What are the three phases of inflammation?
inflammation Upvote10Downvote0ShareAnswer itThe are three main stages inflammation which can each vary intensity and duration Acute swelling stage.Sub acute regenerative stage.Chronic scar tissue maturation and remodelling stage.In this manner, what happens during the inflammatory...
What are the steps of inflammation?
Steps in the process of inflammation. Inflammatory response. 1.Tissue damage caused by bacterial infection or injury. 2.Release of vasodilators and chemotactic factors like histamine. 3. This lead to increased capillary permeability and blood flow to the area. 4. Margination followed by migration of phagocytes to the site of infection.
What are the three phases of the inflammatory response?
What is inflammation and the steps in the process of inflammation?
- Rubor (redness) due to capillary dilation resulting increased blood flow
- Tumor (swelling) due to passage of plasma from the blood stream to the damaged site
- Calor (heat) due to capillary dilation resulting increased blood flow
- Dolor (pain) mainly due to destruction of tissue
What are the steps of the inflammatory process?
- activation of vascular endothelium.
- vasodilation.
- fever production.
- migration of immune system cells into the area.
- activation and cytokine release by neutrophils.
- phagocytosis and methods of target destruction.
- the acute phase response.
- clotting cascade.
What are the 5 steps of the inflammatory response?
Five cardinal signs characterize this response: pain, heat, redness, swelling, and loss of function.
What are the two phases of inflammatory response?
Phases of Acute Inflammation. Acute inflammation can be discussed in terms of two stages; (1) the vascular phase, which is followed by; (2) the cellular phase.
What are the 3 main events in the inflammatory response?
Important microcirculatory events that occur during the inflammatory process include vascular permeability changes, leukocyte recruitment and accumulation, and inflammatory mediator release [2, 6].
What are the steps in the inflammatory process quizlet?
pain. localized heat. swelling. redness. loss of function.
What is the first stage of the inflammatory response?
Inflammatory Response: Acute swelling stage (Phase 1) It is characterized by the classical signs of pain, heat, redness, and swelling. Inflammation is a key part of the body's defense system, an indispensable protective response by the body's system of self-defense.
What is the first step in the events of the inflammatory process?
The response to ICH occurs in four distinct phases: (1) initial tissue damage and local activation of inflammatory factors, (2) inflammation-driven breakdown of the blood–brain barrier, (3) recruitment of circulating inflammatory cells and subsequent secondary immunopathology, and (4) engagement of tissue repair ...
What is the cellular phase of inflammation?
The most important feature of inflammation is the accumulation of white blood cells at the site of injury. Most of these cells are phagocytes, certain “cell-eating” leukocytes that ingest bacteria and other foreign particles and also clean up cellular debris caused by the injury.
What are the 4 signs of inflammation?
This type of stimulation–response activity generates some of the most dramatic aspects of inflammation, with large amounts of cytokine production, the activation of many cell types, and in fact the four cardinal signs of inflammation: heat, pain, redness, and swelling (1).
What is the last step in the inflammatory process?
During the last phase of the healing, inflammation signs start to subside. The four cardinal signs are no longer visible. It is during the remodeling phase that collagen tissue fibers reorganize themselves. This happens to support the tissues better.
What is mechanism of inflammation?
MECHANISMS OF INFLAMMATION. Inflammation consists of a tightly regulated cascade of immunological, physiological, and behavioral processes that are orchestrated by soluble immune signaling molecules called cytokines. The first step of the inflammatory cascade involves recognition of infection or damage (Figure 1b).
What is the main cause of inflammation in the body?
Possible Causes The most common reasons for chronic inflammation include: Autoimmune disorders, such as lupus, where your body attacks healthy tissue. Exposure to toxins, like pollution or industrial chemicals. Untreated acute inflammation, such as from an infection or injury.
What is the cellular phase of inflammation?
The cellular phase of the inflammatory reaction is characterized by the arrival to the site of inflammation of leukocytes circulating in the blood.
What is the last stage of the inflammatory response?
During the last phase of the healing, inflammation signs start to subside. The four cardinal signs are no longer visible. It is during the remodeling phase that collagen tissue fibers reorganize themselves. This happens to support the tissues better.
What is inflammatory phase of wound healing?
