person is in a hospital or has a weakened immune system, the threat becomes very severe. In these situations, a Pseudomonas infection can be life-threatening.
Can Pseudomonas cause sepsis?
Sepsis is a leading cause of mortality in burn patients. One of the major causes of sepsis in burn patients is Pseudomonas aeruginosa.
What are contact precautions?
Contact precautions are used when a person has a type of bacteria or virus on the skin or in a sore, or elsewhere in the body, such as the intestine, that can be transmitted to someone else if that person touches the infected individual or contaminated surfaces or equipment near the infected individual.
How do you get Pseudomonas in your eye?
It is widely known that pseudomonas keratitis is strongly associated with contact lens wear. In one study, incidence of pseudomonas keratitis was 2.76 cases per 10000 individuals per year, but rose to 13.04 cases per 10000 individuals when only considering contact lens wearers.
How do you treat Pseudomonas in wounds?
Topically applied dilute acetic acid, which is cheap and easily available, has been found to be effective in such chronic wounds. In the present study, an attempt has been made to use 1% acetic acid as the sole antimicrobial agent for the treatment of pseudomonal wound infections.
Can Pseudomonas cause conjunctivitis?
Pseudomonas aeruginosa conjunctivitis can rapidly progress to infection of the entire eye and may result in poor vision or blindness. The infection begins as a purulent conjunctivitis followed by infiltration of the corneal epithelium.
What is Pseudomonas ear infection?
Abstract. Pseudomonas aeruginosa commonly causes low-grade infections of the external auditory canal. If these infections are inadequately treated, they can progress into a severe form of external otitis called malignant external otitis (MEO).
What to do after pseudomonas surgery?
After surgery, be on the lookout for signs of infection . If you run a fever, have pain or see redness or discharge at your surgery site, call your doctor right away. Pseudomonas Infection Outlook. In most cases, antibiotics can clear the infection, but it’s important to follow your doctor’s instructions and focus on prevention.
What happens if you don't wash your hands?
If health care workers don’t wash their hands well, they can also transfer the bacteria from an infected patient to you. Your risk of pseudomonas infection also goes up if you: Have a wound from surgery. Are being treated for burns. Use a breathing machine, catheter, or other medical device.
What is the name of the bacteria that causes pseudomoonas?
Pseudomonas infections are infections caused by a kind of bacteria called Pseudomonas that’s commonly found in soil, water, and plants. The type that typically causes infections in people is called Pseudomonas aeruginosa. Some healthy people even have strains of it growing on their skin in moist parts of their body, ...
How to tell if you have a syringe?
Places where infection occurs -- and their signs -- may include: 1 Ears: pain and discharge 2 Skin: rash, which can include pimples filled with pus 3 Eyes: pain, redness, swelling 4 Bones or joints: joint pain and swelling; neck or back pain that lasts weeks 5 Wounds: green pus or discharge that may have a fruity smell 6 Digestive tract: headache, diarrhea 7 Lungs: pneumonia; severe coughing and congestion 8 Urinary: urinary tract infections
What are the signs of Pseudomonas?
Pseudomonas can infect any part of your body, such as your blood, lungs, stomach, urinary tract, or tendons. Pressure sores, wounds, and burns can also become infected. Places where infection occurs -- and their signs -- may include: Ears: pain and discharge. Skin: rash, which can include pimples filled with pus.
Can pseudomonas grow on fruits?
Pseudomonas Infection Causes and Risk Factors. You can get pseudomonas in many different ways. It can grow on fruits and vegetables, so you could get sick from eating contaminated food. It also thrives in moist areas like pools, hot tubs, bathrooms, kitchens, and sinks. The most severe infections occur in hospitals.
Can pseudomonas cause a rash?
If you’re in good health, you could come into contact with pseudomonas and not get sick. Other people only get a mild skin rash or an ear or eye infection. But if you’re sick or your immune system is already weakened, pseudomonas can cause a severe infection. In some cases, it can be life-threatening.
General Information
Pseudomonas [sodo−moh−nas] is a Gram-negative bacterium (bacillus) that can cause different types of healthcare-associated infections. The most common species, Pseudomonas aeruginosa, is commonly found in soil and ground water.
Transmission
In healthcare settings, Pseudomonas may spread through person-to-person contact. This may occur via the contaminated hands of healthcare personnel, or through direct contact with contaminated environmental surfaces or equipment.
Prevention
To prevent spreading Pseudomonas infections between patients, healthcare personnel must follow specific infection control precautions. These precautions may include strict adherence to hand hygiene and wearing gowns and gloves when they enter rooms where patients infected with Pseudomonas are staying.
Treatment
Pseudomonas infections that are not drug-resistant can be treated with antibiotics. Infections caused by MDR Pseudomonas can be very challenging. Therapeutic options are limited which may lead to prolonged hospitalization and even death.
Is P. aeruginosa a cause of nosocomial infections?
