As a review, microvascular complications of diabetes, which affect small blood vessels, are known to lead to diabetic eye disease, kidney disease, and neuropathy; optimal management is proven to reduce complications in hallmark studies.
What are the risks and complications of diabetes?
Complications and manifestations of diabetes. Individuals with diabetes are also at greater risk of developing cardiovascular diseases such as heart attack, stroke, or circulatory problems in the legs and feet (peripheral artery disease). These complications of diabetes are typically called "macrovascular" complications, which mean that these complications affect the larger blood vessels.
What are the main complications of diabetes?
Diabetes-related complications can include damage to: the large blood vessels (macrovascular/ cardiovascular complications), leading to heart attack, stroke or circulation problems in the lower limbs. the small blood vessels (microvascular complications), causing problems in the eyes, kidneys, feet and nerves.
What can people with diabetes do to avoid complications?
Your diabetes management plan will cover how to:
- Track your glucose levels. Very high glucose levels (called hyperglycemia) or very low glucose levels (called hypoglycemia) can be risky to your health. ...
- Make healthy food choices. The food you eat affects glucose levels, so it’s important to learn what’s best for you to eat, how much, and when. ...
- Be active. ...
- Take your medicines. ...
What are the long - term effects of diabetes?
People with diabetes have a greater risk of developing eye problems, including:
- Cataracts: A cataract is a thickening and clouding of the lens of the eye. ...
- Retinopathy: Another eye problem, called diabetic retinopathy, involves changes in the retina, the light-sensitive layer at the back of the eye. ...
- Glaucoma: People who have diabetes also have a greater chance of getting glaucoma. ...
What are microvascular and macrovascular complications of diabetes?
Generally, the injurious effects of hyperglycemia are separated into macrovascular complications (coronary artery disease, peripheral arterial disease, and stroke) and microvascular complications (diabetic nephropathy,neuropathy, and retinopathy).
What complication of diabetes is considered macrovascular?
Results: Macrovascular complications of T2DM include coronary heart disease, cardiomyopathy, arrhythmias and sudden death, cerebrovascular disease and peripheral artery disease. Cardiovascular disease is the primary cause of death in diabetic patients.