Inflammation. Inflammation, the next stage of wound healing occurs within the first 24 hours after injury and can last for up to 2 weeks in normal wounds and significantly longer in chronic non-healing wounds (Figure 23.3).
What are the functions of the inflammatory response?
The goals of the inflammatory response are to: Prevent initial establishment of infection or remove damaged tissue. Prevent the spread of infection or repair damaged tissue. Recruit effector cells if the immune cells of the innate immune system cannot control infection or repair damaged tissue.
How long does the second phase of collagen formation last?
Thus, the new tissue is weak and susceptible to disruption by overly aggressive activity. This phase lasts from 2 days to 8 weeks.
What is inflammation in Pilates?
Written by Christina Eng – Physiotherapist, Clinical Pilates Instructor. Inflammation is the body’s response to injury. Injury to soft tissues can arise from a number of sources. Physical traumas such as a strain, sprain or contusion are most common, whereas injuries can also occur from bacterial or viral infections, heat, or chemical injury.
What is the purpose of phase 1?
The purpose of vascular changes is to increase blood flow to the local area, mobilize and transport cells to the area to initiate healing.
Why is tension important in collagen?
Tension becomes important because new collagen must orient along the lines of stress to best accommodate the loads required for function.
How long does a swollen thigh last?
This phase lasts from 2 days to 8 weeks. Signs and Symptoms: Less warmth and swelling, palpable tenderness decreases, pain felt with tissue resistance or stretch of the tissue. As healing progresses, the tissue continues to remodel, strengthen and improve its cellular organization.
What happens to the brain after hemorrhage?
Upon hemorrhage, iron, in the form of the cofactor heme, is released from the peripheral blood into the brain parenchyma.26Heme is broken down into free iron and bilirubin by heme oxygenases (HO) expressed in neurons, astrocytes, and microglia.24,38,39The subsequent release of free iron acts as a potent oxidative insult,17and markers of oxidative stress neurons have been observed in many studies of ICH.17,24,25,40The exact role of HO enzymes in ICH pathology remains controversial, with some studies finding that HO-1-or HO-2-deficient mice have decreased neurologic deficits and edema,25,39whereas others have reported that HO-1 and HO-2 protect against neuronal death by sequestering free iron within microglia and astrocytes.38,41The deleterious effect of free iron is better supported in experimental models, as treatment with the iron chelator deferoxamine decreased white matter loss and ameliorated the neurologic deficits in experimental models of ICH.9,42,43Notably, the protective effect of deferoxamine was most potent when administered within 2 to 4 hours after hemorrhage, and treatment > 24 hours post-ICH had no significant effect on subsequent inflammation and behavioral outcomes,44,45supporting the role of blood-derived free iron in the earliest stages of the inflammatory response to ICH. Thus, early intervention to prevent oxidative stress induced by blood components is a promising target for therapeutic intervention; a clinical trial to assess the efficacy and safety of deferoxamine treatment for ICH is ongoing.46
What is thrombin released into the brain?
Thrombin is a critical serine protease in the coagulation cascade produced on the plasma membrane of platelets and leukocytes and released into the brain parenchyma early during ICH.16,18,26,47Beyond its role in driving the clotting of blood in the CNS after ICH, thrombin can bind directly to a family of protease-activated receptors (PARs), most notably PAR-1.48PAR-1 expression is increased in the brains of rats after ICH,48and thrombin contributes to the pathology of ICH by acting directly on PAR-1 expressing neurons and microglia.16Indeed, intracerebral injection of rat striata activated resident microglia and increased vascular permeability of the BBB.18,30PAR-1 signaling on neurons potentiates N-methyl-D-aspartate (NMDA) receptor activation of ion channels and can drive glutamate-mediated hypertoxicity and apoptosis.29,30,49,50Indeed, PAR-1-deficient mice have decreased neuronal death and smaller lesion size after ICH, an effect reversed by administration of an NMDA antagonist.49,51Thrombin also acts through PAR-1 to activate the transcription factor NF-κB (nuclear factor kappa-light-chain-enhancer of activated B cells) in microglia, resulting in production of the inflammatory cytokines tumor necrosis factor α (TNF-α) and interleukin 1 β (IL-1β).52,53
What is intracranial hemorrhage?