P. aeruginosa is a major cause of nosocomial infections that affects all patient populations and contributes significantly to morbidity and mortality. Antimicrobial resistance including carbapenem- and multidrug-resistance (MDR) is increasing. Colonization usually precedes manifest clinical infection. P. aeruginosa has been found to be an independent predictor of mortality in some studies of nosocomial bloodstream infection.
Is Pseudomonas aeruginosa a nosocomial path
Pseudomonas aeruginosa is an important nosocomial pathogen that causes serious nosocomial infections and contributes significantly to morbidity and mortality. Antimicrobial resistance including carbapenem- and multidrug-resistance (MDR) also continues to increase, further limiting therapeutic options.
When should isolation precautions be used?
Isolation precautions should be used for patients who are either known or suspected to have an infectious disease, are colonised or infected with a multi-resistant organism or who are particularly susceptible to infection.
How to achieve source isolation?
Source isolation can be achieved by nursing the patient in a single room or a negative pressure isolation room/unit with an ensuite toilet. Inclusion of a ventilation system distinguishes an isolation room from a single room.
Where is isolation carried out?
Isolation is usually carried out in a single (preferably en-suite) room with hand washing facilities and with the door kept closed. Occasionally cohort nursing (placing the patient in a room/bay area with other patients who are infected or colonised with the same microorganism), may be considered.
Should patients be in isolation?
Patients should remain in isolation whilst they remain symptomatic; a risk assessment should be undertaken to ascertain if and when isolation precautions can be relaxed. It is the responsibility of ALL members of staff to comply with isolation and Infection Control procedures.
How long does it take for scabs to separate after a scab?
Until all scabs have crusted and separated (3-4 weeks). Non-vaccinated HCWs should not provide care when immune HCWs are available; N95 or higher respiratory protection for susceptible and successfully vaccinated individuals; postexposure vaccine within 4 days of exposure protective [108, 129, 1038-1040].
What is pneumonia standard?
Pneumonia. Standard. n/a. Not transmitted from person to person except under extraordinary circumstances, (e.g., inhalation of aerosolized tissue phase endospores during necropsy, transplantation of infected lung) because the infectious arthroconidial form of Coccidioides immitis is not produced in humans [1054, 1055].
What is the CDC's guidance for isolation?
To assist hospitals in maintaining up-to-date isolation practices, the Centers for Disease Control and Prevention (CDC) and the Hospital Infection Control Practices Advisory Committee (1) (HICPAC) have revised the "CDC Guideline for Isolation Precautions in Hospitals." HICPAC was established in 1991 to provide advice and guidance to the Secretary, Department of Health and Human Services (DHHS); the Assistant Secretary for Health, DHHS; the Director, CDC; and the Director, National Center for Infectious Diseases, regarding the practice of hospital infection control and strategies for surveillance, prevention, and control of nosocomial infections in US hospitals. HICPAC also advises the CDC on periodic updating of guidelines and other policy statements regarding prevention of nosocomial infections.
What was the problem in hospitals in 1980?
By 1980, hospitals were experiencing new endemic and epidemic nosocomial infection problems, some caused by multidrug-resistant microorganisms and others caused by newly recognized pathogens, which required different isolation precautions from those specified by any existing isolation category.
Why is it important to have a private room?
A private room is important to prevent direct- or indirect-contact transmission when the source patient has poor hygienic habits, contaminates the environment , or cannot be expected to assist in maintaining infection control precautions to limit transmission of microorganisms (ie, infants, children, and patients with altered mental status). When possible, a patient with highly transmissible or epidemiologically important microorganisms is placed in a private room with handwashing and toilet facilities, to reduce opportunities for transmission of microorganisms.
How did infectious disease hospitals combat nosocomial transmission?
Personnel in infectious disease hospitals began to combat problems of nosocomial transmission by setting aside a floor or ward for patients with similar diseases (6) and by practicing aseptic procedures recommended in nursing textbooks published from 1890 to 1900. (5)
Why is handwashing important?
Handwashing frequently is called the single most important measure to reduce the risks of transmitting microorganisms from one person to another or from one site to another on the same patient. The scientific rationale, indications, methods, and products for handwashing have been delineated in other publications. (64-72)
What are the main features of Standard Precautions?
Standard Precautions synthesize the major features of Universal (Blood and Body Fluid) Precautions (designed to reduce the risk of transmission of bloodborne pathogens) and Body Substance Isolation (designed to reduce the risk of transmission of pathogens from moist body substances).
Why do hospitals wear masks?
The wearing of masks, eye protection, and face shields in specified circumstances to reduce the risk of exposures to bloodborne pathogens is mandated by the OSHA bloodborne pathogens final rule. (51) A surgical mask generally is worn by hospital personnel to provide protection against spread of infectious large-particle droplets that are transmitted by close contact and generally travel only short distances (up to 3 ft) from infected patients who are coughing or sneezing.