What is the difference between macrovascular and microvascular complications?
Definitions. Macrovascular complications of T2DM refer to atherosclerosis affecting the aorta, coronary artery, basilar artery, or renal artery. Microvascular complications of T2DM refer to microcirculation abnormalities. Microvascular lesions mainly manifest in the retina, kidney, and nervous tissue.
Is stroke a microvascular complication of diabetes?
Traditionally, retinopathy, neuropathy, and nephropathy have been designated microvascular complications of DM, and stroke, myocardial infarction and gangrene are termed macrovascular complications.
What are the macrovascular complications of diabetes and how do they develop?
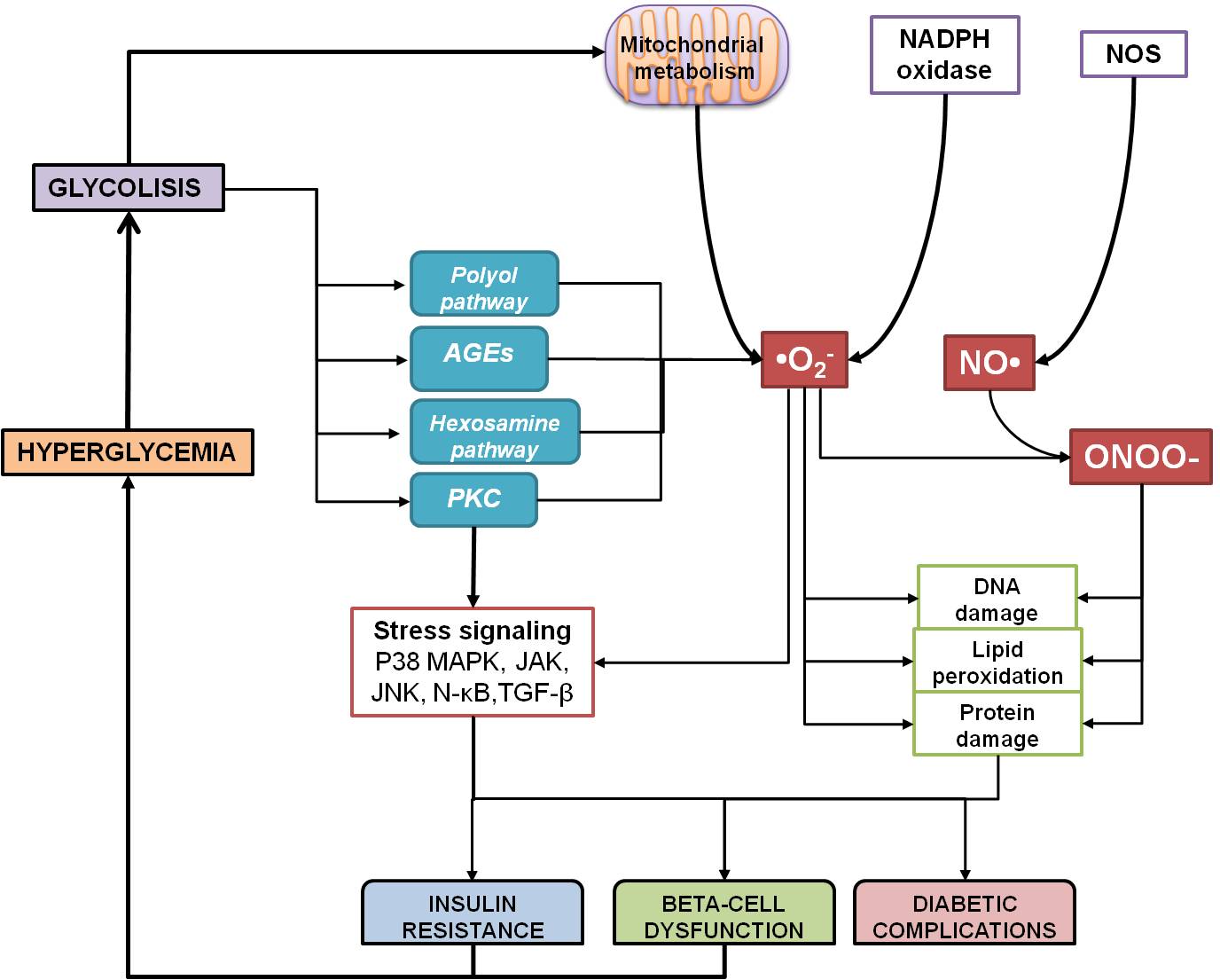
Macrovascular. The macrovascular complications of diabetes result from hyperglycemia, excess free fatty acid, and insulin resistance. These cause increased oxidative stress, protein kinase activation, and activation of the receptor for advanced glycation end products, factors that act on the endothelium.
What are macrovascular diseases?
Macrovascular disease: Disease of the large blood vessels, including the coronary arteries, the aorta, and the sizable arteries in the brain and in the limbs. Macrovascular disease is by contrast to microvascular disease.
What are the complications of diabetes?
Common diabetes health complications include heart disease, chronic kidney disease, nerve damage, and other problems with feet, oral health, vision, hearing, and mental health. Learn how to prevent or delay these diabetes complications and how to improve overall health.
What are complications of diabetes mellitus?
What are the major complications of diabetes?Eye problems (retinopathy) ... Diabetes foot problems are serious and can lead to amputation if untreated. ... Heart attack and stroke. ... Kidney problems (nephropathy) ... Nerve damage (neuropathy) ... Gum disease and other mouth problems. ... Related conditions, like cancer.More items...
Diabetic retinopathy
Diabetic retinopathy may be the most common microvascular complication of diabetes. It is responsible for ∼ 10,000 new cases of blindness every year in the United States alone. 1 The risk of developing diabetic retinopathy or other microvascular complications of diabetes depends on both the duration and the severity of hyperglycemia.