Intracerebral hemorrhage (ICH) is a major health concern, with high rates of mortality and morbidity and no highly effective clinical interventions. Basic research in animal models of ICH has provided insight into its complex pathology, in particular revealing the role of inflammation in driving neuronal death and neurologic deficits after hemorrhage. The response to ICH occurs in four distinct phases: (1) initial tissue damage and local activation of inflammatory factors, (2) inflammation-driven breakdown of the blood–brain barrier, (3) recruitment of circulating inflammatory cells and subsequent secondary immunopathology, and (4) engagement of tissue repair responses that promote tissue repair and restoration of neurologic function. The development of CNS inflammation occurs over many days after initial hemorrhage and thus may represent an ideal target for treatment of the disease, but further research is required to identify the mechanisms that promote engagement of inflammatory versus anti-inflammatory pathways. In this review, the authors examine how experimental models of ICH have uncovered critical mediators of pathology in each of the four stages of the inflammatory response, and focus on the role of the immune system in these processes.
What is the cause of death for an estimated 11% of deaths worldwide?
Keywords: intracerebral hemorrhage, stroke, neuroinflammation, neuroimmunology. Stroke is a major international health concern and the cause of death for an estimated 11% of deaths worldwide.1Intracerebral hemorrhage (ICH), while accounting for just 10 to 25% of total strokes, is responsible for greater than half of stroke-related deaths, ...
How long after ICH do hematomas die?
Hematoma size, neuron death, and inflammation peak between 1 and 3 days after ICH.6,7,13,101,108Notably, while at 72 hours post-ICH levels of IL-1β and IL-6 remain elevated, at this time point the presence of factors associated with inhibition of inflammation in the CNS, such as TGF-β and CXCL1, have increased.92,101By 7 days posthemorrhage, the hematoma has largely been cleared and inflammation has receded.6,7,101Additionally, expression of CD36, a scavenger receptor important for phagocytosis of apoptotic and necrotic cells, is increased on blood-derived macrophages and microglia at 3 and 7 days post-ICH.7,92,95CD36-deficient mice displayed increased hematoma volume 5 days post-ICH and had worse behavioral outcomes than wild-type controls,95indicating that CD36 may play an important role in hematoma clearance and recovery of neurologic function after ICH.
How does collagenase injection work?
The collagenase injection model, first developed in rats,11and then adapted for use in a wide range of species,8acts by dissolving the collagen-based periendothelial extracellular matrix resulting in rapid spontaneous hemorrhage of small blood vessels near the site of injection. Sham injections or injections of saline are common controls. This approach mimics some key elements of clinical ICH, including endothelial damage and continued bleeding/rebleeding. Additionally, it is highly reproducible and hematoma volume can be controlled by the dose of collagenase used.8,11However, this approach typically generates higher levels of inflammation than similar-sized hematomas in other models,12–14suggesting that collagenase may initiate inflammatory pathways independent of its effect on hemorrhage. This may be the result of trace bacterial contaminants in the collagenase capable of potently activating bacterial pattern recognition receptors, or simply the continued dissolution of basement membrane.
How long does it take for CNS inflammation to develop?
The development of CNS inflammation occurs over many days after initial hemorrhage and thus may represent an ideal target for treatment of the disease, but further research is required to identify the mechanisms that promote engagement of inflammatory versus anti-inflammatory pathways.
Stage 1: Slight Chronic Inflammation
Symptoms you may feel are: Fatigue, Insomnia, Brain Fog, “Aches and Pains”, Weight Change, Stress
Stage 2: Moderate Chronic Inflammation
Symptoms you may feel are: Bloating, Cramps, “IBS”, Recurrent infections (skin, respiratory tract), seasonal Allergies, slight “Allergies”, Eczema, Food intolerances and - “sensitivities”, forgetfulness, moodiness, feeling blue or down, confusion, unfocused
Stage 3: Severe Chronic Inflammation
Diagnosable diseases you may “have”: Severe Inflammation, Chronic Diseases (“of Aging??”), some Depressions and probably some other mental illnesses, Severe Allergies with anaphylaxis, Autoimmune diseases (Psoriasis, severe Eczema, M.