Diabetic nephropathy
Diabetic nephropathy is the leading cause of renal failure in the United States. It is defined by proteinuria > 500 mg in 24 hours in the setting of diabetes, but this is preceded by lower degrees of proteinuria, or“microalbuminuria.” Microalbuminuria is defined as albumin excretion of 30-299 mg/24 hours.
Diabetic neuropathy
Diabetic neuropathy is recognized by the American Diabetes Association (ADA) as “the presence of symptoms and/or signs of peripheral nerve dysfunction in people with diabetes after the exclusion of other causes.” 15 As with other microvascular complications, risk of developing diabetic neuropathy is proportional to both the magnitude and duration of hyperglycemia, and some individuals may possess genetic attributes that affect their predisposition to developing such complications..
Macrovascular Complications of Diabetes
The central pathological mechanism in macrovascular disease is the process of atherosclerosis, which leads to narrowing of arterial walls throughout the body. Atherosclerosis is thought to result from chronic inflammation and injury to the arterial wall in the peripheral or coronary vascular system.
Practice Recommendations
Patients with type 1 diabetes of > 5 years' duration should have annual screening for microalbuminuria, and all patients with type 2 diabetes should undergo such screening at the time of diagnosis and yearly thereafter. All patients with diabetes should have serum creatinine measurement performed annually.
What is the soluble receptor for advanced glycation end product (SRAGE)?
Serum soluble receptor for advanced glycation end product (sRAGE) may reflect the activity of the advanced glycation end product (AGE)–receptor for advanced glycation end product (RAGE) axis, which has been proposed as a potential mechanism linking hyperglycaemia to vascular complications in diabetes. We have investigated whether serum AGEs, sRAGE and pentosidine levels were increased and correlated with microvascular complications in type 2 diabetes mellitus (DM). We included 30 healthy control subjects, and 200 diabetic patients were divided into two subgroups: 100 patients with diabetic retinopathy and 100 patients with diabetic nephropathy. AGEs, sRAGE and pentosidine were measured in serum by enzyme-linked immunosorbent assay (ELISA). Serum AGEs, sRAGE and pentosidine levels were significantly increased in diabetic patients with retinopathy and in diabetic patients with nephropathy compared to control subjects (p < 0.001). Serum AGEs, sRAGE and pentosidine levels are positively associated with microvascular complications in type 2 DM. Multiple regression analysis reveals serum pentosidine as an independent determinant of the presence of diabetic retinopathy (p = 0.004) and the presence of hypertension (p = 0.018) and hyperlipidaemia (p = 0.036). Pentosidine levels may be a biomarker for microvascular complications in type 2 diabetic patients. Continue reading >>
What is a diabetic ketoacidosis?
4.1. Diabetic Ketoacidosis (DKA) Diabetic ketoacidosis results from lack of insulin and it is considered a medical emergency as it has a mortality rate of approximately 5 percent, mostly because of late recognition and frequently suboptimal management. Diabetic ketoacidosis can be the first manifestation of type 1 diabetes in a previously undiagnosed patient or can occur in a patient with type 1 diabetes when insulin requirements rise during medical stress. Noncompliance with insulin administration is another common cause of DKA. Although DKA is much more common in type 1 diabetes, it can also occur in patients with type 2 diabetes who have a predominant insulin secretory defect under severe medical stress. 4.1.1. Pathophysiology Diabetes is often referred to as "starvation in the midst of plenty" and the progression of events that results from acute insulin deficiency holds this concept to be valid. Insulin deficiency leads to impaired peripheral glucose uptake. In the presence of inadequate insulin, energy stores in fat and muscle are rapidly broken down into fatty acids and amino acids, which are then transported to the liver for conversion to glucose and ketones (beta-hydroxybutyrate and acetoacetate). Counter-regulatory hormones such as glucagon, catecholamines, cortisol and growth hormone rise in an attempt to correct the perceived low glucose levels, further contributing to hyperglycemia and ketonemia. The combination of increased production of glucose and ketones with decreased utilization (due to insulin deficiency) results in high levels of these substances. Hyperglycemia causes osmotic diuresis with an ensuing reduction of intravascular volume, which in turn causes an impairment of renal blood flow and an inability to excrete glucose which worsens the hypergl Continue reading >>
Why is the number of people with diabetes mellitus increasing?
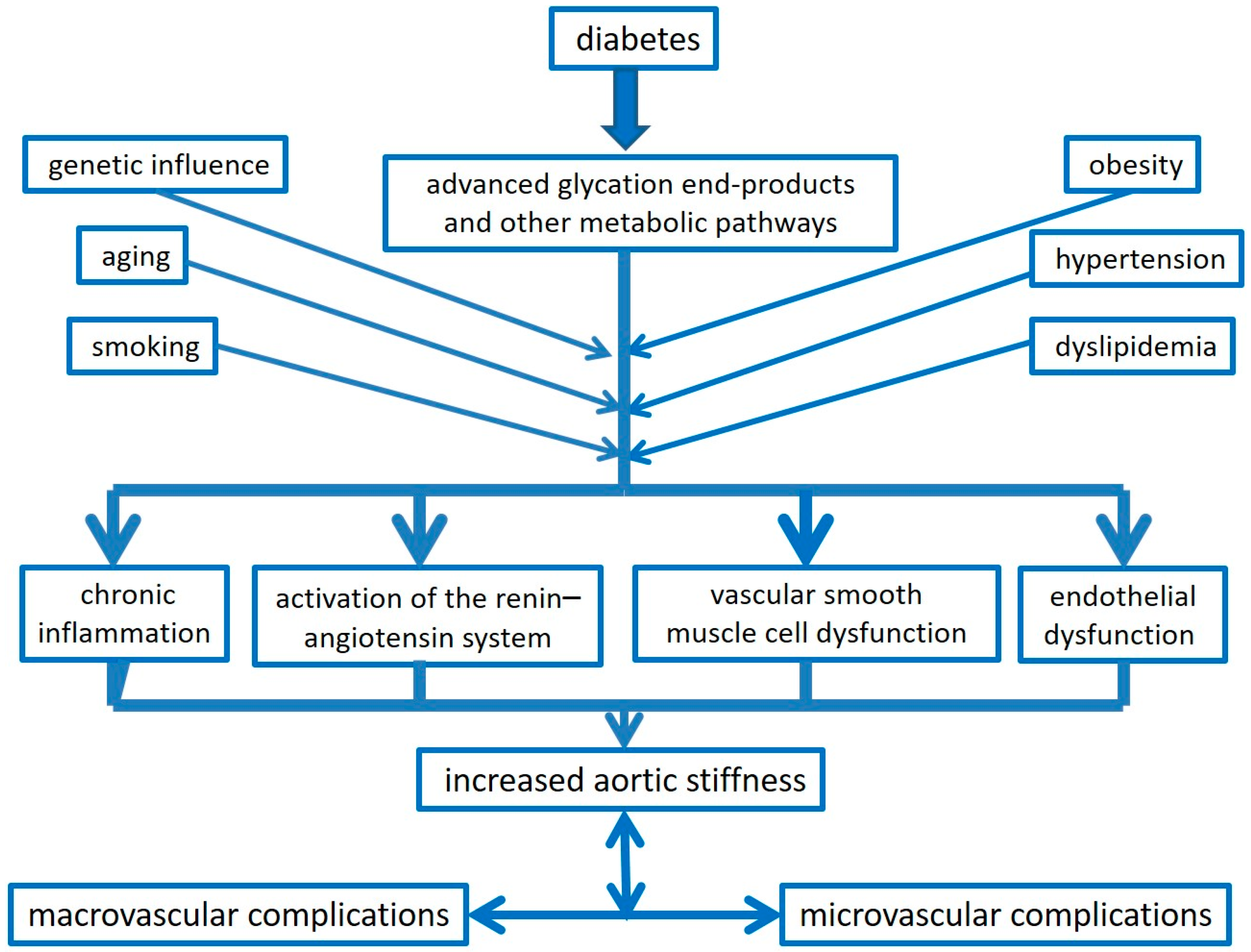
The number of people with diabetes mellitus is alarmingly increasing due to the growing prevalence of obesity, genetic susceptibility, urbanization, and ageing.1,2 Type 2 diabetes, the most common form of the disease, may remain undetected for many years and its diagnosis is often made incidentally through an abnormal blood or urine glucose test. Hence, physicians often face this disease at an advanced stage when vascular complications have already occurred in most of patients. Macrovascular complications are mainly represented by atherosclerotic disease and its sequelae. Diabetes-related microvascular disease such as retinopathy and nephropathy are major causes of blindness and renal insufficiency.1 Based on this scenario, a better understanding of the mechanisms underlying diabetic vascular disease is mandatory because it may provide novel approaches to prevent or delay the development of its complications. This review will focus on the most current advances in the pathophysiology of vascular disease (Part I) and will address clinical manifestations and management strategies of patients with diabetes (Part II). The alterations in vascular homeostasis due to endothelial and smooth muscle cell dysfunction are the main features of diabetic vasculopathy favouring a pro-inflammatory/thrombotic state which ultimately leads to atherothrombosis. Macro- and microvascular diabetic complications are mainly due to prolonged exposure to hyperglycemia clustering with other risk factors such as arterial hypertension, dyslipidemia as well as genetic susceptibility.3 Interestingly, nephropathy, retinopathy, and diabetic vascular disease are in line with the notion that endothelial, mesangial, and retinal cells are all equipped to handle high sugar levels when compared with other cell Continue reading >>
What is the primary cause of death in diabetics?
Whether type I or type II, this disease has serious macro- and microvascular complications that constitute the primary cause of death in diabetic patients.
What is DM in medical terms?