Stage 4: End-Stage Inflammation
What does that look like? End-stage Cancer, Severe Bone deformities, End-stage Heart failure, End-stage Dementia, Blindness, Amputations…
The Good News
Stages 1-3 are reversible if addressed properly. How can you do that? It can be complicated. At DocChristine, we use a comprehensive, root-cause approach, combined with testing and bio-individual nutrition and targeted supplementation.
What is inflammation?
Well, inflammation is the body’s protective response to harmful stimuli such as foreign invaders like bacteria and viruses, damaged cells such as from physical trauma, and irritants such as the capsaicin chemical inside hot chili peppers. Inflammation may also be triggered by allergies and certain foods that a person is allergic to.
What happens during inflammation?
Let’s outline the whole inflammatory process to really understand what happens during inflammation:
What is the term for white blood cells that start oozing out?
Leukocyte exudation or extravasation a.k.a. white blood cells start oozing out
How does inflammation occur?
Inflammation can by provoke by stimuli that damages the body or triggers off the immune system.
What causes inflammation in the body?
So to list them out, the causes of inflammation include: 1 Physical trauma; i.e. blows, crush, cuts 2 Exposure to excessive sunlight; UV rays damage skin cells in excess 3 X-rays and radiation damage cells including DNA 4 Chemicals that damage the body via corrosion 5 Extreme heat or cold 6 Infections by bacteria, viruses and parasites 7 Allergens or what the immune system treats as a foreign invader
Why is inflammation important?
Another function of inflammation is to prevent further damage to the affected part of the body. For example, let’s say a boy sprains his ankle. Very soon after, the boy’s ankle would immediately start getting inflamed and swollen, preventing further movement. This is actually good thing, as the swelling & inflammation stiffens the joint, and becomes painful to prevent further movement of the joint and to allow for proper healing.
Why is my inflamed area hotter?
By the way, the increased blood flow from the bigger blood vessel size is one of the reasons why the inflamed area becomes hotter and redder.
What is tissue damage caused by wound or invading pathogenic organisms?
Tissue damage caused by wound or invading pathogenic organisms induces a complex sequence of events collective ly known as inflammation. Inflammation if localised to the site of infection or injury. Once intruder is destroyed, inflammation settles down. 3.
What causes tissue damage?
1.Tissue damage caused by bacterial infection or injury. 2.Release of vasodilators and chemotactic factors like histamine. 3. This lead to increased capillary permeability and blood flow to the area. 4. Margination followed by migration of phagocytes to the site of infection. 5.The serum proteins along with phagocytes destroy bacteria.
What is the difference between a rubor and a tumor?
Rubor (redness) due to capillary dilation resulting increased blood flow. Tumor (swelling) due to passage of plasma from the blood stream to the damaged site. Calor (heat) due to capillary dilation resulting increased blood flow.
What causes inflammation to occur?
Acute inflammation starts after a specific injury that will cause soluble mediators like cytokines, acute phase proteins, and chemokines to promote the migration of neutrophils and macrophages to the area of inflammation.[3] These cells are part of natural innate immunity that can take an active role in acute inflammation. If this inflammation does not resolve after six weeks, this will cause the acute inflammation to develop from subacute to the chronic form of inflammation with the migration of T lymphocytes and plasma cells to the site of inflammation. If this persists with no recovery, then tissue damage and fibrosis will ensue. Other varieties of cells, such as macrophages and monocytes, play a role in both acute and chronic inflammation. In this article, we will discuss "acute inflammation."
What are the causes of inflammatory bowel disease?
Polygenic inflammatory bowel disease (IBDs) is characterized by an excessive inflammatory response to gut microbial flora. IBDs include Crohn disease (CD) and ulcerative colitis (UC). These two diseases are cytokine driven. Apart from that, other causes include non-infectious inflammation of the bowel. The system can recognize the microbial agent through the TLRs. These PAMPs that bind to the TLRs (mainly TLR4) activate the signaling pathways (NF-kB, MAPK) that cause the production of cytokines and chemokines to start the resistance to the infection. [19]
What are mediators in the inflammatory process?