Go to: Diabetes mellitus (DM) has routinely been described as a metabolic disorder characterized by hyperglycemia that develops as a consequence of defects in insulin secretion, insulin action, or both. Type 2 diabetes encompasses individuals who have insulin resistance (IR) and usually relative (rather than absolute) insulin deficiency. [1] The pathologic hallmark of DM involves the vasculature leading to both microvascular and macrovascular complications. [2] Chronicity of hyperglycemia is associated with long-term damage and failure of various organ systems mainly affecting the eyes, nerves, kidneys, and the heart. [1] According to diabetes atlas (7th edition), the global prevalence of diabetes is estimated at 415 million (8.8%), which is predicted to rise to 642 million in next 25 years. [3] In India, there are about 69.2 million people with diabetes and are expected to cross 123.5 million by 2040. [3] Moreover, worldwide approximately 193 million diabetics remain undiagnosed predisposing them to the development of several long-term complications of untreated chronic hyperglycemia. [3] Although intensive glycemic control lowers the incidence and progression of microvascular complications, the morbidity associated with these complications is still increasing. [4] Several landmark studies such as the United Kingdom Prospective Diabetes Study (UKPDS) have demonstrated that strict glycemic control does limit microvascular disease while attempts to improve macrovascular outcomes through glucose-lowering interventions still remain shrouded with controversy. A relative risk (RR) reduction in myocardial infarction (MI) (P = 0.052) has been observed in the 10 years of posttrial follow-up of UKPDS. [5] Similarly, the risk of cardiovascular mortality, nonfatal MI and stroke reduced wi Continue reading >>
What is a DKA in dogs?
Diabetes Complications in Dogs and Cats: Diabetes Ketoacidosis (DKA) Association of Glycemic Variability in Type 1 Diabetes With Progression of Microvascular Outcomes in the Diabetes Control and Complications Trial.
What is the fourth theory of diabetes?
Fourth theory In diabetes glucose is converted into sorbitol which is a tissue toxin. Q Enzyme required in this step is aldose reductase. Q Recently a new drug Epalrestat (PNQ) Q has been launched which is a aldose reductase inhibitor. (PNQ) Which is supposed to reduce the complication of diabetes.
What is the major cause of morbidity and mortality in patients with diabetes?
Late stages of macrovascular disease involve complete obstruction of these vessels, which can increase the risks of myocardial infarction (MI), stroke, claudication, and gangrene. Cardiovascular disease (CVD) is the major cause of morbidity and mortality in patients with diabetes. Back to Top.
What is the primary goal of diabetes management?
The management of type 1 and 2 diabetes mellitus (DM) requires addressing multiple goals, with the primary goal being glycemic control. Maintaining glycemic control in patients with diabetes prevents many of the microvascular and macrovascular complications associated with diabetes. This chapter presents a review of the prevalence, screening, diagnosis, and management of these complications.
How long does DM last?
Retinopathy. In patients with type 1 DM, 13% have retinopathy at 5 years and 90% have retinopathy after 10 to 15 years; approximately 25% will develop proliferative retinopathy after 15 years. [1]
What is the earliest manifestation of diabetic retinopathy?
Retinopathy. Microaneurysm formation is the earliest manifestation of diabetic retinopathy. Microaneurysms may form due to the release of vasoproliferative factors, weakness in the capillary wall, or increased intra-luminal pressures. Microaneurysms can cause vascular permeability in the macula, which can lead to macular edema that threatens central vision. Obliteration of retinal capillaries can lead to intraretinal microvascular abnormalities. As capillary closure becomes extensive, intraretinal hemorrhages develop.
Can diabetic retinopathy be detected with ophthalmoscopy?
Handheld ophthalmoscopy may be able to detect diabetic retinopathy, but it offers limited view of the retina and has difficulty detecting diabetic macular edema, a significant cause of vision loss in diabetes. Retinopathy is easier to detect with binocular vision. In difficult cases, IV fluorescein angiography and confocal microscopy are used. Technology is available for screening with fundus photographs obtained in the practitioner's office and then read by an expert. However, these do not show a complete view of the retina and do not include other aspects of the eye examination, such as eye pressure, and, thus, cannot replace yearly eye evaluations.
Can you see the bottom of your feet with diabetes?
Patients who have difficulty examining their feet should seek assistance, especially if they have impaired vision. The use of a mirror can help patients see the bottoms of their feet (see the chapter, " Prevention and Treatment of Leg and Foot Ulcers in Diabetes Mellitus ").
Can vitreous humor cause retinal detachment?
These vessels are very friable and can lead to vitreous hemorrhages. The vitreous humor can contract and lead to retinal detachment. Nephropathy.
What are the complications of diabetes?
In diabetes (DM), chronic complications related to the direct or indirect effects of prolonged hyperglycemia on the vasculature have been classified into macrovascular and microvascular complications, depending on the size of affected vessels and the pathophysiological mechanisms involved. Microvascular disease includes retinopathy, nephropathy and neuropathy.
What is DR in diabetes?
Diabetic retinopathy (DR) is a chronic complication associated with long DM duration and poor glycemic control, the overall incidence of DR and of vision-threatening forms of DR (VTDR) being higher in T1DM than in T2DM [ 8 ]. The United Kingdom Prospective Diabetes Study (UKPDS) showed that both the incidence and progression of DR correlate with elevated HbA 1c, emphasizing the importance of good glycemic control to prevent visual impairment [ 9 ]. Every 1% decrease in HbA 1c leads to a 40% reduction in the risk of developing retinopathy, a 25% reduction in the risk of progression to vision-threatening retinopathy, and a 15% reduction in the risk of blindness [ 10 ].
Which area of the retina is affected by thrombosis?
The first areas affected by thrombosis and ischemia are in the middle retinal periphery, and the answer is to release a range of mediators, of which the key role is played by VEGF, which promotes retinal neovascularization and interruption of blood flow in many areas (optical disc, macula, iridocorneal angle and iris). The response to retinal hypoperfusion, a maladaptive protective mechanism, leads to the appearance of fragile new vessels, prone to repeated bleeding and leakage, ultimately destroying normal retinal architecture ( Figure 1 ).