The first group of mediators is the toll-like receptors (TLRs), which are membrane-spanning proteins found on the surfaces of the innate immune system cells like macrophages and dendritic cells. These single-pass membrane-spanning receptors recognize the pathogen-associated molecular patterns (PAMPs) or can recognize endogenous signals activated during tissue or cell damage known as danger-associated molecular patterns (DAMPS). To date, research has identified more than ten TLRs. An important example is the CD14 (cluster of differentiation 14), a co-receptor for TLR4, which is present on the surface of innate immune system cells preferentially expressed in macrophages, monocytes, and neutrophils. TLR4 can recognize the Lipopolysaccharide, which is the major component of the outer membrane of the gram-negative bacteria (PAMPs). Then the transmission of PAMPs and DAMPs are mediated by MyD88 (myeloid differentiation 88) along with the TLRs. Subsequently, the signaling will transmit through a specific cascade that leads to nuclear translocation of transcription factors, such as NF-kB, activator protein-1 (AP-1), or interferon regulatory factor 3(IRF3). [7][8][9]
What is the most common cause of death in the world?
Cardiovascular diseases, including atherosclerosis, are recognized as the most common cause of death worldwide. During the formation of atherosclerosis, the inflammatory mediators play a principal role in the initial cell recruitment until the rupture of the plaque. Cardiac stress, due to any reason, will first appear as inflammation. In affected cardiac tissues, there are elevated levels of inflammatory chemokines and cytokines synthesis and release. In cardiac injury, the most immediate defense mechanism against any cardiac tissue damage is innate immunity. Coronary atherosclerosis is the most common cause of myocardial infarction that results in cardiac tissue loss. In myocardial infarction, as the cardiac cells die and become necrotic, the inflammatory cells would start to come to the site of the necrotic tissue to clear the dead cells and debris. Cell death is the inducer that triggers the acute inflammation process resulting in the release of endogenous signals recognized as a danger signal. Subsequently, the TLRs-mediated pathways trigger inflammatory responses by activating the NF-kB pathway. Next, the chemokines recruit the leukocytes to the areas of the infarct, and the cytokines allow the adhesion between leukocytes and endothelial cells. TGF-B and IL-10 promote cardiac repair by suppressing inflammation. [7]
What are the two groups of inflammatory inducers?
As an alternative, we could also divide the inflammatory inducers into two large groups, which are the infectious factors and the non-infectious factors.
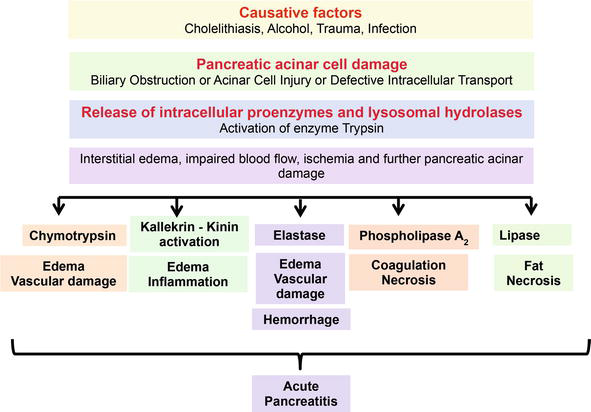
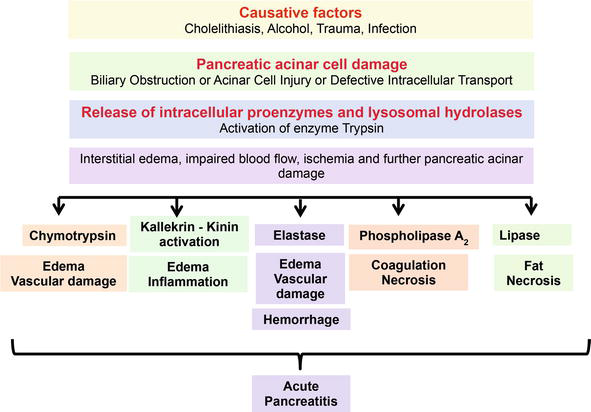
What causes acute pancreatitis?
Acute pancreatitis is an inflammatory disease of the pancreas caused by either pancreatic duct obstruction, gene mutation, or alcoholism. Acute pancreatitis is among the most common causes of hospitalization in the United States. Inflammation in acute pancreatitis occurs by activation of neutrophils and granulocytes, which secrete inflammatory cytokines. NF-kB, JAK-STAT, and MAPK pathways play an important role in cell activation during pancreatitis. [17]
What are the signs of inflammation?
This mechanism is non-specific and immediate.[1] There are five fundamental signs of inflammation that include: heat (calor), redness (rubor), swelling (tumor), pain (dolor), and loss of function (functio laesa). Inflammation can divide into three types based on the time of the process that responds to the injurious cause; acute which occurs immediately after injury and lasts for few days, chronic inflammation that may last for months or even years when acute inflammation fails to settle, and subacute which is a transformational period from acute to chronic which lasts from 2 to 6 weeks.[2]
What happens when an intruder is destroyed?from biologyexams4u.com
Inflammation if localised to the site of infection or injury. Once intruder is destroyed, inflammation settles down. 3. This lead to increased capillary permeability and blood flow to the area. 4. Margination followed by migration of phagocytes to the site of infection.
Why does my swollen area feel sore?from study.com
Of course, as blood vessels dilate and become leaky to allow cells out, a lot of fluid leaks out too, causing redness and swelling. As the swelling increases, the area becomes more and more painful as neighboring tissues are squeezed, triggering pain and pressure receptors.
What is inflammation in the body?from study.com
Inflammation is a nonspecific immune response that helps your body fight infections and heal tissue damage. It is part of the innate immune system because it does not respond to a specific pathogen but is instead a response to any infection or injury. When tissues are damaged, inflammatory molecules called cytokines are released to initiate the inflammatory response. This causes the classic symptoms of inflammation: pain, redness, swelling, and heat.
What is the inflammatory process that occurs when a cell is damaged by an infection?from study.com
When tissues are damaged by infection or injury, they release inflammatory molecules called cytokines. Cytokines are a very important part of the inflammatory process, and they have several effects on the cells around them.
What causes tissue damage?from biologyexams4u.com
1.Tissue damage caused by bacterial infection or injury. 2.Release of vasodilators and chemotactic factors like histamine. 3. This lead to increased capillary permeability and blood flow to the area. 4. Margination followed by migration of phagocytes to the site of infection. 5.The serum proteins along with phagocytes destroy bacteria.
What are the Latin words for inflammation?from study.com
By now, you would be experiencing all of the classic symptoms of inflammation, as denoted by their Latin words and their meanings: calor (heat), dolor (pain), rubor (redness), and tumor (swelling).
What is the process of inflammation?from study.com
What triggers inflammation in your body? The inflammatory process is part of the innate immune system, which means that it is non specific and responds to many types of potential threats. Any damage to your tissues can trigger inflammation.
How do fibroblasts help heal wounds?
Then, reepithelialization starts to occur with the migration of cells from the wound periphery and adjacent edges. Initially, only a thin superficial layer of epithelial cells is laid down, but a thicker and more durable layer of cells will bridge the wound over time. Next, neovascularization occurs through both angiogenesis, forming new blood vessels from existing vessels, and vasculogenesis, which is the formation of new vessels from endothelial progenitor cells (EPCs). Once collagen fibers have been laid down on the fibrin framework, the wound starts to mature. The wound also begins to contract and is facilitated by continued deposition of fibroblasts and myofibroblasts.
What is wound healing?
Wound healing is a natural physiological reaction to tissue injury. However, wound healing is not a simple phenomenon but involves a complex interplay between numerous cell types, cytokines, mediators, and the vascular system.
Why do wound dressings need to be moist?
Wound dressings should create a moist environment to prevent wound desiccation but allows for absorption of additional exudate. In addition, it should allow for airflow, prevent particulate contamination, and be impermeable to bacteria or microbiota.
What is the maturation and remodeling phase of a wound?
The maturation and remodeling phase is where the wound achieves maximum strength as it matures. [3]
How does neovascularization occur?
Next, neovascularization occurs through both angiogenesis, forming new blood vessels from existing vessels, and vasculogenesis, which is the formation of new vessels from endothelial progenitor cells (EPCs). Once collagen fibers have been laid down on the fibrin framework, the wound starts to mature.
What is the inflammatory phase of a wound?
[1] The inflammatory phase is characterized by hemostasis, chemotaxis, and increased vascular permeability, limiting further damage, closing the wound, removing cellular debris and bacteria, and fostering cellular migration.
What is NCBI bookshelf?
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.